Demerol (Oral)
Generic name: meperidine [ me-PER-i-deen ]
Other brand names of meperidine include: Demerol, Meperitab
Drug class: Opioids (narcotic analgesics)
Medically reviewed by Drugs.com. Last updated on Apr 28, 2025.
Ensure accuracy when prescribing, dispensing, and administering meperidine hydrochloride oral solution. Dosing errors due to confusion between mg and mL, and other meperidine hydrochloride oral solutions of different concentrations can result in accidental overdose and death. Meperidine hydrochloride has the potential for addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk before prescribing, and monitor for development of these behaviors or conditions. To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. Accidental ingestion of meperidine hydrochloride, especially in children, can result in fatal overdose of meperidine hydrochloride. Prolonged use of meperidine hydrochloride during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. Concomitant use or discontinuation of concomitantly used cytochrome P450 3A4 inhibitors may effect meperidine plasma concentrations and lead to fatal respiratory depression, profound sedation, opioid toxicity, and/or opioid withdrawal. Careful monitoring of patients should occur when meperidine and cytochrome P450 3A4 inhibitors are concurrently used. Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for patients with inadequate alternative treatment options. Limit dosages and durations to the minimum required and follow patients for signs and symptoms of respiratory depression and sedation. Concomitant use of meperidine hydrochloride with MAOIs or use of MAOIs within the last 14 days is contraindicated and can lead to coma, severe respiratory depression, cyanosis, and hypotension .
Uses for Demerol
Meperidine is used to relieve pain severe enough to require opioid treatment and when other pain medicines did not work well enough or cannot be tolerated. It belongs to the group of medicines called narcotic analgesics (pain medicines). Meperidine acts on the central nervous system (CNS) to relieve pain. This medicine should not be used to relieve chronic (long-lasting or recurrent) pain.
When meperidine is used for a long time, it may become habit-forming, causing mental or physical dependence. However, people who have continuing pain should not let the fear of dependence keep them from using narcotics to relieve their pain. Mental dependence (addiction) is not likely to occur when narcotics are used for this purpose. Physical dependence may lead to withdrawal side effects if treatment is stopped suddenly. However, severe withdrawal side effects can usually be prevented by gradually reducing the dose over a period of time before treatment is stopped completely.
This medicine is available only under a restricted distribution program called the Opioid Analgesic REMS (Risk Evaluation and Mitigation Strategy) program.
Before using Demerol
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies have not been performed on the relationship of age to the effects of meperidine in the pediatric population. Safety and efficacy have not been established.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of meperidine in the elderly. However, elderly patients are more likely to have age-related kidney, liver, or lung problems, which may require caution and an adjustment in the dose for patients receiving meperidine.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Furazolidone
- Iproniazid
- Isocarboxazid
- Linezolid
- Methylene Blue
- Moclobemide
- Nalmefene
- Naltrexone
- Nialamide
- Phenelzine
- Procarbazine
- Rasagiline
- Safinamide
- Samidorphan
- Selegiline
- Toloxatone
- Tranylcypromine
