Amantadine Side Effects
Applies to amantadine: oral capsule, oral capsule extended release, oral capsule liquid filled, oral solution, oral syrup, oral tablet, oral tablet extended release.
Precautions
It is very important that your doctor check your progress at regular visits to see if the medicine is working properly and to allow changes in your dose. Blood and urine tests may be needed to check for any unwanted effects.
Amantadine may cause some people to be agitated, irritable, or display other abnormal behaviors. It may also cause some people to have suicidal thoughts and tendencies or to become more depressed. Also tell your doctor if you have sudden or strong feelings, such as feeling nervous, angry, restless, violent, or scared. If you, your child, or your caregiver notice any of these adverse effects, tell your doctor or your child's doctor right away.
Some people who have used this medicine had unusual changes in their behavior. Talk with your doctor right away if you start having unusual urges, such as gambling urges, binge or compulsive eating, compulsive shopping, or sexual urges while using this medicine.
Drinking alcoholic beverages while taking this medicine may cause increased side effects, such as circulation problems, dizziness, lightheadedness, fainting, or confusion. Do not drink alcoholic beverages while you are taking this medicine.
This medicine may cause some people to become dizzy, drowsy, or lightheaded, or to have blurred vision or trouble concentrating. Do not drive or do anything else that could be dangerous until you know how this medicine affects you.
Dizziness, lightheadedness, or fainting may occur with this medicine, especially when you suddenly get up from a lying or sitting position. These symptoms are more likely to occur when you begin taking this medicine or when the dose is increased. Getting up slowly may help. If this problem continues or gets worse, check with your doctor.
Patients with Parkinson's disease must be careful not to overdo physical activities when their condition improves and body movements become easier, since injuries resulting from falls may occur. Such activities must be gradually increased to give your body time to adjust to a change in balance, circulation, and coordination.
Amantadine may cause dryness of the mouth, nose, and throat. For temporary relief of mouth dryness, use sugarless candy or gum, melted bits of ice in your mouth, or use a saliva substitute. If your mouth continues to feel dry for more than 2 weeks, check with your doctor or dentist. Continuing dryness of the mouth may increase the chance of dental disease, including tooth decay, gum disease, and fungus infections.
This medicine may cause purplish red, net-like, blotchy spots on the skin. This problem occurs more often in females and usually occurs on the legs or feet after this medicine has been taken regularly for a month or more. Although the blotchy spots may remain as long as you are taking this medicine, they will usually go away gradually within 2 to 12 weeks after you stop taking the medicine. If you have any questions about this, talk with your doctor.
Check with your doctor right away if you are having convulsions (seizures), difficulty with breathing, a fast heartbeat, a high fever, high or low blood pressure, increased sweating, loss of bladder control, severe muscle stiffness, unusually pale skin, or tiredness. These could be symptoms of a serious condition called neuroleptic malignant syndrome (NMS).
If you are using this medicine for Parkinson's disease, do not Stop taking amantadine suddenly without first checking with your doctor. Your doctor may want you to slowly reduce the amount you are using before stopping it completely.
If you are using this medicine for Parkinson's disease, it is important that your doctor check your skin regularly for signs of melanoma (skin cancer). If you notice any unusual red, brown, or black spots on your skin, check with your doctor right away.
