Levofloxacin Side Effects
Medically reviewed by Drugs.com. Last updated on May 25, 2024.
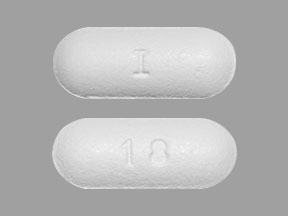
Applies to levofloxacin: oral solution, oral tablet.
Other dosage forms:
Important warnings
This medicine can cause some serious health issues
Oral route (tablet; solution)
Fluoroquinolones, including levofloxacin, are associated with disabling and potentially irreversible serious adverse reactions that have occurred together, including tendinitis and tendon rupture, peripheral neuropathy, and CNS effects.
Discontinue levofloxacin and avoid use of fluoroquinolones in patients with these serious adverse reactions.
Reserve use of levofloxacin for patients with no alternative treatment options for an uncomplicated UTI, acute bacterial exacerbation of chronic bronchitis, or acute bacterial sinusitis.
Fluoroquinolones, including levofloxacin, may exacerbate muscle weakness in persons with myasthenia gravis.
Avoid in patients with known history of myasthenia gravis.
Precautions
It is very important that your doctor check your or your child's progress at regular visits to make sure the medicine is working properly and to decide if you should continue to take it. Blood and urine tests may be needed to check for unwanted effects.
If your or your child's symptoms do not improve within a few days, or if they become worse, check with your doctor.
Levofloxacin may rarely cause inflammation (tendinitis) or tearing of a tendon (the cord that attaches muscles to the bones). This can occur while you are taking the medicine or after you finish using it. The risk of having tendon problems may be increased if you are over 60 years of age, are using steroid medicines (eg, dexamethasone, prednisolone, prednisone, or Medrol®), have severe kidney problems, have a history of tendon problems (eg, rheumatoid arthritis), or have received an organ (eg, heart, kidney, or lung) transplant. Check with your doctor right away if you get sudden pain or swelling in a tendon after exercise (eg, in the ankle, back of the knee or leg, shoulder, elbow, or wrist), bruise more easily after an injury, or are unable to bear weight or move the affected area. Refrain from exercise until your doctor says otherwise.
This medicine may cause serious allergic reactions, including anaphylaxis, which can be life-threatening and require immediate medical attention. Call your doctor right away if you have a rash, itching, hives, hoarseness, lightheadedness or fainting, trouble breathing, trouble swallowing, or any swelling of your hands, face, or mouth after you or your child take this medicine.
Serious side effects can occur during treatment with this medicine. Sometimes serious side effects can occur without warning. However, possible warning signs include: black, tarry stools, blistering, peeling, or loosening of the skin, bloody or cloudy urine, chills, decreased urination, diarrhea, fever, joint or muscle pain including tendon rupture or swelling of the tendon (tendinitis)., red skin lesions, often with a purple center, sores, ulcers, or white spots in the mouth or on the lips, severe stomach pain, skin rash, swelling of the face, fingers, feet, or lower legs, unusual bleeding or bruising, unusual weight gain, or yellow skin or eyes. Check with your doctor immediately if you notice any of these warning signs.
Levofloxacin may lower the number of some types of blood cells in your body. Because of this, you may bleed or get infections more easily. To help with these problems, avoid being near people who are sick or have infections. Wash your hands often. Stay away from rough sports or other situations where you could be bruised, cut, or injured. Brush and floss your teeth gently. Be careful when using sharp objects, including razors and fingernail clippers.
Levofloxacin may cause serious liver problems, including hepatitis. Check with your doctor right away if you or your child start having nausea or vomiting, dark urine, light-colored stools, stomach pain, or yellow eyes or skin while using this medicine.
Levofloxacin may cause diarrhea, and in some cases it can be severe. It may occur 2 months or more after you stop using this medicine. Do not take any medicine to treat diarrhea without first checking with your doctor. Diarrhea medicines may make the diarrhea worse or make it last longer. If you have any questions about this or if mild diarrhea continues or gets worse, check with your doctor.
Tell your doctor right away if you or your child start having numbness, tingling, or burning pain in the hands, arms, legs, or feet including worsening of myasthenia gravis.. These may be symptoms of a condition called peripheral neuropathy.
If you have low blood potassium or an abnormally slow heartbeat, levofloxacin may increase your risk of having a fast, slow, or irregular heartbeat, loss of consciousness, or fainting spells. If these symptoms occur, tell your doctor right away.
Tell your doctor right away if you or your child have any of the following symptoms while using this medicine: convulsions (seizures), feeling anxious, confused, or depressed, seeing, hearing, or feeling things that are not there, severe headache, trouble sleeping, or unusual thoughts or behaviors.
This medicine may increase your risk for aortic aneurysm (bulge in the wall of the largest artery). Check with your doctor right away if you have sudden chest, stomach, or back pain, trouble breathing, cough, or hoarseness.