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acepromazine
- Alfentanil
- Almotriptan
- Alprazolam
- Amifampridine
- Amineptine
- Amiodarone
- Amitriptyline
- Amitriptylinoxide
- Amobarbital
- Amoxapine
- Amphetamine
- Amprenavir
- Anileridine
- Aprepitant
- Aripiprazole
- Armodafinil
- Asenapine
- Atazanavir
- Baclofen
- Benperidol
- Benzhydrocodone
- Benzphetamine
- Boceprevir
- Bosentan
- Bromazepam
- Bromopride
- Brompheniramine
- Buprenorphine
- Bupropion
- Buspirone
- Butabarbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Cannabis
- Carbamazepine
- Carbinoxamine
- Carisoprodol
- Carphenazine
- Cetirizine
- Chloral Hydrate
- Chlordiazepoxide
- Chlorpheniramine
- Chlorpromazine
- Chlorzoxazone
- Cimetidine
- Ciprofloxacin
- Citalopram
- Clarithromycin
- Clobazam
- Clomipramine
- Clonazepam
- Clopidogrel
- Clorazepate
- Clozapine
- Cobicistat
- Cocaine
- Codeine
- Conivaptan
- Crizotinib
- Cyclobenzaprine
- Cyclosporine
- Daridorexant
- Darunavir
- Delavirdine
- Desipramine
- Desmopressin
- Desvenlafaxine
- Dexamethasone
- Dexmedetomidine
- Dextroamphetamine
- Dextromethorphan
- Dezocine
- Diazepam
- Dibenzepin
- Dichloralphenazone
- Difenoxin
- Dihydrocodeine
- Diltiazem
- Diphenhydramine
- Diphenoxylate
- Dixyrazine
- Dolasetron
- Donepezil
- Doxepin
- Doxylamine
- Dronedarone
- Droperidol
- Duloxetine
- Efavirenz
- Eletriptan
- Enflurane
- Enzalutamide
- Erythromycin
- Escitalopram
- Esketamine
- Eslicarbazepine Acetate
- Estazolam
- Eszopiclone
- Ethchlorvynol
- Ethopropazine
- Ethylmorphine
- Etravirine
- Fenfluramine
- Fentanyl
- Flibanserin
- Fluconazole
- Fluoxetine
- Fluphenazine
- Flurazepam
- Fluspirilene
- Fluvoxamine
- Fosamprenavir
- Fosaprepitant
- Fosphenytoin
- Fospropofol
- Frovatriptan
- Gabapentin
- Gabapentin Enacarbil
- Gepirone
- Granisetron
- Halazepam
- Haloperidol
- Halothane
- Hexobarbital
- Hydrocodone
- Hydromorphone
- Hydroxyamphetamine
- Hydroxytryptophan
- Hydroxyzine
- Idelalisib
- Imatinib
- Imipramine
- Indinavir
- Isoflurane
- Itraconazole
- Ivacaftor
- Ketamine
- Ketazolam
- Ketobemidone
- Ketoconazole
- Lacosamide
- Lasmiditan
- Lemborexant
- Levocetirizine
- Levomilnacipran
- Levorphanol
- Lisdexamfetamine
- Lithium
- Lofepramine
- Lofexidine
- Lomitapide
- Lopinavir
- Lorazepam
- Lorcaserin
- Loxapine
- Lumacaftor
- Magnesium Oxybate
- Meclizine
- Melitracen
- Melperone
- Mephobarbital
- Meprobamate
- Meptazinol
- Mesoridazine
- Metaxalone
- Methadone
- Methamphetamine
- Methocarbamol
- Methohexital
- Methotrimeprazine
- Metopimazine
- Mibefradil
- Midazolam
- Mifepristone
- Milnacipran
- Mirtazapine
- Mitotane
- Modafinil
- Molindone
- Moricizine
- Morphine
- Morphine Sulfate Liposome
- Nafcillin
- Nalbuphine
- Naratriptan
- Nefazodone
- Nelfinavir
- Nevirapine
- Nicomorphine
- Nilotinib
- Nirmatrelvir
- Nitrazepam
- Nitrous Oxide
- Nortriptyline
- Olanzapine
- Ondansetron
- Opipramol
- Opium
- Opium Alkaloids
- Orphenadrine
- Oxazepam
- Oxcarbazepine
- Oxycodone
- Oxymorphone
- Ozanimod
- Palbociclib
- Palonosetron
- Papaveretum
- Paregoric
- Paroxetine
- Pentazocine
- Pentobarbital
- Perampanel
- Perazine
- Periciazine
- Perphenazine
- Phenobarbital
- Phenytoin
- Pimozide
- Piperacetazine
- Pipotiazine
- Piritramide
- Posaconazole
- Potassium Oxybate
- Prazepam
- Prednisone
- Pregabalin
- Primidone
- Prochlorperazine
- Promazine
- Promethazine
- Propiomazine
- Propofol
- Protriptyline
- Quazepam
- Quetiapine
- Ramelteon
- Ranitidine
- Ranolazine
- Remifentanil
- Remimazolam
- Remoxipride
- Rifabutin
- Rifampin
- Rifapentine
- Rizatriptan
- Ropeginterferon Alfa-2b-njft
- Saquinavir
- Scopolamine
- Secobarbital
- Sertindole
- Sertraline
- Sibutramine
- Sodium Oxybate
- St John's Wort
- Sufentanil
- Sulpiride
- Sumatriptan
- Suvorexant
