Prochlorperazine (Systemic) (Sedative) (Monograph)
Brand name: Compro
Drug class: Phenothiazines
Warning
- Increased Mortality in Geriatric Patients with Dementia-related Psychosis
-
Geriatric patients with dementia-related psychosis treated with antipsychotic agents are at an increased risk of death.
-
Analyses of 17 placebo-controlled trials in geriatric patients mainly receiving atypical antipsychotic agents revealed an approximate 1.6- to 1.7-fold increase in mortality compared with that in patients receiving placebo.
-
Most fatalities appeared to result from cardiovascular-related events (e.g., heart failure, sudden death) or infections (mostly pneumonia).
-
Observational studies suggest that conventional or first-generation antipsychotic agents also may increase mortality in such patients.
-
Antipsychotic agents, including prochlorperazine, are not approved for the treatment of dementia-related psychosis.
Introduction
Propylpiperazine-derivative phenothiazine; conventional (prototypical, first-generation) antipsychotic and antiemetic agent.
Uses for Prochlorperazine (Systemic) (Sedative)
Psychotic Disorders
Symptomatic management of psychotic disorders (i.e., schizophrenia).
Nonpsychotic Anxiety
Short-term management of nonpsychotic anxiety.
Efficacy established in patients with generalized anxiety disorder; not established whether prochlorperazine is useful for the management of other nonpsychotic conditions in which anxiety or manifestations that mimic anxiety are evident (e.g., physical illness, organic mental conditions, agitated depression, character pathologies).
Because of the risks of toxicity, use only as an alternative to other less toxic anxiolytic agents (e.g., benzodiazepines) in most patients.
Nausea and Vomiting
Management of severe nausea and vomiting of various etiologies (e.g., postoperative, acute migraine, toxins, radiation, or cytotoxic drugs).
Not effective in preventing vertigo or motion sickness, or for the management of emesis caused by the action of drugs on the nodose ganglion or locally on the GI tract.
Use not recommended for the prevention and treatment of nausea and vomiting associated with pregnancy except in cases of severe nausea and vomiting so serious and intractable that pharmacologic intervention is required and the potential benefits justify the possible risks to the fetus. (See Fetal/Neonatal Morbidity under Cautions.)
Prochlorperazine (Systemic) (Sedative) Dosage and Administration
General
-
Adjust dosage carefully according to individual requirements and response; use the lowest possible effective dosage.
-
Periodically evaluate patients receiving long-term therapy to determine whether maintenance dosage can be decreased or drug therapy discontinued. (See Tardive Dyskinesia under Cautions.)
Psychotic Disorders
-
Symptomatic relief of psychotic disorders may be seen in many patients during the first 2 days of therapy; however, optimum antipsychotic effect usually requires prolonged administration of the drug.
-
For prompt control of severe psychotic symptoms, administer IM; after symptoms are controlled, oral therapy should replace parenteral therapy at the same dosage level or higher.
Administration
Prochlorperazine edisylate is administered by deep IM injection, direct IV injection, or IV infusion.
Prochlorperazine maleate is administered orally as conventional tablets.
Prochlorperazine is administered rectally.
Sub-Q administration of prochlorperazine edisylate is not recommended because of local irritation.
IV Administration
May be administered undiluted or diluted in isotonic solution.
To minimize hypotension following IV administration, patient should remain in supine position under observation for ≥30 minutes. (See Hypotension under Cautions.)
Rate of Administration
Administer by IV infusion or by direct IV injection at a rate not exceeding 5 mg/minute.
Do not administer as a rapid (“bolus”) injection.
IM Administration
Administer by deep IM injection into the upper outer quadrant of the gluteus maximus.
If possible, avoid IM administration in geriatric patients who are thin or debilitated with reduced muscle mass (injections may be painful and absorption may be erratic or unpredictable).
Dosage
Available as prochlorperazine, prochlorperazine edisylate, or prochlorperazine maleate; dosage expressed in terms of prochlorperazine.
