Triazolam (Monograph)
Brand name: Halcion
Drug class: Benzodiazepines
VA class: CN302
CAS number: 28911-01-5
Warning
- Concomitant Use with Opiates
-
Concomitant use of benzodiazepines and opiates may result in profound sedation, respiratory depression, coma, and death.
-
Reserve concomitant use for patients in whom alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy and monitor closely for respiratory depression and sedation. (See Specific Drugs and Foods under Interactions.)
- Potential for Abuse, Addiction, and Other Serious Risks
-
A boxed warning has been included in the prescribing information for all benzodiazepines describing risks of abuse, misuse, addiction, physical dependence, and withdrawal reactions.
-
Abuse and misuse can result in overdose or death, especially when benzodiazepines are combined with other medicines, such as opioid pain relievers, alcohol, or illicit drugs.
-
Assess a patient’s risk of abuse, misuse, and addiction. Standardized screening tools are available ([Web]).
-
To reduce risk of acute withdrawal reactions, use a gradual dose taper when reducing dosage or discontinuing benzodiazepines. Take precautions when benzodiazepines are used in combination with opioid medications.
Introduction
Benzodiazepine; sedative and hypnotic.
Uses for Triazolam
Insomnia
Short-term (generally 7–10 days) management of insomnia.
Decreases sleep latency, increases the duration of sleep, and decreases the number of nocturnal awakenings.
Has been used for the prevention or short-term treatment of transient insomnia associated with sleep-wake schedule changes† [off-label] (e.g., rapid travel across time zones [“jet lag”], rotating shift work). May be useful for this purpose in some patients; however, consider the possibility of transient impairment of cognitive function (e.g., anterograde amnesia [“traveler’s amnesia”]). (See Amnesia under Cautions.)
Triazolam Dosage and Administration
General
-
Use only when able to get 7–8 hours of sleep before being active again.
-
Avoid prolonged administration. Generally limit hypnotic therapy to 7–10 days.
-
Write prescriptions for short-term (7–10 days) use only; the quantity dispensed to the patient should not exceed a 1-month supply.
-
Reevaluate patient if triazolam is to be used for more than 2–3 weeks.
-
Avoid abrupt discontinuance in patients who have received prolonged therapy (because of potential for precipitating withdrawal manifestations); after therapy with more than the lowest dose for longer than a few weeks, taper dosage gradually, particularly in patients with a seizure history.
-
Consider gradual dosage reduction (e.g., over several nights) when discontinuing short-term triazolam therapy (because of potential for rebound insomnia).
Administration
Oral Administration
Administer at bedtime.
Avoid concomitant oral administration with grapefruit juice.
Dosage
Individualize dosage; use the smallest effective dose.
Some adverse effects (e.g., amnesia, dizziness, drowsiness, lightheadedness) appear to be dose related. Inconclusive whether other effects (e.g., confusion, bizarre or abnormal behavior, agitation, hallucinations) are dose related.
Adults
Insomnia
Oral
Usual dose is 0.25 mg.
In some patients (e.g., those with low body weight), 0.125 mg may be adequate.
Reserve 0.5-mg dose for exceptional cases in which the patient does not respond adequately to a lower dose.
Prescribing Limits
Adults
Insomnia
Oral
Maximum 0.5 mg daily.
Special Populations
Hepatic Impairment
No specific dosage recommendations.
Renal Impairment
No specific dosage recommendations.
Geriatric or Debilitated Patients
Usual dosages in healthy geriatric patients should be approximately half those in younger adults.
Initially, 0.125 mg daily. Increased risk of adverse (e.g., behavioral) effects if therapy is initiated at doses >0.125 mg.
Reserve 0.25-mg dose for exceptional cases in which the patient does not respond adequately to a lower dose.
Cautions for Triazolam
Contraindications
-
Concomitant use of itraconazole, ketoconazole, nefazodone, delavirdine, efavirenz, or HIV protease inhibitors.