If you are a diabetic patient using insulin or diabetes medicine by mouth: Levofloxacin may cause hypoglycemia (low blood sugar) in some patients. Symptoms of low blood sugar must be treated before they lead to unconsciousness (passing out). Different people may feel different symptoms of low blood sugar. If you experience symptoms of low blood sugar, check with your doctor right away.
- Symptoms of low blood sugar can include: anxiety, behavior change similar to being drunk, blurred vision, cold sweats, confusion, cool pale skin, difficulty with concentrating, drowsiness, excessive hunger, headache, nausea, nervousness, rapid heartbeat, shakiness, or unusual tiredness or weakness.
Some people who take levofloxacin may become more sensitive to sunlight than they are normally. Exposure to sunlight, even for brief periods of time, may cause severe sunburn or skin rash, redness, itching, or discoloration. When you begin using this medicine:
- Stay out of direct sunlight, especially between the hours of 10 AM and 3 PM, if possible.
- Wear protective clothing, including a hat and sunglasses.
- Apply a sun block product that has a sun protection factor (SPF) of at least 15. Some patients may require a product with a higher SPF number, especially if they have a fair complexion. If you have any questions about this, check with your doctor.
- Do not use a sun lamp or tanning bed or booth.
If you have a severe reaction from the sun, check with your doctor.
Levofloxacin may cause some people to become dizzy, lightheaded, drowsy, or less alert than they are normally. Do not drive or do anything else that could be dangerous until you know how this medicine affects you. If these reactions are especially bothersome, check with your doctor.
Before you have any medical tests, tell the medical doctor in charge that you are using this medicine. The results of some tests may be affected by this medicine.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of levofloxacin
Along with its needed effects, levofloxacin may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking levofloxacin:
More common side effects
- diarrhea
Rare side effects
- agitation
- blisters
- confusion
- diarrhea (watery and severe) which may also be bloody
- feeling that others can hear your thoughts or control your behavior
- fever
- pain, inflammation, or swelling in the calves of the legs, shoulders, or hands, including tendon rupture or swelling of the tendon (tendinitis)
- redness and swelling of the skin
- seeing, hearing, or feeling things that are not there
- sensation of burning on the skin
- severe mood or mental changes
- stomach cramps or pain (severe)
- skin rash, itching, or redness
- trembling
- unusual behavior
Incidence not known
- black, tarry stools
- blurred vision
- burning, numbness, tingling, or painful sensation including peripheral neuropathy.
- cough
- dark urine
- difficulty with breathing
- difficulty with chewing, talking, or swallowing
- drooping eyelids
- fainting
- fast or irregular heartbeat
- general body swelling
- hives
- hoarseness
- joint or muscle pain including tendon rupture or swelling of the tendon (tendinitis).
- muscle cramps, spasms, pain, or stiffness
- peeling or loosening of the skin
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- seizures
- severe dizziness
- severe tiredness
- tightness in the chest
- unsteadiness or awkwardness
- unusual bleeding or bruising
- unusual tiredness or weakness
- vision changes
- voice changes
- weakness in the arms, hands, legs, or feet including worsening of myasthenia gravis.
Other side effects of levofloxacin
Some side effects of levofloxacin may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common side effects
- change in taste
- constipation
- dizziness
- drowsiness
- headache
- lightheadedness
- nausea
- nervousness
- stomach pain or discomfort
- trouble sleeping
- vaginal itching and discharge
- vomiting
Incidence not known
- feeling of warmth or heat
- flushing or redness of the skin, especially on the face and neck
- sweating
See also:
For healthcare professionals
Applies to levofloxacin: compounding powder, intravenous solution, oral solution, oral tablet.
General adverse events
The most frequently reported side effects with the IV and oral formulations included nausea, headache, diarrhea, insomnia, constipation, and dizziness. Therapy was discontinued due to side effects in 4.3% of patients overall (3.8% treated with 250 mg and 500 mg doses; 5.4% treated with 750 mg dose). The most common side effects leading to discontinuation were gastrointestinal (primarily nausea, vomiting), dizziness, and headache.
Cough/productive cough, dysgeusia, and fatigue/asthenia were reported most often with the nebulizer solution formulation.