Pediatric Patients
Children should receive the lowest possible effective dosage, and parents should be instructed not to exceed the prescribed dosage.
Use not recommended in children <2 years of age or those weighing <9 kg.
Psychotic Disorders
Oral
Children 2–12 years of age: Initially, 2.5 mg 2 or 3 times daily; total dosage should not exceed 10 mg on first day. May increase dosage according to patient’s therapeutic response and tolerance, but usually should not exceed 20 and 25 mg daily for children 2–5 and 6–12 years of age, respectively.
Dosage for children <2 years of age or those weighing <9 kg not established.
IM
Children <12 years of age: 0.13 mg/kg. Generally, most pediatric patients respond after 1 dose, and oral therapy should replace parenteral therapy at the same dosage level or higher.
Nausea and Vomiting
Oral
|
Weight (kg) |
Daily Dosage |
|---|---|
|
≤9 |
Use not recommended |
|
9.1–13.2 |
2.5 mg once or twice daily |
|
13.6–17.7 |
2.5 mg 2 or 3 times daily |
|
18.2–38.6 |
2.5 mg 3 times daily or 5 mg twice daily |
Alternatively, in children ≥2 years of age and weighing >9 kg: 0.4 mg/kg or 10 mg/m2 daily given in 3 or 4 divided doses.
Generally, it is not necessary to continue therapy for >24 hours.
IM
Children ≥2 years of age and weighing >9 kg: 0.13 mg/kg. Generally, a single dose is sufficient to control nausea and vomiting in most patients.
Adults
Psychotic Disorders
Oral
5 or 10 mg 3 or 4 times daily in office patients and outpatients with relatively mild symptomatology.
Initially, 10 mg 3 or 4 times daily for hospitalized or well-supervised patients with moderate to severe symptomatology. Gradually increase dosage every 2 or 3 days until symptoms are controlled or adverse effects become troublesome. Although some patients exhibit optimum response with 50–75 mg daily, dosages of 100–150 mg daily usually required in more severely disturbed patients.
IM
10–20 mg for prompt control in patients with severe symptomatology; may be necessary to repeat the initial dose every 1–4 hours to control symptoms in some patients. Generally, not more than 3 or 4 doses are required.
10–20 mg every 4–6 hours, if prolonged parenteral therapy is required.
After the patient’s symptoms are controlled, oral therapy should replace parenteral therapy at the same dosage level or higher.
Nonpsychotic Anxiety
Oral
5 mg 3 or 4 times daily for ≤12 weeks.
Nausea and Vomiting
Oral
Usually, 5 or 10 mg 3 or 4 times daily.
Dosages >40 mg daily should be used only in resistant cases.
Rectal
25 mg twice daily.
IV
2.5–10 mg.
For control of severe nausea and vomiting during surgery: 5–10 mg given 15–30 minutes before induction of anesthesia. If necessary, repeat initial dose once before surgery.
To control acute symptoms during or after surgery, usually 5–10 mg, repeated once, if necessary; single IV doses of the drug should not exceed 10 mg.
IM
Initially, 5–10 mg; if necessary, initial dose may be repeated every 3 or 4 hours, but total dosage should not exceed 40 mg daily.
For control of severe nausea and vomiting during surgery: 5–10 mg given 1–2 hours before induction of anesthesia. If necessary, dose may be repeated once, 30 minutes after the initial dose.
To control acute symptoms during or after surgery: 5–10 mg, repeated once in 30 minutes, if necessary.
Prescribing Limits
Pediatric Patients
Psychotic Disorders
Oral
Maximum 10 mg daily for the first day.
Subsequently, maximum 20 and 25 mg daily for children 2–5 and 6–12 years of age, respectively.