-
Pregnancy.
-
Known hypersensitivity to benzodiazepines or any ingredient in the formulation.
Warnings/Precautions
Warnings
Concomitant Use with Opiates
Concomitant use of benzodiazepines, including triazolam, and opiates may result in profound sedation, respiratory depression, coma, and death. Substantial proportion of fatal opiate overdoses involve concurrent benzodiazepine use.
Reserve concomitant use of triazolam and opiates for patients in whom alternative treatment options are inadequate. (See Specific Drugs and Foods under Interactions.)
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; avoid use of benzodiazepines as hypnotics during pregnancy. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Adequate Patient Evaluation
Insomnia may be a manifestation of an underlying physical and/or psychiatric disorder; carefully evaluate patient before providing symptomatic treatment.
Failure of insomnia to remit after 7–10 days of treatment, worsening of insomnia, or emergence of new abnormal thinking or behavior may indicate the presence of an underlying psychiatric and/or medical condition.
Complex Sleep-related Behaviors
Potential risk of complex sleep-related behaviors such as sleep-driving (i.e., driving while not fully awake after ingesting a sedative-hypnotic drug, with no memory of the event), making phone calls, or preparing and eating food, while asleep.
Adverse Psychiatric Events
Abnormal thinking and behavioral changes (e.g., aggressiveness, uncharacteristic extroversion, bizarre behavior, agitation, hallucinations, depersonalization, amnesia) may occur unpredictably in patients receiving benzodiazepines.
Some evidence suggests that some such behavioral effects may occur more frequently with triazolam than with other hypnotic benzodiazepines.
Immediately evaluate any new behavioral sign or symptom.
Amnesia
Anterograde amnesia of varying degrees of severity reported following therapeutic doses. Frequency may be greater with triazolam than with other benzodiazepines. May be particularly disturbing with triazolam, especially when high doses (e.g., 0.5 mg) are used.
Anterograde amnesia (“traveler’s amnesia”) that occurred upon awakening and persisted for several hours has been reported by individuals who took triazolam to induce sleep while traveling (e.g., during airplane flights). Concomitant use of alcohol may have been a contributory factor in some cases.
Bizarre behavior has been associated with the period of amnesia in some patients.
Consider the risk of anterograde amnesia in patients receiving triazolam, particularly when relatively high doses are considered (e.g., for transient insomnia associated with sleep-wake schedule changes) or when the duration of drug effect is likely to exceed the intended period of sleep (e.g., when taken to induce sleep while traveling).
CNS Depression
Performance of activities requiring mental alertness and physical coordination may be impaired.
Concurrent use of other CNS depressants may potentiate CNS depression. (See Concomitant Use with Opiates under Cautions and also see Specific Drugs and Foods under Interactions.)
Dependence and Abuse Potential
Psychologic and physical dependence may occur following prolonged use.
Patients with a history of drug or alcohol dependence or abuse are at risk of habituation or dependence; use only with careful surveillance in such patients.
Tolerance and Withdrawal Effects
Tolerance and adaptation to the hypnotic effect may occur after several weeks of therapy, resulting in diminished effectiveness during the end of each night’s use (early morning insomnia) and, possibly, increased daytime anxiety.
Increase in daytime anxiety reported after as few as 10 days of continuous use; daytime anxiety also may occur between nightly doses as a manifestation of interdose withdrawal. If increased daytime anxiety occurs, discontinuance may be advisable.
Potential for rebound insomnia for 1 or 2 nights after drug discontinuance.
Rapid dosage reduction or abrupt discontinuance may result in signs and symptoms of withdrawal (similar to barbiturates or alcohol).
CYP3A-mediated Drug Interactions
Concomitant use with drugs that are potent inhibitors of CYP3A (e.g., itraconazole, ketoconazole, nefazodone, delavirdine, efavirenz, HIV protease inhibitors) is contraindicated. Less potent inhibitors of CYP3A should be used concomitantly with caution; consider possible need for reduction of triazolam dosage. (See Interactions.)