Very rare cases of prolonged (up to months or years), disabling, and potentially irreversible serious side effects affecting several (sometimes multiple) system organ classes and senses (including reactions such as tendonitis, tendon rupture, arthralgia, pain in extremities, gait disturbance, neuropathies associated with paresthesia, depression, fatigue, memory impairment, sleep disorders, impairment of hearing/vision/taste/smell) have been reported in association with use of quinolones and fluoroquinolones, in some cases irrespective of preexisting risk factors.[Ref]
Respiratory
- Common (1% to 10%): Dyspnea
- Uncommon (0.1% to 1%): Epistaxis
- Frequency not reported: Rhinitis, sinusitis, pharyngitis, bronchitis, chronic obstructive airway disease, laryngitis, pleurisy, pneumonitis, upper respiratory tract infection, asthma, cough, hemoptysis, hiccough, hypoxia, pleural effusion, pulmonary embolism, respiratory insufficiency, airway obstruction, acute respiratory distress syndrome, aspiration, bronchospasm, emphysema, pneumonia, pneumothorax, pulmonary collapse, pulmonary edema, respiratory depression, respiratory disorder
- Postmarketing reports: Allergic pneumonitis (isolated reports), dysphonia
Nebulizer Solution:
- Very common (10% or more): Cough/productive cough (54%), dyspnea, changes in bronchial secretions (volume, viscosity), hemoptysis, decreased forced expiratory volume
- Common (1% to 10%): Dysphonia, decreased pulmonary function test, abnormal breath sounds
- Uncommon (0.1% to 1%): Bronchospasm, bronchial hyper-reactivity, obstructive airways disorder[Ref]
Nervous system
- Common (1% to 10%): Headache, dizziness
- Uncommon (0.1% to 1%): Convulsions, hyperkinesias, hypertonia, paresthesia, somnolence, tremor, vertigo, abnormal gait, syncope, dysgeusia
- Rare (0.01% to 0.1%): Tinnitus
- Frequency not reported: Abnormal coordination, coma, hypoesthesia, dysesthesia, weakness, involuntary muscle contractions, hyperesthesia, paralysis, speech disorder, stupor, encephalopathy, leg cramps, ataxia, migraine, seizures, benign intracranial hypertension, hearing loss, hearing impaired, peripheral sensory neuropathy/sensory axonal polyneuropathy, peripheral sensory motor neuropathy/sensorimotor axonal polyneuropathy, dyskinesia, extrapyramidal disorder, hypoglycemic coma
- Postmarketing reports: Abnormal electroencephalogram (EEG), exacerbation of myasthenia gravis, anosmia, ageusia, parosmia, encephalopathy (isolated reports), pseudotumor cerebri, hypoacusis, peripheral neuropathy (sometimes irreversible)
Nebulizer Solution:
- Very common (10% or more): Dysgeusia (30%)
- Common (1% to 10%): Headache, dizziness, tinnitus
- Uncommon (0.1% to 1%): Hyposmia, somnolence, peripheral neuropathy, hearing loss[Ref]
Cases of sensory or sensorimotor axonal polyneuropathy (affecting small and/or large axons) resulting in paresthesias, hypoesthesias, dysesthesias, and weakness have been reported.
One survey reported 33 cases of peripheral neuropathy associated with this drug, ranging in severity from mild and reversible to severe and persistent. In 1 case, a 51-year-old female developed "electrical" sensations, numbness, allodynia, multiple severe tendinitis, partial tendon rupture, impaired memory, confusion, and impaired concentration, with some symptoms persisting after 1 year.[Ref]
Other
- Common (1% to 10%): Chest pain, edema, moniliasis
- Uncommon (0.1% to 1%): Asthenia, increased alkaline phosphatase, fungal infection (including Candida infection), pathogen resistance
- Rare (0.01% to 0.1%): Pyrexia
- Frequency not reported: Malaise, increased LDH, elevated serum triglycerides, elevated serum cholesterol, rigors, substernal chest pain, ascites, changed temperature sensation, ear disorder (unspecified), enlarged abdomen, hot flashes, gangrene, influenza-like symptoms, leg pain, multiple organ failure, earache, abscess, herpes simplex, bacterial infection, viral infection, otitis media, sepsis, pain (including pain in back, chest, extremities), fatigue, face edema, flushing, aggravated condition
- Postmarketing reports: Multi-organ failure
Nebulizer Solution:
- Very common (10% or more): Fatigue/asthenia (25%), decreased exercise tolerance
- Common (1% to 10%): Pyrexia
- Uncommon (0.1% to 1%): Increased blood alkaline phosphatase[Ref]
Gastrointestinal
- Common (1% to 10%): Nausea, diarrhea, constipation, abdominal pain, dyspepsia, vomiting
- Uncommon (0.1% to 1%): Gastroenteritis, pancreatitis, glossitis, gastritis, esophagitis, flatulence, stomatitis, pseudomembranous/Clostridioides difficile colitis
- Frequency not reported: Dry mouth, dysphagia, gastrointestinal hemorrhage, tongue edema, gastroesophageal reflux, melena, taste perversion, intestinal perforation, intestinal obstruction, C difficile-associated diarrhea, hemorrhagic diarrhea, enterocolitis
Nebulizer Solution:
- Common (1% to 10%): Nausea, vomiting, abdominal pain, diarrhea, constipation
- Uncommon (0.1% to 1%): Retching, dyspepsia, flatulence, oral fungal infection[Ref]
During 1 study, C difficile-associated diarrhea occurred in 11 of 490 study patients (2.2%) receiving this drug.