Nausea and Vomiting
Oral
|
Weight (kg) |
Maximum Daily Dosage |
|---|---|
|
≤9 |
Use not recommended |
|
9.1–13.2 |
Maximum 7.5 mg daily |
|
13.6–17.7 |
Maximum 10 mg daily |
|
18.2–38.6 |
Maximum 15 mg daily |
Adults
Nonpsychotic Anxiety
Oral
Maximum 20 mg daily; do not administer for >12 weeks.
Nausea and Vomiting
Oral
Dosages >40 mg daily should be used only in resistant cases.
IV
Maximum 10 mg as a single dose. Maximum 40 mg daily (total daily dosage).
IM
Maximum 40 mg daily (total daily dosage).
Special Populations
Geriatric Patients
Generally, select dosage at lower end of recommended range; increase dosage gradually and monitor closely. (See Geriatric Use under Cautions.)
Debilitated or Emaciated Patients
Increase dosage gradually.
Cautions for Prochlorperazine (Systemic) (Sedative)
Contraindications
-
Comatose states or in the presence of large amounts of CNS depressants (e.g., alcohol, barbiturates, opiates). (See Specific Drugs and Laboratory Tests under Interactions.)
-
Pediatric surgery.
-
Children <2 years of age or <9 kg.
-
Children with conditions for which dosage has not been established.
-
Known hypersensitivity to prochlorperazine or other phenothiazines.
Warnings/Precautions
Warnings
Shares the toxic potentials of other phenothiazines; observe the usual precautions of phenothiazine therapy.
Increased Mortality in Geriatric Patients with Dementia-related Psychosis
Increased risk of death with use of either conventional (first-generation) or atypical (second-generation) antipsychotics in geriatric patients with dementia-related psychosis.
Antipsychotic agents, including prochlorperazine, are not approved for the treatment of dementia-related psychosis. (See Increased Mortality in Geriatric Patients with Dementia-related Psychosis in Boxed Warning.)
Extrapyramidal Reactions
Possible extrapyramidal reactions, especially in hospitalized psychiatric patients and in children. Consider dosage reduction or discontinuance, depending on severity of symptoms. An anticholinergic antiparkinsonian agent or diphenhydramine may be given to control persistent or severe reactions.
Signs and symptoms may be similar to those accompanying certain disorders (e.g., encephalitis, Reye’s syndrome, encephalopathy, meningitis, tetanus); diagnosis of these disorders may be obscured or the disease-associated signs and symptoms may be incorrectly diagnosed as drug induced.
Tardive Dyskinesia
Tardive dyskinesia, a syndrome of potentially irreversible, involuntary dyskinetic movements, reported with use of antipsychotic agents.
Reserve long-term antipsychotic treatment for patients with chronic illness known to respond to antipsychotic agents, and for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients requiring chronic treatment, use smallest dosage and shortest duration of treatment producing a satisfactory clinical response; periodically reassess need for continued therapy.
APA recommends assessing patients receiving conventional antipsychotic agents for abnormal involuntary movements every 6 months; for patients at increased risk for tardive dyskinesia, assess every 3 months. Consider discontinuance of prochlorperazine if signs and symptoms of tardive dyskinesia appear. However, some patients may require treatment despite the presence of the syndrome.
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome (NMS), a potentially fatal syndrome characterized by hyperpyrexia, muscle rigidity, altered mental status, and autonomic instability, reported with antipsychotic agents.
Immediately discontinue therapy and initiate supportive and symptomatic therapy if NMS occurs. Careful monitoring recommended if therapy is reinstituted following recovery; the risk that NMS can recur must be considered.
Fetal/Neonatal Morbidity
Safety of use during pregnancy not established. Jaundice, prolonged extrapyramidal signs and symptoms, hyperreflexia, and hyporeflexia reported in some neonates born to women who received phenothiazines during pregnancy.
Risk for extrapyramidal and/or withdrawal symptoms (e.g., agitation, hypertonia, hypotonia, tardive dyskinetic-like symptoms, tremor, somnolence, respiratory distress, feeding disorder) in neonates exposed to antipsychotic agents during the third trimester; monitor neonates exhibiting such symptoms. Symptoms were self-limiting in some neonates but varied in severity; some infants required intensive support and prolonged hospitalization.