- Tapentadol
- Telaprevir
- Telithromycin
- Temazepam
- Thiethylperazine
- Thiopental
- Thiopropazate
- Thioproperazine
- Thioridazine
- Tianeptine
- Tilidine
- Tizanidine
- Tolonium Chloride
- Topiramate
- Tramadol
- Trazodone
- Triazolam
- Trifluoperazine
- Trifluperidol
- Triflupromazine
- Trimeprazine
- Trimipramine
- Tryptophan
- Venlafaxine
- Verapamil
- Vilazodone
- Voriconazole
- Vortioxetine
- Zaleplon
- Ziprasidone
- Zolmitriptan
- Zolpidem
- Zopiclone
- Zotepine
- Zuranolone
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Isoniazid
- Ritonavir
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Grapefruit Juice
Using this medicine with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Addison disease (adrenal gland problem) or
- Alcohol abuse, or history of or
- Brain problems (including tumors or increased intracranial pressure) or
- Breathing or lung problems (eg, COPD, hypoxia, sleep apnea) or
- Central nervous system (CNS) depression or
- Cor pulmonale (serious heart condition) or
- Drug dependence, especially with narcotics, or history of or
- Enlarged prostate or
- Gallbladder disease or
- Head injuries, history of or
- Hypothyroidism (an underactive thyroid) or
- Kyphoscoliosis (severe curvature of the spine with breathing problems) or
- Mental illness, history of or
- Pancreatitis (swelling of the pancreas) or
- Pheochromocytoma (adrenal gland tumor) or
- Sickle cell anemia (inherited blood disorder) or
- Weakened physical condition—Use with caution. May increase risk for more serious side effects.
- Heart rhythm problems (eg, atrial flutter, tachycardia) or
- Hypotension (low blood pressure) or
- Hypovolemia (low blood volume) or
- Seizures, history of—Use with caution. May make these conditions worse.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
- Lung or breathing problems (eg, asthma, respiratory depression), severe or
- Stomach or bowel blockage (eg, paralytic ileus)—Should not be used in patients with these conditions.
Proper use of Demerol
Take this medicine only as directed by your doctor. Do not take more of it, do not take it more often, and do not take it for a longer time than your doctor ordered. This is especially important for elderly patients, who may be more sensitive to the effects of pain medicines. If too much of this medicine is taken for a long time, it may become habit-forming (causing mental or physical dependence).
It is very important that you understand the rules of the Opioid Analgesic REMS program to prevent addiction, abuse, and misuse of meperidine. This medicine should come with a Medication Guide. Read and follow these instructions carefully. Read it again each time you refill your prescription in case there is new information. Ask your doctor if you have any questions.
Measure the oral liquid with a marked measuring spoon, oral syringe, or medicine cup. Never use an average household teaspoon or tablespoon to measure the dose of this medicine.
Mix each dose of the liquid into a one-half glass of water and drink all of the mixture in order to get the correct amount of medicine. This may help lessen the numbing effects of the oral liquid.
Swallow the tablet whole. Do not crush, break, or chew it.
Drink plenty of fluids to help avoid constipation during treatment with this medicine.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For oral dosage forms (solution or tablets):
- For moderate to severe pain:
- Adults—50 to 150 milligrams (mg) every 3 or 4 hours as needed.
- Children 1 year of age and older—Dose is based on body weight and must be determined by your doctor. The dose is usually 1.1 to 1.8 milligrams (mg) per kilogram (kg) of body weight per dose given every 3 or 4 hours as needed.
