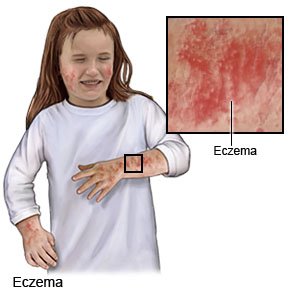
Eczema in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Eczema is an itchy, red, scaly skin rash. Eczema is common in children between the ages of 2 months and 5 years. Your child is more likely to have eczema if he or she also has asthma or allergies. Your child's symptoms may improve as he or she gets older. However, your child may have flare-ups from time to time for the rest of his or her life.
 |
DISCHARGE INSTRUCTIONS:
Return to the emergency department if:
- Your child develops a fever.
- Your child has red streaks going up his or her arm or leg.
- Your child's rash gets more swollen, red, or hot.
Call your child's doctor if:
- Most of your child's skin is red, swollen, painful, and covered with scales.
- Your child develops bloody, painful crusts.
- Your child's skin blisters and oozes white or yellow pus.
- Your child has trouble sleeping because of itching.
- You have questions or concerns about your child's condition or care.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Medicines:
- Medicines may help reduce itching, redness, pain, and swelling. They may be given as an emollient (thick) cream, pill, or injection under the skin. Your child may also receive antibiotics if he or she has a skin infection.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
- Do not give aspirin to children younger than 18 years. Your child could develop Reye syndrome if he or she has the flu or a fever and takes aspirin. Reye syndrome can cause life-threatening brain and liver damage. Check your child's medicine labels for aspirin or salicylates.
Care for your child's skin:
- Pat or press on your child's skin to relieve itching. Remind your child not to scratch. Trim your child's fingernails. Put cotton gloves or mittens on your child's hands while he or she sleeps.
- Keep your child's skin moist. Rub gentle or sensitive skin lotion, cream, or ointment on your child's skin many times throughout the day. Ask your child's healthcare provider what to use and how often to use it. Use moist bandages if directed. Do not use products that contain alcohol, dyes, or fragrances.
- Give your child warm water baths or showers for 10 minutes or less. Use mild soap. Apply moisturizer to your child's skin when it is damp, right after the bath or shower. Teach your child how to gently pat his or her skin dry.
- Choose cotton clothes. Dress your child in loose-fitting clothes made from cotton or cotton blends. Avoid wool, polyester, or other scratchy material.
- Use a humidifier to add moisture to the air in your home.
- Help your child avoid changes in temperature. For example, activities that cause him or her to sweat a lot. Sweat can cause itching. Remove blankets from your child's bed if he or she gets hot while sleeping.
- Avoid allergens, dust, and skin irritants. Use mild soap, shampoo, and detergent. Do not use fabric softener.
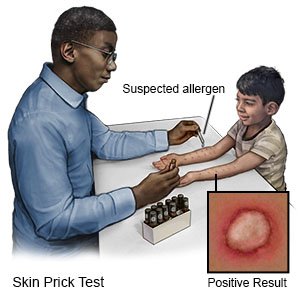
- Ask your child's healthcare provider about allergy testing. Allergy testing may help identify allergens that irritate your child's skin.
Follow up with your child's doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Eczema
Treatment options
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