Sensitivity Reactions
Potential risk of anaphylaxis and angioedema; may occur even with the first dose of drug.
General Precautions
Suicide
Use with caution in depressed patients; potential for suicidal tendencies. Prescribe and dispense drug in the smallest feasible quantity.
Respiratory Effects
Use with caution in patients with compromised respiratory function (e.g., chronic pulmonary insufficiency, sleep apnea). Respiratory depression and apnea reported infrequently in these patients.
Specific Populations
Pregnancy
Category X. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
If used during the last weeks of pregnancy, potential for neonatal CNS depression.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Use not recommended.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Geriatric Use
Increased sensitivity to dose-related adverse effects. Clearance is reduced and plasma concentrations are increased by about 50%. Use reduced dosages (see Geriatric or Debilitated Patients under Dosage and Administration); use the smallest effective dose.
Hepatic Impairment
Use with caution.
Renal Impairment
Use with caution.
Common Adverse Effects
Drowsiness, headache, dizziness, nervousness, lightheadedness, coordination disorders or ataxia, nausea or vomiting.
Drug Interactions
Metabolized by CYP3A.
Drugs Affecting Hepatic Microsomal Enzymes
Pharmacokinetic interaction (increased plasma triazolam concentrations) with inhibitors of CYP3A. Concomitant use with potent CYP3A inhibitors is contraindicated. Use less potent CYP3A inhibitors with caution; triazolam dosage reduction may be indicated (see table).
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Amiodarone |
Possible increased plasma concentrations of triazolam |
Use with caution |
|
Antidepressants, SSRIs (fluvoxamine, paroxetine, sertraline) |
Possible increased plasma concentrations of triazolam |
Use with caution |
|
Antifungals, azoles (itraconazole, ketoconazole) |
Increased plasma concentrations and decreased clearance of triazolam |
Concomitant use of itraconazole or ketoconazole is contraindicated; avoid concomitant use of other azole antifungals that are potent CYP3A inhibitors |
|
Calcium-channel blocking agents (diltiazem, nicardipine, nifedipine, verapamil) |
Possible increased plasma concentrations of triazolam |
Use with caution |
|
Cimetidine |
Increased plasma concentrations and decreased clearance of triazolam |
Use with caution; consider triazolam dosage reduction |
|
CNS depressants (e.g., psychotropic agents, anticonvulsants, antihistamines, alcohol) |
Additive CNS depressant effects |
Avoid concomitant use of alcohol; use other CNS depressants with caution |
|
Cyclosporine |
Possible increased plasma concentrations of triazolam |
Use with caution |
|
Delavirdine |
Decreased metabolism and clearance of triazolam; potential for intense and prolonged sedation and respiratory depression |
Concomitant use contraindicated |
|
Efavirenz |
Decreased metabolism and clearance of triazolam; potential for intense and prolonged sedation and respiratory depression |
Concomitant use contraindicated |
|
Ergotamine |
Possible increased plasma concentrations of triazolam |
Use with caution |
|
Grapefruit juice |
Increased triazolam bioavailability with concomitant oral administration |
Avoid concomitant administration |
|
HIV protease inhibitors (atazanavir, darunavir, fosamprenavir, indinavir, lopinavir/ritonavir, nelfinavir, ritonavir, saquinavir, tipranavir) |
Decreased metabolism and clearance of triazolam; potential for intense and prolonged sedation and respiratory depression |
Concomitant use contraindicated |
|
Isoniazid |
Increased plasma concentrations and decreased clearance of triazolam |
Use with caution |
|
Macrolide antibiotics (clarithromycin, erythromycin) |
Increased plasma concentrations and decreased clearance of triazolam |
Use with caution; consider triazolam dosage reduction |
|
Nefazodone |
Increased plasma concentrations and decreased clearance of triazolam |
Concomitant use contraindicated |
|
Opiate agonists and partial agonists |
Risk of profound sedation, respiratory depression, coma, or death |
Whenever possible, avoid concomitant use Opiate analgesics: Use concomitantly only if alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy; monitor closely for respiratory depression and sedation In patients receiving triazolam, initiate opiate analgesic, if required, at reduced dosage and titrate based on clinical response In patients receiving an opiate analgesic, initiate triazolam, if required, at lower dosage than indicated in the absence of opiate therapy and titrate based on clinical response Opiate antitussives: Avoid concomitant use Consider offering naloxone to patients receiving benzodiazepines and opiates concomitantly |
|
Oral contraceptives |
Increased plasma concentrations and decreased clearance of triazolam |
Use with caution |
|
Ranitidine |
Increased plasma concentrations of triazolam |
Use with caution |
|
Warfarin |
Effect on warfarin pharmacokinetics or PT unlikely |
Triazolam Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentration usually attained within 2 hours after oral administration.