If your Parkinson's symptoms do not improve within a few days, if they become worse, or if this medicine appears less effective after a few weeks, check with your doctor.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of amantadine
Along with its needed effects, amantadine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking amantadine:
More common side effects
- bladder pain
- bloody or cloudy urine
- blurred vision
- confusion
- difficult, burning, or painful urination
- dizziness or lightheadedness
- fainting
- falls
- frequent urge to urinate
- lower back or side pain
- seeing, hearing, or feeling things that are not there
- swelling of the hands, feet, or lower legs
Less common side effects
- inability to move the eyes
- increased blinking or spasms of the eyelid
- muscle spasm
- sticking out of the tongue
- trouble breathing, speaking, or swallowing
- uncontrolled twisting movements of the neck, trunk, arms, or legs
- unusual facial expressions
Rare side effects
- chills
- decreased vision or any change in vision
- difficulty in coordination
- fever
- increased blood pressure
- increase in body movements
- irritation and swelling of the eye
- loss of memory
- mental depression
- seizures
- severe mood or mental changes
- skin rash
- slurred speech
- sore throat
- thoughts of suicide or attempts at suicide
Other side effects of amantadine
Some side effects of amantadine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- agitation
- anxiety
- difficulty concentrating
- dry mouth
- headache
- irritability
- loss of appetite
- nausea
- nervousness
- nightmares
- purplish red, net-like, or blotchy spots on the skin
- trouble with sleeping
Less common side effects
- blindness
- blurred vision
- constipation
- decrease in sexual desire
- decreased vision
- diarrhea
- drowsiness
- dry eyes
- dryness of the mouth, nose, and throat
- false sense of well-being
- joint swelling
- unusual tiredness or weakness
- vomiting
See also:
For healthcare professionals
Applies to amantadine: compounding powder, oral capsule, oral capsule extended release, oral liquid, oral tablet, oral tablet extended release.
General adverse events
The more commonly reported adverse reactions have included nausea, dizziness/lightheadedness, and insomnia.[Ref]
Nervous system
- Common (1% to 10%): Dizziness/lightheadedness, ataxia, headache, somnolence, dystonia
- Uncommon (0.1% to 1%): Weakness, slurred speech, hyperkinesia
- Rare (less than 0.1%): Convulsion
- Frequency not reported: Falling asleep during activities of daily living, withdrawal-emergent hyperpyrexia (a syndrome resembling neuroleptic malignant syndrome)
- Postmarketing reports: Coma, delirium, hypokinesia, involuntary muscle contractions, gait abnormalities, paresthesia, EEG changes, tremor[Ref]
Psychiatric
- Very common (10% or more): Hallucinations (up to 21%)
- Common (1% to 10%): Insomnia, depression, anxiety, irritability, hallucinations, confusion, nervousness, abnormal dreams, agitation
- Uncommon (0.1% to 1%): Psychosis, euphoria, abnormal thinking, amnesia
- Rare (less than 0.1%): Suicide attempt, suicide, suicidal ideation
- Postmarketing reports: Stupor, delusions, aggressive behavior, paranoid reaction, manic reaction, pathological gambling, increased libido including hypersexuality, and impulse control symptoms[Ref]
Gastrointestinal
- Very common (10% or more): Dry mouth (up to 16%); constipation (up to 13%)
- Common (1% to 10%): Nausea, anorexia, diarrhea, decreased appetite
- Uncommon (0.1% to 1%): Vomiting
- Postmarketing reports: Dysphagia[Ref]
Cardiovascular
- Very common (10% or more): Peripheral edema (up to 16%), orthostatic hypotension (up to 13%)
- Uncommon (0.1% to 1%): Congestive heart failure, hypertension
- Postmarketing reports: Cardiac arrest, arrhythmias including malignant arrhythmias, hypotension, and tachycardia[Ref]
Ocular
- Common (1% to 10%): Dry eye, cataract, blurred vision
- Uncommon (0.1% to 1%): Visual disturbance, punctate subeithelial or other corneal opacity, corneal edema, decreased visual acuity, sensitivity to light, optic nerve palsy
- Rare (less than 0.1%): Oculogyric episodes
- Postmarketing reports: Keratitis, mydriasis[Ref]
Other
- Very common (10% or more): Fall (up to 13%)
- Common (1% to 10%): Fatigue, contusions
- Frequency not reported: Death
- Postmarketing reports: Fever[Ref]
Deaths have been reported from overdose with the lowest reported acute lethal dose as 1 gram. Drug overdose has resulted in cardiac, respiratory, renal, or CNS toxicity. Deaths have been reported in patients with renal impairment and attributed to drug accumulation.[Ref]
Respiratory
- Common (1% to 10%): Dry nose, cough
- Uncommon (0.1% to 1%): Dyspnea
- Postmarketing reports: Acute respiratory failure, pulmonary edema, tachypnea[Ref]
Hematologic
- Rare (less than 0.1%): Leukopenia, neutropenia
- Postmarketing reports: Leukocytosis, agranulocytosis[Ref]
Dermatologic
- Common (1% to 10%): Livedo reticularis, pigmentation disorder
- Uncommon (0.1% to 1%): Skin rash
- Rare (less than 0.1%): Eczematoid dermatitis
- Postmarketing reports: Pruritus, diaphoresis[Ref]
Hypersensitivity
- Postmarketing reports: Allergic reactions including anaphylactic reactions[Ref]
Genitourinary
- Common (1% to 10%): Urinary tract infection, benign prostatic hyperplasia
- Uncommon (0.1% to 1%): Urinary retention, decreased libido[Ref]
Renal
- Postmarketing reports: Elevated: CPK, BUN, serum creatinine[Ref]
Hepatic
- Rare (less than 0.1%): Reversible liver enzyme elevations
- Postmarketing reports: Elevated: alkaline phosphatase, LDH, bilirubin, GGT, SGOT, and SGPT[Ref]
Musculoskeletal
- Common (1% to 10%): Joint swelling, muscle spasms[Ref]
References
1. (2002) "Product Information. Symmetrel (amantadine)." DuPont Pharmaceuticals
2. (2018) "Product Information. Gocovri (amantadine)." Adamas Pharmaceuticals Inc.