Generally, use during pregnancy only when the potential benefits justify the possible risks to the fetus.
Sensitivity Reactions
Possible sensitivity reactions (e.g., cholestatic jaundice, blood dyscrasias, dermatoses, photosensitivity). Use generally not recommended in patients with bone marrow suppression or those with known hypersensitivity to a phenothiazine (unless potential benefits outweigh the possible risks). (See Hematologic Effects under Cautions.)
Contact dermatitis occurs rarely following skin contact with prochlorperazine edisylate injection; use care to avoid skin contact with injection.
General Precautions
Hematologic Effects
Leukopenia, neutropenia, and agranulocytosis temporally related to antipsychotic agents reported during clinical trial and/or postmarketing experience.
Possible risk factors for leukopenia and neutropenia include preexisting low WBC count and a history of drug-induced leukopenia or neutropenia. Monitor CBC frequently during the first few months of therapy in patients with such risk factors. Discontinue prochlorperazine at the first sign of a decline in WBC count in the absence of other causative factors.
Carefully monitor patients with neutropenia for fever or other signs and symptoms of infection and treat promptly if they occur. In patients with severe neutropenia (ANC <1000/mm3), discontinue prochlorperazine and monitor WBC until recovery occurs.
CNS Depression
May impair mental and/or physical abilities, especially during the first few days of therapy; use caution with activities requiring alertness (e.g., operating vehicles or machinery).
Because of CNS depressant effects, use with caution in patients with chronic respiratory disorders (e.g., severe asthma, emphysema, acute respiratory tract infections).
Hypotension
Possible hypotension; large dosages and parenteral administration should be used with caution in patients with severe cardiovascular disorders.
To minimize hypotension following injection, patient should remain in supine position under observation for ≥30 minutes.
If hypotension occurs, place patient in Trendelenburg’s position and, if required, administer norepinephrine or phenylephrine; epinephrine or dopamine should not be used. (See Specific Drugs and Laboratory Tests under Interactions.)
Prolactin Secretion
Increased serum prolactin concentrations; may be associated with galactorrhea, menstrual cycle changes (e.g., oligomenorrhea, amenorrhea), and gynecomastia.
Since approximately one-third of human breast cancers are prolactin dependent, use with caution in patients with previously detected breast cancer.
Mutagenicity
Chromosomal aberrations in spermatocytes and abnormal sperm have been demonstrated in rodents.
Anticholinergic Effects
Possible anticholinergic effects (e.g., dry mouth, blurred vision, mydriasis, constipation, nausea, adynamic ileus, atonic colon, urinary retention, decreased sweating, impotence).
Use with caution in patients with glaucoma or prostatic hypertrophy.
Body Temperature Regulation
Phenothiazines depress the hypothalamic mechanism for body temperature regulation; possible hyperthermia or hypothermia when exposed to temperature extremes.
Use with caution in patients exposed to extreme heat or cold.
Surgery
Possible suppression of the cough reflex and aspiration of gastric contents. Use caution in postoperative patients.
Other Precautions
Antiemetic effects may mask signs of overdosage of other drugs (e.g., antineoplastic agents) or obscure the cause of vomiting in various disorders (e.g., intestinal obstruction, brain tumor, Reye’s syndrome). (See Extrapyramidal Reactions under Cautions.)
Use phenothiazines with caution in patients with hypocalcemia, since susceptibility to dystonic reactions may be increased.
Specific Populations
Pregnancy
Category C. (See Fetal/Neonatal Morbidity under Cautions.)
Lactation
Distributed into milk. Caution if used in nursing women.
Pediatric Use
Safety and efficacy not established in children <2 years of age or those weighing <9 kg. (See Contraindications.)