- Children younger than 1 year of age—Use and dose must be determined by your doctor.
- For moderate to severe pain:
Missed Dose
If you miss a dose of this medicine, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Meperidine can cause serious unwanted effects if taken by adults who are not used to strong narcotic pain medicines. Make sure you store the medicine in a safe and secure place to prevent others from getting it.
Drop off any unused narcotic medicine at a drug take-back location right away. If you do not have a drug take-back location near you, flush any unused narcotic medicine down the toilet. Check your local drug store and clinics for take-back locations. You can also check the DEA web site for locations. Here is the link to the FDA safe disposal of medicines website: www.fda.gov/drugs/resourcesforyou/consumers/buyingusingmedicinesafely/ensuringsafeuseofmedicine/safedisposalofmedicines/ucm186187.htm
Precautions while using Demerol
It is very important that your doctor check your progress while you are using this medicine, especially within the first 24 to 72 hours of treatment. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to use it. Blood and urine tests may be needed to check for unwanted effects.
Do not use this medicine with a monoamine oxidase (MAO) inhibitor (eg, isocarboxazid [Marplan®], linezolid [Zyvox®], phenelzine [Nardil®], selegiline [Eldepryl®], tranylcypromine [Parnate®]). Do not start taking meperidine during the 2 weeks after you stop an MAO inhibitor. Wait for 2 weeks after stopping meperidine before you start taking an MAO inhibitor. If you take them together or do not wait 2 weeks, you may have confusion, agitation, restlessness, stomach or bowel symptoms, a sudden high body temperature, an extremely high blood pressure, or severe convulsions.
Using too much meperidine may cause an overdose. Symptoms of an overdose include: extreme dizziness or weakness, trouble breathing, slow heartbeat or breathing, seizures, or cold, clammy skin. In case of an overdose, call your doctor right away. Your doctor may also give naloxone to treat an overdose.
Check with your doctor before using this medicine with alcohol or other medicines that affect the central nervous system (CNS). The use of alcohol or other medicines that affect the CNS with meperidine may worsen the side effects of this medicine, such as dizziness, poor concentration, drowsiness, unusual dreams, and trouble with sleeping. Some examples of medicines that affect the CNS are antihistamines or medicine for allergies or colds, sedatives, tranquilizers or sleeping medicines, medicine for depression, medicine for anxiety, prescription pain medicine or narcotics, medicine for attention deficit and hyperactivity disorder, medicine for seizures or barbiturates, muscle relaxants, or anesthetics, including some dental anesthetics.
This medicine may cause sleep-related breathing problems (eg, sleep apnea, sleep-related hypoxemia). Your doctor may decrease your dose if you have sleep apnea (stop breathing for short periods during sleep) while using this medicine.
This medicine may be habit-forming. If you feel that the medicine is not working as well, do not use more than your prescribed dose. Call your doctor for instructions.
Using narcotics for a long time can cause severe constipation. To prevent this, your doctor may direct you to take laxatives, drink lots of fluids, or increase the amount of fiber in your diet. Be sure to follow these directions carefully, because continuing constipation can lead to more serious problems.
This medicine may cause adrenal gland problems. Check with your doctor right away if you have darkening of the skin, diarrhea, dizziness, fainting, loss of appetite, mental depression, nausea, skin rash, unusual tiredness or weakness, or vomiting.
Dizziness, lightheadedness, or fainting may occur, especially when you get up suddenly from a lying or sitting position. Getting up slowly may help. Also, lying down for a while may relieve the dizziness or lightheadedness. If this problem continues or gets worse, check with your doctor.
Check with your doctor right away if you have anxiety, restlessness, a fast heartbeat, fever, sweating, muscle spasms, twitching, nausea, vomiting, diarrhea, or see or hear things that are not there. These may be symptoms of a serious condition called serotonin syndrome. Your risk may be higher if you also take certain other medicines that affect serotonin levels in your body.