Hemorrhagic diarrhea has been reported, which in very rare cases was indicative of enterocolitis (including pseudomembranous colitis).[Ref]
Psychiatric
- Common (1% to 10%): Insomnia
- Uncommon (0.1% to 1%): Abnormal dreams, agitation, anxiety, confusional state, nervousness, depression, hallucination, nightmare, sleep disorder
- Rare (0.01% to 0.1%): Psychotic reactions (with hallucination, paranoia)
- Frequency not reported: Aggressive reaction, delirium, emotional lability, impaired concentration, manic reaction, mental deficiency, toxic psychoses, withdrawal syndrome, psychotic disorders/reactions with self-endangering behavior (including suicidal ideation, suicide attempt)
- Postmarketing reports: Psychosis, paranoia, suicide attempt (isolated reports), suicidal ideation (isolated reports), completed suicide (isolated reports)
Nebulizer Solution:
- Common (1% to 10%): Insomnia
- Uncommon (0.1% to 1%): Anxiety, depression[Ref]
Attempted or completed suicide reported, especially in patients with medical history of/underlying risk factor for depression.[Ref]
Dermatologic
- Common (1% to 10%): Rash, pruritus
- Uncommon (0.1% to 1%): Urticaria, hyperhidrosis
- Rare (0.01% to 0.1%): Angioedema, drug reaction with eosinophilia and systemic symptoms (DRESS), fixed drug eruption
- Frequency not reported: Dry skin, skin disorder, skin exfoliation, skin ulceration, erythematous rash, alopecia, maculopapular rash, erythema nodosum, eczema, mucocutaneous reactions
- Postmarketing reports: Photosensitivity/phototoxicity reaction, bullous eruptions (including Stevens-Johnson syndrome, toxic epidermal necrolysis, acute generalized exanthematous pustulosis, fixed drug eruptions, erythema multiforme), leukocytoclastic vasculitis
Nebulizer Solution:
- Common (1% to 10%): Rash
- Uncommon (0.1% to 1%): Urticaria, pruritus[Ref]
Mucocutaneous reactions have been reported, sometimes after the first dose.
A 78-year-old female developed toxic epidermal necrolysis 2 days after parenteral therapy. The rash initially manifested as an erythematous rash, blistering, and mucosal sloughing but progressed to exfoliation involving three-quarters of the patient's body surface area including mucosa. A positive Nikolsky sign was noted.
A 15-year-old male developed fatal toxic epidermal necrolysis taking this drug for 9 days. The rash progressed over 40 hours to involve 80% of his body surface area with a positive Nikolsky sign and involvement of the eyes and oral, nasal, and perianal mucosa.[Ref]
Hepatic
- Common (1% to 10%): Increased hepatic enzymes (ALT/AST, alkaline phosphatase, GGT)
- Uncommon (0.1% to 1%): Abnormal hepatic function, increased blood bilirubin
- Frequency not reported: Acute hepatocellular injury, cholecystitis, cholelithiasis, hepatic coma, hepatic necrosis, bilirubinemia, severe liver injury (including fatal cases with acute liver failure)
- Postmarketing reports: Severe hepatotoxicity (including acute hepatitis and fatal events), hepatic failure (including fatal cases), hepatitis, jaundice
Nebulizer Solution:
- Common (1% to 10%): Increased ALT, increased AST
- Uncommon (0.1% to 1%): Hepatitis, hyperbilirubinemia, abnormal liver function test[Ref]
Severe liver injury (including fatal cases with acute liver failure) has been reported, primarily in patients with severe underlying diseases.
A 74-year-old female developed hepatotoxicity and significantly increased AST (4962 units/L), ALT (7071 units/L), alkaline phosphatase (90 units/L), and total bilirubin (2.5 mg/dL) after starting this drug. Levels returned to normal within a week after discontinuation.
Severe hepatotoxicity usually occurred within 14 days (most within 6 days) after starting this drug and most cases were not associated with hypersensitivity. The majority of fatal hepatotoxicity cases occurred in patients 65 years or older and most were not associated with hypersensitivity.[Ref]
Genitourinary
- Common (1% to 10%): Vaginitis
- Uncommon (0.1% to 1%): Genital moniliasis
- Frequency not reported: Dysmenorrhea, hematuria, dysuria, oliguria, urinary incontinence, urinary retention, leukorrhea, genital pruritus, ejaculation failure, impotence, albuminuria, candiduria, crystalluria, cylindruria, vaginal candidiasis, urinary tract infection
Nebulizer Solution:
- Common (1% to 10%): Vulvovaginal mycotic infection[Ref]
Metabolic
- Uncommon (0.1% to 1%): Anorexia, hyperglycemia, hyperkalemia, hypoglycemia
- Frequency not reported: Decreased blood glucose, hypomagnesemia, thirst, aggravated diabetes mellitus, dehydration, hypokalemia, gout, hypernatremia, hypophosphatemia, weight decrease, fluid overload, hyponatremia, acidosis, symptomatic hypoglycemia, electrolyte abnormalities
Nebulizer Solution:
- Very common (10% or more): Anorexia
- Common (1% to 10%): Increased and decreased blood glucose
Fluoroquinolones:
- Frequency not reported: Attacks of porphyria[Ref]
Hypoglycemia has been reported, especially in diabetic patients.