Avoid use in children and adolescents with suspected Reye’s syndrome, since the antiemetic and potential extrapyramidal effects produced by the drug may obscure the diagnosis of or be confused with CNS manifestations of this condition. (See Extrapyramidal Reactions under Cautions.)
Not recommended for use in children during surgery or in conditions for which pediatric dosage has not been established. (See Contraindications.)
Incidence of extrapyramidal reactions appears to be relatively high in children. Children with acute illnesses (e.g., varicella-zoster [chickenpox] infections, CNS infections, measles, gastroenteritis) or dehydration appear to be at increased risk of such reactions (particularly dystonic reactions and akathisia); use only under close supervision in these patients.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults.
Geriatric patients appear to be particularly sensitive to adverse CNS (e.g., tardive dyskinesia, parkinsonian manifestations, akathisia, sedation), anticholinergic, and cardiovascular (e.g., orthostatic hypotension) effects of antipsychotic agents. (See Tardive Dyskinesia and also Hypotension and also Anticholinergic Effects, under Cautions.) Possible increased incidence of agranulocytosis in geriatric patients receiving prochlorperazine. (See Hematologic Effects under Cautions.)
Geriatric patients with dementia-related psychosis treated with either conventional or atypical antipsychotic agents are at an increased risk of death. (See Increased Mortality in Geriatric Patients with Dementia-related Psychosis in Boxed Warning.)
Use with caution. (See Geriatric Patients under Dosage and Administration.)
Hepatic Impairment
Use with caution.
Renal Impairment
Use with caution.
Common Adverse Effects
Drowsiness, dizziness, amenorrhea, blurred vision, skin reactions, hypotension.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Anticholinergic drugs (e.g., atropine) |
Possible potentiation of anticholinergic effects |
Use with caution |
|
Anticoagulants, oral |
Potential decreased effect of oral anticoagulants |
|
|
Anticonvulsants (e.g., phenytoin) |
Prochlorperazine may lower seizure threshold Prochlorperazine may interfere with phenytoin metabolism and precipitate phenytoin toxicity |
Dosage adjustments of anticonvulsants may be necessary |
|
CNS depressants (e.g., alcohol, anesthetics, opiates) |
May potentiate CNS depression |
Use with caution to avoid excessive sedation or CNS depression |
|
Epinephrine or dopamine |
Concomitant use may cause further lowering of BP |
Do not use epinephrine or dopamine to treat phenothiazine-induced hypotension (see Hypotension under Cautions) |
|
Guanethidine and related compounds |
Potential for decreased effectiveness of guanethidine and related compounds |
|
|
Lithium |
Possible acute encephalopathic syndrome, especially with high serum lithium concentrations |
Observe patients receiving combined therapy for evidence of adverse neurologic effects; discontinue treatment promptly if such signs or symptoms appear |
|
Propranolol |
Increased plasma concentrations of prochlorperazine and propranolol |
|
|
Test for phenylketonuria (PKU) |
Potential false positive test results |
|
|
Thiazide diuretics |
Potential for increased orthostatic hypotension |
Prochlorperazine (Systemic) (Sedative) Pharmacokinetics
Absorption
Bioavailability
Phenothiazines are generally well absorbed from the GI tract and from parenteral sites.
Onset
Psychotic disorders: Symptomatic relief may be seen during the first 2 days of oral therapy; however, optimum antipsychotic effect usually requires prolonged administration.
Antiemetic effects: Onset in 30–40 minutes (conventional tablet), 60 minutes (rectal suppository), or 10–20 minutes (IM administration).
Duration
Antiemetic effects: Duration of 3–4 hours (conventional tablet, rectal suppository, or IM administration).
Distribution
Extent
Phenothiazines are distributed into most body tissues and fluids, with high concentrations being distributed into the brain, lungs, liver, kidneys, and spleen.
Phenothiazines cross the placenta. Prochlorperazine is distributed into milk.
