Juvenile Arthritis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Juvenile arthritis is a long-term autoimmune disease that causes pain and inflammation in one or more joints. Juvenile arthritis develops when the immune system attacks the tissues in the joints. Your child may have symptoms for only a few months, or for the rest of his or her life. Your child may have periods of remission (no signs or symptoms). Your child may have any of 6 subtypes of juvenile arthritis. Ask his or her healthcare provider for more information about the type he or she has.
DISCHARGE INSTRUCTIONS:
Return to the emergency department if:
- Your child has severe eye pain or vision changes.
- Your child's pain becomes worse.
- Your child has severe redness, swelling, or pain in one of his or her joints.
Call your child's doctor or rheumatologist if:
- Your child has a fever.
- Your child has problems eating or you feel he or she is not eating enough.
- Your child begins to lose weight, thinks more slowly, or seems sad most of the time.
- Your child has a severe headache or pain around his or her eyes.
- You have questions or concerns about your child's condition or care.
Medicines:
Your child may need any of the following:
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Disease-modifying rheumatoid arthritis drugs (DMARDs) help prevent joint damage, slow the progression of juvenile arthritis, and reduce pain, stiffness, and inflammation. DMARDs can take time to start working. Your child may also need to take other medicines to control his or her symptoms until the DMARDs start to work.
- Steroid medicine helps decrease severe inflammation. These are usually given for a short time while other medicines are started that can take longer to be effective.
- Biologic therapy includes medicines used to help decrease joint swelling, pain, and stiffness. These medicines can increase the risk for serious infections. Your child's health will need to be monitored while he or she is taking this medicine.
- Do not give aspirin to children younger than 18 years. Your child could develop Reye syndrome if he or she has the flu or a fever and takes aspirin. Reye syndrome can cause life-threatening brain and liver damage. Check your child's medicine labels for aspirin or salicylates.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Help your child manage juvenile arthritis:
- Eye exams are used to check for uveitis (eye inflammation). Have your child's eyes examined regularly. Ask your child's healthcare provider or rheumatologist for more information about eye checks and how often your child should have them.
- A physical therapist can teach your child exercises to help improve movement and strength, and to decrease pain. An occupational therapist can teach him or her skills to help with his or her daily activities.
- Rest is important if your child's joints are painful. Limit his or her activities until his or her symptoms improve. Gradually let him or her start his or her regular activities when he or she can do them without pain. Have him or her avoid motions and activities that cause strain on his or her joints, such as heavy exercise and lifting.
- Ice or heat can help decrease swelling and pain. Ice may also help prevent tissue damage. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel and place it on your child's joint for 15 to 20 minutes every hour as directed. You can also apply heat to his or her joints for 20 minutes every 2 hours. Heat treatment includes hot packs, heat lamps, warm baths, or showers.
- Splints may be given for your child to wear on his or her hands. Splints can help his or her joints rest and decrease inflammation.
- Physical activity can help increase strength and flexibility. Keep your child as active as possible while avoiding things that increase his or her pain. Ask your child's healthcare provider or rheumatologist about the best exercise plan for your child.
Keep a daily record:
Keep a daily record of your child's activities and the severity of his or her symptoms. Write down what activities he or she did, and if his or her symptoms got better or worse. Bring the record with you to follow-up appointments.
Nutrition:
- Offer your child a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask if your child needs to be on a special diet.
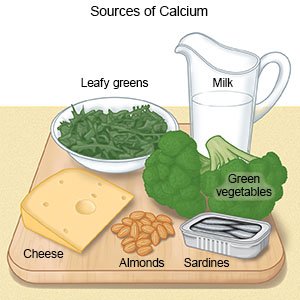
- Give your child foods rich in calcium and vitamin D. These are important for your child's bones while he or she is growing. Foods high in calcium include milk, cheese, broccoli, and tofu. Vitamin D may be found in meat, fish, fortified milk, cereal, and bread. Ask if your child needs extra vitamins and minerals, especially calcium and vitamin D.
Follow up with your child's doctor or rheumatologist as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Juvenile Arthritis
Treatment options
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