A 79-year-old male with type 2 diabetes mellitus developed severe hypoglycemia (blood glucose 6 mg/dL) and became unresponsive 6 hours after receiving 1 dose of this drug (250 mg IV). Blood glucose levels subsequently ranged between 40 to 159 mg/dL with dextrose doses and infusions; however, he did not regain consciousness and expired 2 days later.
Attacks of porphyria in patients with porphyria have been associated with fluoroquinolone use.[Ref]
Cardiovascular
- Common (1% to 10%): Phlebitis
- Uncommon (0.1% to 1%): Cardiac arrest, palpitation, ventricular arrhythmia, ventricular tachycardia
- Rare (0.01% to 0.1%): Tachycardia, hypotension
- Frequency not reported: Angina pectoris, arrhythmia, atrial fibrillation, bradycardia, cardiac failure, cerebrovascular disorder, circulatory failure, coronary thrombosis, heart block, hypertension, aggravated hypertension, myocardial infarction, postural hypotension, purpura, supraventricular tachycardia, deep thrombophlebitis, vasculitis, ventricular fibrillation
- Postmarketing reports: Vasodilation, QT interval prolongation/prolonged ECG QT, torsade de pointes
Nebulizer Solution:
- Uncommon (0.1% to 1%): Tachycardia, prolonged ECG QT[Ref]
Ventricular arrhythmia and torsade de pointes have been reported, mainly in patients with risk factors of QT prolongation.
This drug was associated with 13 cases of torsade de pointes reported to the FDA between 1996 and 2001.
An 88-year-old woman developed a prolonged QTc interval during treatment with this drug (500 mg once a day). The QTc interval increased from 450 msec to 577 msec by the fourth day of treatment. This drug was discontinued after the patient experienced runs of ventricular tachycardia. The QTc interval then decreased to 437 msec 2 days after discontinuing this drug.
A 65-year-old woman with hypokalemia (2.8 mEq/L), hypomagnesemia (1.5 mEq/L), and renal insufficiency (serum creatinine 7.7 mg/dL, BUN 34 mg/dL) developed a QTc interval of 605 ms (baseline 435 to 485 ms), several episodes of torsade de pointes, and cardiac arrest after 3 days of this drug (250 mg/day IV). The QTc interval decreased to 399 ms and no further arrhythmias occurred after discontinuation of this drug and electrolyte replacement.
Hypotension has been associated with rapid or bolus IV infusion.[Ref]
Local
- Common (1% to 10%): Injection site reactions (pain, reddening)
- Frequency not reported: Injection site pain, injection site inflammation[Ref]
Musculoskeletal
- Uncommon (0.1% to 1%): Arthralgia, myalgia, skeletal pain, tendinitis
- Rare (0.01% to 0.1%): Tendon disorders (including tendinitis [e.g., Achilles tendon]), muscular weakness
- Frequency not reported: Arthritis, arthrosis, pathological fracture, osteomyelitis, synovitis , back pain, ligament rupture
- Postmarketing reports: Tendon rupture (e.g., Achilles tendon), muscle injury (including rupture), increased muscle enzymes, rhabdomyolysis
Nebulizer Solution:
- Common (1% to 10%): Arthralgia, myalgia
- Uncommon (0.1% to 1%): Tendinitis, costochondritis, joint stiffness[Ref]
Achilles tendon rupture occurred in 4 of 489 study patients (3217 treatment days) after 1 to 10 days of this drug.
Severe rhabdomyolysis occurred in a 77-year-old female after 6 days of oral therapy. She developed acute renal failure (serum creatinine 678 micromole/L), hyperkalemia (6.8 micromole/L), anuria, elevated creatine kinase (30,400 international units/L), myoglobinemia (86,000 mcg/L), and acute hepatic cytolysis (AST 555 international units/L, ALT 249 international units/L). The fluid/electrolyte disorders and creatine kinase and myoglobin levels improved with hemodialysis; however, the patient died of a myocardial infarction and respiratory failure after 13 days.[Ref]
Renal
- Uncommon (0.1% to 1%): Abnormal renal function, acute renal failure (e.g., due to interstitial nephritis), increased blood creatinine
- Frequency not reported: Renal calculi, allergic interstitial nephritis, increased nonprotein nitrogen
- Postmarketing reports: Interstitial nephritis
Nebulizer Solution:
- Common (1% to 10%): Increased blood creatinine
- Uncommon (0.1% to 1%): Renal failure[Ref]
