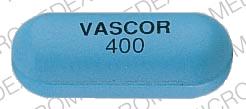
Vascor Disease Interactions
There are 8 disease interactions with Vascor (bepridil).
- Agranulocytosis
- Arrhythmias
- CHF
- Electrolyte imbalance/hypokalemia
- MI
- Bradyarrhythmia/AV block
- Cardiogenic shock/hypotension
- Liver disease
Bepridil (applies to Vascor) agranulocytosis
Major Potential Hazard, Low plausibility. Applicable conditions: Neutropenia
According to the manufacturer, there have been two cases of marked leukopenia and neutropenia reported in U.S. clinical trials of over 800 patients treated with bepridil for up to five years. Both involved diabetic and elderly patients, with one case resulting in death and the other recovering after discontinuation of the drug. In a postmarketing report, a 72-year-old man with severe angina pectoris developed fever and chills associated with an absolute neutrophil count of 35/mm3 six weeks after switching from diltiazem and nitrates to bepridil and nitrates. A bone marrow biopsy revealed profound myeloid hypoplasia. The patient recovered after discontinuation of bepridil and institution of granulocyte colony-stimulating factor and broad-spectrum antibiotics. Therapy with bepridil should be administered cautiously in patients with preexisting neutropenia or agranulocytosis. The drug should be withdrawn promptly if these conditions develop during therapy.
Bepridil (applies to Vascor) arrhythmias
Major Potential Hazard, High plausibility. Applicable conditions: Abnormal Electrocardiogram, Tachyarrhythmia
The use of bepridil is contraindicated in patients with a history of serious ventricular arrhythmias; patients with congenital or acquired QT interval prolongation syndromes; and patients treated concomitantly with class IA or III antiarrhythmic drugs or other medications that are known to produce increases in the QT interval or cause torsade de pointes. Bepridil has class I antiarrhythmic properties and can induce new arrhythmias, including ventricular tachycardia and ventricular fibrillation. Patients with other severe arrhythmias may have increased susceptibility to the proarrhythmic effects of bepridil, but use in such patients has been limited. Bepridil can also cause torsade de pointes type ventricular tachycardia secondary to its ability to prolong the QT interval. In U.S. clinical trials, the mean prolongations of QTc and QT were 8% and 10%, respectively, but increases of 25% or more occurred in 5% of the studied population for QTc and 8.7% for QT. Although the absolute safe upper limit of QT is not known, the manufacturer recommends that the dosage be reduced in patients whose QT interval exceeds 0.52 seconds during treatment. If prolongation remains excessive, the drug should be discontinued.
Bepridil (applies to Vascor) CHF
Major Potential Hazard, High plausibility. Applicable conditions: Myocardial Infarction, Congestive Heart Failure
Bepridil may have a negative inotropic effect, particularly at high dosages. Congestive heart failure has been observed infrequently (approximately 1%) in U.S. controlled clinical trials. However, experience with the use of bepridil in the presence of significantly impaired ventricular function is limited, and there is little information on the effect of concomitant administration with digoxin. Therapy with bepridil should be administered cautiously in patients with congestive heart failure, especially if they have severe left ventricular dysfunction (e.g., ejection fraction < 30%) or if they are receiving a beta-adrenergic blocker. Likewise, bepridil should not be given to patients with acute myocardial infarction and pulmonary congestion documented by X-ray on admission, since associated heart failure may be acutely worsened. Mild symptoms of cardiac failure should be under control, if possible, prior to initiating bepridil therapy.
Bepridil (applies to Vascor) electrolyte imbalance/hypokalemia
Major Potential Hazard, High plausibility. Applicable conditions: Electrolyte Abnormalities, Magnesium Imbalance, Diarrhea
Bepridil can cause torsade de pointes type ventricular tachycardia secondary to its ability to prolong the QT interval. In U.S. clinical trials, the mean prolongations of QTc and QT were 8% and 10%, respectively, but increases of 25% or more occurred in 5% of the studied population for QTc and 8.7% for QT. Electrolyte disturbances such as hypokalemia and hypomagnesemia may augment the prolongation effect of bepridil on the QT interval and should be corrected prior to institution of bepridil therapy. In addition, patients who experience frequent, severe, and/or prolonged diarrhea may be subject to electrolyte losses and should be followed closely and managed accordingly during therapy with bepridil.
Bepridil (applies to Vascor) MI
Major Potential Hazard, High plausibility. Applicable conditions: Myocardial Infarction, Post MI Syndrome, History - Myocardial Infarction
Bepridil has class I antiarrhythmic properties and can induce new arrhythmias, including ventricular tachycardia and ventricular fibrillation. In the National Heart, Lung, and Blood Institute's Cardiac Arrhythmia Suppression Trial involving patients with asymptomatic, non-life-threatening ventricular arrhythmias who have had myocardial infarctions for less than two years previously, an excess rate of mortality/nonfatal cardiac arrest was seen in patients treated with the class I antiarrhythmic agents, encainide and flecainide, compared with that seen in patients assigned to matched placebo-treated groups. Although the applicability of these results to other antiarrhythmic agents is uncertain, the manufacturer recommends generally avoiding the use of bepridil in the post-infarction period. There is also limited experience in the use of bepridil within three months following a myocardial infarction, since it was one of the exclusion criteria in U.S. clinical trials.
CCBs (applies to Vascor) bradyarrhythmia/AV block
Major Potential Hazard, High plausibility. Applicable conditions: Heart Block, Sinus Node Dysfunction
The use of some calcium channel blockers (CCBs) is contraindicated in patients with severe bradyarrhythmia, sick sinus syndrome (unless a functioning pacemaker is present), or heart block greater than the first degree (unless a functioning pacemaker is present). CCBs like bepridil, diltiazem and verapamil have a negative effect on AV conduction and the SA node and may exacerbate these conditions.
CCBs (applies to Vascor) cardiogenic shock/hypotension
Major Potential Hazard, High plausibility.
In general, calcium channel blockers (CCBs) should not be used in patients with hypotension (systolic pressure < 90 mm Hg) or cardiogenic shock. Due to potential negative inotropic and peripheral vasodilating effects, the use of CCBs may further depress cardiac output and blood pressure, which can be detrimental in these patients. The use of verapamil and diltiazem is specifically contraindicated under these circumstances.
CCBs (applies to Vascor) liver disease
Major Potential Hazard, High plausibility.
Calcium channel blockers (CCBs) are extensively metabolized by the liver. The half-lives of CCBs may be prolonged substantially in patients with severe hepatic impairment, with the potential for significant drug accumulation. In addition, the use of some CCBs has been associated with elevations in serum transaminases, both with and without concomitant elevations in alkaline phosphatase and bilirubin. While these effects may be transient and reversible, some patients have developed cholestasis or hepatocellular injury. Therapy with CCBs should be administered cautiously and often at reduced dosages in patients with significantly impaired hepatic function. Periodic monitoring of liver function is advised.
Switch to professional interaction data
Vascor drug interactions
There are 582 drug interactions with Vascor (bepridil).
Vascor alcohol/food interactions
There are 3 alcohol/food interactions with Vascor (bepridil).
More about Vascor (bepridil)
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: calcium channel blockers
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.