Special Populations
In healthy geriatric patients, peak plasma concentration and AUC are increased by about 50% compared with younger adults.
Distribution
Extent
Benzodiazepines are widely distributed into body tissues and cross the blood-brain barrier.
Benzodiazepines generally cross the placenta and are distributed into milk; not known whether triazolam distributes into milk.
Elimination
Metabolism
Extensively metabolized in the liver. Hydroxylated by CYP3A and subsequently conjugated to form inactive metabolites.
Elimination Route
Excreted principally in urine as inactive glucuronide conjugates.
Half-life
1.5–5.5 hours.
Special Populations
In healthy geriatric patients, clearance is decreased by about 50% compared with younger adults.
Stability
Storage
Oral
Tablets
20–25°C.
Actions
-
Effects appear to be mediated through the inhibitory neurotransmitter GABA; the sites and mechanisms of action within the CNS appear to involve a macromolecular complex (GABAA-receptor-chloride ionophore complex) that includes GABAA receptors, high-affinity benzodiazepine receptors, and chloride channels.
-
Provide patient with a copy of the manufacturer's patient information.
-
Importance of taking only as prescribed; do not increase dosage or duration of therapy unless otherwise instructed by a clinician.
-
Risk of potentially fatal additive effects (e.g., profound sedation, respiratory depression, coma) if used concomitantly with opiates either therapeutically or illicitly. Avoid concomitant use of opiate antitussives; also avoid concomitant use of opiate analgesics unless use is supervised by clinician.
-
Importance of informing clinicians of any behavioral or mental changes, memory impairment, tolerance, or dependence/withdrawal symptoms.
-
Importance of taking only when able to get a full night’s sleep (i.e., 7–8 hours) before being active again.
-
Potential for drug to impair mental alertness or physical coordination; use caution when operating machinery or performing hazardous tasks until effects on individual are known.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and of concomitant illnesses, particularly depression.
-
Importance of not consuming alcoholic beverages.
-
Risk of rebound insomnia for 1 or 2 nights after discontinuance.
-
Importance of women informing their clinician if they are or plan to become pregnant or to breast-feed; necessity for clinicians to advise women to avoid pregnancy during therapy.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as a schedule IV (C-IV) drug.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
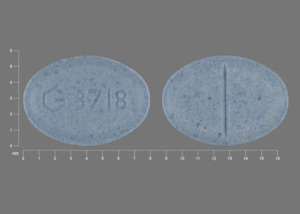
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
0.125 mg* |
Halcion (C-IV) |
Pfizer |
|
Triazolam Tablets (C-IV) |
||||
|
0.25 mg* |
Halcion (C-IV; scored) |
Pfizer |
||
|
Triazolam Tablets (C-IV) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 9, 2020. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about triazolam
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (77)
- Drug images
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: benzodiazepines
- Breastfeeding
- En español