Plasma Protein Binding
Phenothiazines are highly bound to plasma proteins.
Elimination
Metabolism
Extensively metabolized, principally in the liver.
Elimination Route
Phenothiazines and their metabolites are excreted in urine and feces.
Stability
Storage
Rectal
Suppositories
20–25°C. Do not remove from wrapper until ready to use.
Oral
Tablets
20–25°C. Protect from light.
Parenteral
Injection
20–25°C; do not freeze. Protect from light.
Actions
-
Exhibits weak anticholinergic effects, moderate sedative effects, strong extrapyramidal effects, and strong antiemetic effects.
-
May antagonize dopamine-mediated neurotransmission at the synapses and may block postsynaptic dopamine receptor sites; however, precise mechanism(s) of action have not been determined.
-
Exerts an antiemetic effect by directly affecting the medullary chemoreceptor trigger zone (CTZ), apparently by blocking dopamine receptors in the CTZ. Inhibits apomorphine-induced vomiting.
-
Also has peripheral and/or central antagonistic activity against α-adrenergic, serotonergic, histaminic H1, and muscarinic receptors.
Advice to Patients
-
Importance of advising patients and caregivers that elderly patients with dementia-related psychosis treated with antipsychotic agents are at an increased risk of death. Patients and caregivers also should be informed that prochlorperazine is not approved for treating elderly patients with dementia-related psychosis.
-
Potential for drug to impair mental alertness or physical coordination; use caution when driving or operating machinery until effects on individual are known.
-
Importance of clinicians informing patients of risk of extrapyramidal reactions and providing reassurance that these reactions usually can be controlled by administration of antiparkinsonian drugs (e.g., benztropine) and by subsequent dosage reduction.
-
Importance of informing patients and caregivers about the risk of NMS, which can cause high fever, stiff muscles, sweating, fast or irregular heart beat, change in BP, confusion, and kidney damage.
-
Importance of clinicians informing patients in whom chronic use is contemplated of risk of tardive dyskinesia, taking into account clinical circumstances and competency of patient to understand information provided.
-
Importance of avoiding exposure to temperature extremes.
-
Risk of leukopenia, neutropenia, and agranulocytosis. Importance of advising patients with a preexisting low WBC count or history of drug-induced leukopenia/neutropenia that their CBC count should be monitored during prochlorperazine therapy.
-
Importance of informing clinician if sore throat or other signs of infection occur.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses (e.g., cardiovascular disease, seizures).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Importance of clinicians informing patients about the benefits and risks of taking antipsychotics during pregnancy (see Fetal/Neonatal Morbidity under Cautions). Importance of advising patients not to stop taking prochlorperazine if they become pregnant without consulting their clinician; abruptly stopping antipsychotic agents may cause complications.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Rectal |
Suppositories |
25 mg* |
Compro |
Paddock |
|
Prochlorperazine Suppositories |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection |
5 mg (of prochlorperazine) per mL* |
Prochlorperazine Edisylate Injection |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
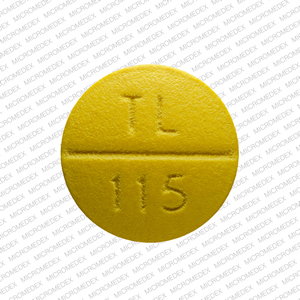
Oral |
Tablets, film-coated |
5 mg (of prochlorperazine)* |
Prochlorperazine Maleate Tablets |
|
|
10 mg (of prochlorperazine)* |
Prochlorperazine Maleate Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 15, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about prochlorperazine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (461)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: phenothiazine antiemetics
- Breastfeeding
Patient resources
Professional resources
- Prochlorperazine, Prochlorperazine Edisylate, Prochlorperazine Maleate (Systemic) (Antiemetic) monograph
- Prochlorperazine (FDA)
- Prochlorperazine Injection (FDA)
- Prochlorperazine Suppository (FDA)
- Prochlorperazine Tablets (FDA)