3. (2018) "Product Information. Amantadine Hydrochloride (amantadine)." Sandoz Inc
4. Smith EJ (2008) "Amantadine-induced psychosis in a young healthy patient." Am J Psychiatry, 165, p. 1613
5. Michalski LS, Hantsch Bardsley C, Holt DR, Milner JE, Hou SH (2009) "Altered mental status in a transplant patient. Amantadine toxicity." Kidney Int, 75, p. 243-4
6. (2009) "Antiviral drugs for influenza." Med Lett Drugs Ther, 51, p. 89-92
7. Kataoka H, Ueno S (2011) "Dropped head associated with amantadine in Parkinson disease." Clin Neuropharmacol, 34, p. 48-9
8. Beal E (2011) "Parkinson disease: Amantadine administration is associated with impulse control disorders in PD." Nat Rev Neurol, 7, p. 62
9. Salgado JC, Gutknecht DR (2006) "A reticular rash." Am J Med, 119, p. 577-8
10. Alonso Navarro H, Sanz-Aiz A, Izquierdo L, Jimenez Jimenez FJ (2009) "Syndrome of Inappropriate Antidiuretic Hormone Secretion Possibly Associated With Amantadine Therapy in Parkinson Disease." Clin Neuropharmacol, 32, p. 167-168
Frequently asked questions
- What is the difference between Osmolex ER and Gocovri?
- What is Gocovri used to treat?
- Why should you not discontinue amantadine?
- Why was amantadine discontinued for flu?
- How long does it take for amantadine to start working?
- What symptoms does amantadine treat?
- What is Gocovri (amantadine) and how does it work?
More about amantadine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (59)
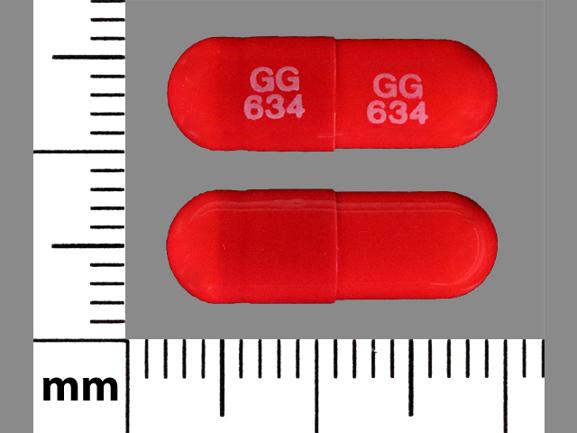
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: adamantane antivirals
- Breastfeeding
- En español
Patient resources
Other brands
Gocovri, Symmetrel, Osmolex ER
Professional resources
- Amantadine Hydrochloride (Antiparkinson) monograph
- Amantadine Hydrochloride (Antiviral) (AHFS Monograph)
- Amantadine (FDA)
- Amantadine Capsules (FDA)
- Amantadine Oral Solution USP (FDA)
Other brands
Related treatment guides
Further information
Amantadine side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.