A 73-year-old male developed vasculitis and acute renal failure within 3 days of starting oral therapy. Symptoms included significantly decreased urine output (0.5 to 0.7 L/day), palpable purpura, erythematous skin lesions, and increased serum creatinine (6.4 mg/dL) and BUN (190 mg/dL). The condition resolved within 4 weeks after discontinuation of this drug. Due to the possibility that this may have been an allergic reaction, rechallenge was not attempted.[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Allergic reaction
- Rare (0.01% to 0.1%): Hypersensitivity
- Postmarketing reports: Hypersensitivity reactions (sometimes fatal and including anaphylactic/anaphylactoid reactions, anaphylactic/anaphylactoid shock, serum sickness, angioneurotic edema)
Nebulizer Solution:
- Uncommon (0.1% to 1%): Hypersensitivity[Ref]
Anaphylactic and anaphylactoid reactions have been reported, sometimes after the first dose.[Ref]
Hematologic
- Uncommon (0.1% to 1%): Anemia, granulocytopenia, thrombocytopenia, eosinophilia, leukopenia
- Rare (0.01% to 0.1%): Neutropenia
- Frequency not reported: Decreased lymphocytes, abnormal WBCs (unspecified), abnormal platelets, agranulocytosis, hematoma, leukocytosis, lymphadenopathy, decreased prothrombin, purpura, thrombocythemia, serious hematological side effects (e.g., pancytopenia, agranulocytosis, hemolytic anemia)
- Postmarketing reports: Hemolytic anemia, pancytopenia, aplastic anemia, prothrombin time prolonged, INR prolonged
Nebulizer Solution:
- Uncommon (0.1% to 1%): Anemia, neutropenia, increased eosinophil count, decreased platelet count[Ref]
Serious hematological side effects (e.g., pancytopenia, agranulocytosis, hemolytic anemia) have been reported after systemic administration of this drug.[Ref]
Ocular
- Rare (0.01% to 0.1%): Visual disturbances (e.g., blurred vision)
- Frequency not reported: Ophthalmologic abnormalities (including cataracts, multiple punctate lenticular opacities), abnormal vision, eye pain, nystagmus, conjunctivitis, transient vision loss
- Postmarketing reports: Vision disturbance (including diplopia), reduced visual acuity, blurred vision, scotomata, uveitis
Nebulizer Solution:
- Uncommon (0.1% to 1%): Visual disturbance[Ref]
Endocrine
- Rare (0.01% to 0.1%): Syndrome of inappropriate secretion of antidiuretic hormone (SIADH)[Ref]
Oncologic
- Frequency not reported: Carcinoma[Ref]
References
1. (2001) "Product Information. Levaquin (levofloxacin)." Ortho McNeil Pharmaceutical
2. Kahn JB (2001) "Latest industry information on the safety profile of levofloxacin in the US." Chemotherapy, 47 Suppl 3, p. 32-7
3. Yagawa K (2001) "Latest industry information on the safety profile of levofloxacin in Japan." Chemotherapy, 47 Suppl 3, p. 38-43
4. Croom KF, Goa KL (2003) "Levofloxacin: A Review of its Use in the Treatment of Bacterial Infections in the United States." Drugs, 63, p. 2769-2802
5. Anderson VR, Perry CM (2008) "Levofloxacin : a review of its use as a high-dose, short-course treatment for bacterial infection." Drugs, 68, p. 535-65
6. Goodwin SD, Gallis HA, Chow AT, Wong FA, Flor SC, Bartlett JA (1994) "Pharmacokinetics and safety of levofloxacin in patients with human immunodeficiency virus infection." Antimicrob Agents Chemother, 38, p. 799-804
7. Kawai T (1995) "Clinical evaluation of levofloxacin 200 mg 3 times daily in the treatment of bacterial lower respiratory tract infections." Drugs, 49(suppl 2, p. 416-7
8. Chien SC, Wong FA, Fowler CL, CalleryDAmico SV, Williams RR, Nayak R, Chow AT (1998) "Double-blind evaluation of the safety and pharmacokinetics of multiple oral once-daily 750-milligram and 1-gram doses of levofloxacin in healthy volunteers." Antimicrob Agents Chemother, 42, p. 885-8
9. Sydnor TA, Kopp EJ, Anthony KE, LoCoco JM, Kim SS, Fowler CL (1998) "Open-label assessment of levofloxacin for the treatment of acute bacterial sinusitis in adults." Ann Allergy Asthma Immunol, 80, p. 357-62
10. Klimberg IW, Cox CE, Fowler CL, King W, Kim SS, CalleryDAmico S (1998) "A controlled trial of levofloxacin and lomefloxacin in the treatment of complicated urinary tract infection." Urology, 51, p. 610-5
11. Adelglass J, Jones TM, Ruoff G, et al. (1998) "A multicenter, investigator-blinded, randomized comparison of oral levofloxacin and oral clarithromycin in the treatment of bacterial sinusitis." Pharmacotherapy, 18, p. 1255-63