This medicine may make you dizzy, drowsy, confused, or disoriented. Do not drive or do anything else that could be dangerous until you know how this medicine affects you.
Before having any kind of surgery (including dental surgery) or emergency treatment, tell the medical doctor or dentist in charge that you are using this medicine. Serious unwanted effects can occur if certain medicines are given together with meperidine.
Do not stop using this medicine without checking first with your doctor. Your doctor may want you to gradually reduce the amount you are using before stopping it completely. This is to decrease the chance of having certain side effects when you stop the medicine, including agitation, anxiety, dizziness, a feeling of constant movement of self or surroundings, headaches, increased sweating, nausea, trembling or shaking, trouble sleeping or walking, or unusual tiredness.
Using this medicine while you are pregnant may cause serious unwanted effects, including neonatal opioid withdrawal syndrome in your newborn baby. Tell your doctor right away if you think you are pregnant or if you plan to become pregnant while using this medicine.
For nursing mothers:
- Talk to your doctor if you have any questions about taking meperidine or about how this medicine may affect your baby.
- Call your doctor if you become extremely tired and have difficulty caring for your baby.
- Your baby should generally nurse every 2 to 3 hours and should not sleep for more than 4 hours at a time.
- Check with your doctor or hospital emergency room immediately if your baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, difficulty breathing, or limpness. These may be symptoms of an overdose and need immediate medical attention.
Using too much of this medicine may cause infertility (unable to have children). Talk with your doctor before using this medicine if you plan to have children.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal (eg, St. John's wort) or vitamin supplements.
Side Effects of Demerol
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
Incidence not known
- Agitation
- blurred vision
- chest pain or discomfort
- cold, clammy skin
- confusion
- cough
- darkening of the skin
- decrease in the frequency of urination
- decrease in urine volume
- diarrhea
- difficult or trouble breathing
- difficulty in passing urine (dribbling)
- difficulty with swallowing
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fast, slow, pounding, or irregular heartbeat
- feeling of warmth
- fever
- hives, itching, or skin rash
- irregular, fast, slow, or shallow breathing
- lightheadedness, dizziness, or fainting
- loss of appetite
- mental depression
- muscle twitching or jerking
- nausea
- overactive reflexes
- painful urination
- pale or blue lips, fingernails, or skin
- poor coordination
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- redness of the face, neck, arms, and occasionally, upper chest
- restlessness
- rhythmic movement of the muscles
- seizures
- shakiness in the legs, arms, hands, or feet
- shivering
- sweating
- talking or acting with excitement you cannot control
- tightness in the chest
- trembling or shaking of the hands or feet
- twitching
- unusual tiredness or weakness
- upper abdominal or stomach pain
- vomiting
Get emergency help immediately if any of the following symptoms of overdose occur:
Symptoms of overdose
- Bluish color of the fingernails, lips, skin, palms, or nail beds
- change in consciousness
- decreased awareness or responsiveness
- loss of consciousness
- severe sleepiness
- sleepiness or unusual drowsiness
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Drowsiness
- relaxed and calm feeling
Incidence not known
- Blurred or loss of vision
- confusion about identity, place, and time
- deep or fast breathing with dizziness
- difficulty having a bowel movement
- disturbed color perception
- double vision
- dry mouth
- false or unusual sense of well-being
- halos around lights
- headache
- irritability
- nervousness
- night blindness
- numbness of the feet, hands, and around the mouth
- overbright appearance of lights
- redness of the skin
- seeing, hearing, or feeling things that are not there
- trouble sleeping
- tunnel vision
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Commonly used brand name(s)
In the U.S.
- Demerol
- Meperitab
Available Dosage Forms:
- Syrup
- Tablet
- Solution
Therapeutic Class: Analgesic
Chemical Class: Opioid
Frequently asked questions
More about Demerol (meperidine)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (76)
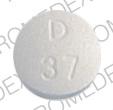
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- Drug class: Opioids (narcotic analgesics)
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.