12. Cohen JS (2001) "Peripheral neuropathy associated with fluoroquinolones." Ann Pharmacother, 35, p. 1540-7
13. Bird SB, Orr PG, Mazzola JL, Brush DE, Boyer EW (2005) "Levofloxacin-Related Seizure Activity in a Patient With Alzheimer's Disease: Assessment of Potential Risk Factors." J Clin Psychopharmacol, 25, p. 287-288
14. Shams WE, Evans ME (2005) "Guide to Selection of Fluoroquinolones in Patients with Lower Respiratory Tract Infections." Drugs, 65, p. 949-991
15. Marra F, Marra CA, Moadebi S, et al. (2005) "Levofloxacin treatment of active tuberculosis and the risk of adverse events." Chest, 128, p. 1406-13
16. Bellon A, Perez-Garcia G, Coverdale JH, Chacko RC (2009) "Seizures associated with levofloxacin: case presentation and literature review." Eur J Clin Pharmacol, 65, p. 959-62
17. Sato A, Ogawa H, Iwata M, Ono T, Yasuda K, Nagayama M, Shirai T, Shirai M, Ida M, Suda T, et al. (1995) "Clinical efficacy of levofloxacin in elderly patients with respiratory tract infections." Drugs, 49(suppl 2, p. 428-9
18. Gopal Rao G, Mahankali Rao CS, Starke I (2003) "Clostridium difficile-associated diarrhoea in patients with community-acquired lower respiratory infection being treated with levofloxacin compared with beta-lactam-based therapy." J Antimicrob Chemother, 51, p. 697-701
19. Boccumini LE, Fowler CL, Campbell TA, Puertolas LF, Kaidbey KH (2000) "Photoreaction potential of orally administered levofloxacin in healthy subjects." Ann Pharmacother, 34, p. 453-8
20. Digwood-Lettieri S, Reilly KJ, Haith LR Jr, et al. (2002) "Levofloxacin-induced toxic epidermal necrolysis in an elderly patient." Pharmacotherapy, 22, p. 789-93
21. Dawe RS, Ibbotson SH, Sanderson JB, Thomson EM, Ferguson J (2003) "A randomized controlled trial (volunteer study) of sitafloxacin, enoxacin, levofloxacin and sparfloxacin phototoxicity." Br J Dermatol, 149, p. 1232-41
22. Corral De La Calle M, Martin Diaz MA, Flores CR, Vidaurrazaga C (2005) "Acute localized exanthematous pustulosis secondary to levofloxacin." Br J Dermatol, 152, p. 1076-7
23. Islam AS, Rahman MS (2005) "Levofloxacin-induced fatal toxic epidermal necrolysis." Ann Pharmacother, 39, p. 1136-7
24. Maunz G, Conzett T, Zimmerli W (2009) "Cutaneous vasculitis associated with fluoroquinolones." Infection, 37, p. 466-8
25. Karim A, Ahmed S, Rossoff LJ, Siddiqui RK, Steinberg HN (2001) "Possible levofloxacin-induced acute hepatocellular injury in a patient with chronic obstructive lung disease." Clin Infect Dis, 33, p. 2088-90
26. Coban S, Ceydilek B, Ekiz F, Erden E, Soykan I (2005) "Levofloxacin-induced acute fulminant hepatic failure in a patient with chronic hepatitis B infection." Ann Pharmacother, 39, p. 1737-40
27. Paterson JM, Mamdani MM, Manno M, Juurlink DN (2012) "Fluoroquinolone therapy and idiosyncratic acute liver injury: a population-based study." CMAJ, 184, p. 1565-70
28. Friedrich LV, Dougherty R (2004) "Fatal hypoglycemia associated with levofloxacin." Pharmacotherapy, 24, p. 1807-12
29. Graumlich JF, Habis S, Avelino RR, et al. (2005) "Hypoglycemia in inpatients after gatifloxacin or levofloxacin therapy: nested case-control study." Pharmacotherapy, 25, p. 1296-302
30. Lodise T, Graves J, Miller C, Mohr JF, Lomaestro B, Smith RP (2007) "Effects of gatifloxacin and levofloxacin on rates of hypoglycemia and hyperglycemia among elderly hospitalized patients." Pharmacotherapy, 27, p. 1498-505
31. Laplante KL, Mersfelder TL, Ward KE, Quilliam BJ (2008) "Prevalence of and risk factors for dysglycemia in patients receiving gatifloxacin and levofloxacin in an outpatient setting." Pharmacotherapy, 28, p. 82-9
32. Singh N, Jacob JJ (2008) "Levofloxacin and hypoglycemia." Clin Infect Dis, 46, p. 1127
33. Gibert AE, Porta FS (2008) "Hypoglycemia and levofloxacin: a case report." Clin Infect Dis, 46, p. 1126-7
34. Kelesidis T, Canseco E (2009) "Levofloxacin-induced hypoglycemia: a rare but life-threatening side effect of a widely used antibiotic." Am J Med, 122, e3-4
35. Kelesidis T, Canseco E (2010) "Quinolone-induced hypoglycemia: a life-threatening but potentially reversible side effect." Am J Med, 123, e5-6
36. Micheli L, Sbrilli M, Nencini C (2012) "Severe hypoglycemia associated with levofloxacin in Type 2 diabetic patients receiving polytherapy: two case reports." Int J Clin Pharmacol Ther, 50, p. 302-6
37. Samaha FF (1999) "QTC interval prolongation and polymorphic ventricular tachycardia in association with levofloxacin." Am J Med, 107, p. 528-9
38. Iannini PB, Doddamani S, Byazrova E, Curciumaru I, Kramer H (2001) "Risk of torsades de pointes with non-cardiac drugs." BMJ, 322, p. 46-7
39. Frothingham R (2001) "Rates of torsades de pointes associated with ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and moxifloxacin." Pharmacotherapy, 21, p. 1468-72
40. Owens RC Jr, Ambrose PG (2002) "Torsades de pointes associated with fluoroquinolones." Pharmacotherapy, 22, 663-8; discussion 668-72
41. Amankwa K, Krishnan SC, Tisdale JE (2004) "Torsades de pointes associated with fluoroquinolones: Importance of concomitant risk factors." Clin Pharmacol Ther, 75, p. 242-7
42. Ramakrishnan K, Scheid DC (2005) "Diagnosis and management of acute pyelonephritis in adults." Am Fam Physician, 71, p. 933-42
43. Berger RE (2005) "Rates of torsades de pointes associated with ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and moxifloxacin." J Urol, 174, p. 165
44. Makaryus AN, Byrns K, Makaryus MN, Natarajan U, Singer C, Goldner B (2006) "Effect of ciprofloxacin and levofloxacin on the QT interval: is this a significant "clinical" event?" South Med J, 99, p. 52-6
45. Owens RC Jr, Nolin TD (2006) "Antimicrobial-Associated QT Interval Prolongation: Pointes of Interest." Clin Infect Dis, 43, p. 1603-1611
46. Briasoulis A, Agarwal V, Pierce WJ (2011) "QT Prolongation and Torsade de Pointes Induced by Fluoroquinolones: Infrequent Side Effects from Commonly Used Medications." Cardiology, 120, p. 103-110
47. Abo-Salem E, Nugent K, Chance W (2011) "Antibiotic-induced cardiac arrhythmia in elderly patients." J Am Geriatr Soc, 59, p. 1747-9
48. Lapi F, Wilchesky M, Kezouh A, Benisty JI, Ernst P, Suissa S (2012) "Fluoroquinolones and the risk of serious arrhythmia: a population-based study." Clin Infect Dis, 55, p. 1457-65
49. Lewis JR, Gums JG, Dickensheets DL (1999) "Levofloxacin-induced bilateral achilles tendonitis." Ann Pharmacother, 33, p. 792-5
50. Fleisch E, Hartmann K, Kuhn M (2000) "Fluouroquinolone-induced tendinopathy: Also occurring with levofloxacin." Infection, 28, p. 256-7
51. Haddow LJ, Chandra Sekhar M, Hajela V, Gopal Rao G (2003) "Spontaneous Achilles tendon rupture in patients treated with levofloxacin." J Antimicrob Chemother, 51, p. 747-8
52. Khaliq Y, Zhanel GG (2003) "Fluoroquinolone-Associated Tendinopathy: A Critical Review of the Literature." Clin Infect Dis, 36, p. 1404-1410
53. Mathis AS, Chan V, Gryszkiewicz M, Adamson RT, Friedman GS (2003) "Levofloxacin-Associated Achilles Tendon Rupture." Ann Pharmacother, 37, p. 1014-1017
54. Petitjeans F, Nadaud J, Perez JP, et al. (2003) "A case of rhabdomyolysis with fatal outcome after a treatment with levofloxacin." Eur J Clin Pharmacol, 59, p. 779-80
55. Hsiao SH, Chang CM, Tsao CJ, Lee YY, Hsu MY, Wu TJ (2004) "Acute rhabdomyolysis associated with ofloxacin/levofloxacin therapy." Ann Pharmacother, 39, p. 146-9
56. Vyas H, Krishnaswamy G (2007) "Images in clinical medicine. Quinolone-associated rupture of the Achilles' tendon." N Engl J Med, 357, p. 2067
57. Solomon NM, Mokrzycki MH (2000) "Levofloxacin-induced allergic interstitial nephritis." Clin Nephrol, 54, p. 356
58. Famularo G, De Simone C (2002) "Nephrotoxicity and purpura associated with levofloxacin." Ann Pharmacother, 36, p. 1380-2
59. Oh YR, Carr-Lopez SM, Probasco JM, Crawley PG (2003) "Levofloxacin-induced autoimmune hemolytic anemia." Ann Pharmacother, 37, p. 1010-3
Frequently asked questions
- What are the best antibiotics for pneumonia?
- What is the best antibiotic to treat a sinus infection?
- What antibiotics are used to treat UTI?
- Can Levaquin cause tendonitis?
More about levofloxacin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (746)
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
Patient resources
Other brands
Professional resources
- Levofloxacin monograph
- Levofloxacin (FDA)
- Levofloxacin Injection Concentrate (FDA)
- Levofloxacin Oral Solution (FDA)
- Levofloxacin Tablets (FDA)
Other brands
Related treatment guides
Further information
Levofloxacin side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.