Pindolol (Monograph)
Drug class: beta-Adrenergic Blocking Agents
Introduction
A nonselective β-adrenergic blocking agent (β-blocker).
Uses for Pindolol
Hypertension
Management of hypertension (alone or in combination with other classes of antihypertensive agents).
β-Blockers generally not preferred for first-line therapy of hypertension according to current evidence-based hypertension guidelines, but may be considered in patients who have a compelling indication (e.g., prior MI, ischemic heart disease, heart failure) for their use or as add-on therapy in those who do not respond adequately to the preferred drug classes (ACE inhibitors, angiotensin II receptor antagonists, calcium-channel blockers, or thiazide diuretics). A 2017 ACC/AHA multidisciplinary hypertension guideline states that β-blockers used for ischemic heart disease that are also effective in lowering BP include bisoprolol, carvedilol, metoprolol succinate, metoprolol tartrate, nadolol, propranolol, and timolol.
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
The 2017 ACC/AHA hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Other hypertension guidelines generally have based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment is recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg. Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Black hypertensive patients generally tend to respond better to monotherapy with calcium-channel blockers or thiazide diuretics than to β-blockers. However, diminished response to β-blockers is largely eliminated when administered concomitantly with a thiazide diuretic.
Chronic Stable Angina
Management of chronic stable angina pectoris† [off-label].
β-Blockers are recommended as first-line anti-ischemic drugs in most patients with chronic stable angina; despite differences in cardioselectivity, intrinsic sympathomimetic activity, and other clinical factors, all β-blockers appear to be equally effective for this use.
Pindolol Dosage and Administration
General
-
Individualize dosage according to patient response and tolerance.
-
If long-term therapy is discontinued, reduce dosage gradually over a period of about 1–2 weeks. (See Abrupt Withdrawal of Therapy under Cautions.)
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, calcium-channel blocker, thiazide diuretic). Many patients will require ≥2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved, add a third drug.
Administration
Oral Administration
Administer orally, usually twice daily; bioavailability does not appear to be affected by food. (See Absorption under Pharmacokinetics.)
Dosage
Adults
Hypertension
Oral
Initially, 5 mg twice daily, either alone or in combination with other antihypertensives. Increase dosage gradually by 10 mg daily at 3- to 4-week intervals as necessary up to 60 mg daily. Some experts state usual maintenance dosage range is 10–60 mg daily, given in 2 divided doses.
Chronic Stable Angina† [off-label]
Oral
15–40 mg daily, given in 3 or 4 divided doses.
Prescribing Limits
Adults
Hypertension
Oral
Maximum 60 mg daily.
Special Populations
Hepatic Impairment
Dosage must be modified in response to the degree of hepatic impairment.
Cautions for Pindolol
Contraindications
-
Bronchial asthma, heart block greater than first degree, cardiogenic shock, overt cardiac failure, or severe bradycardia.
Warnings/Precautions
Warnings
Heart Failure
Possible precipitation of CHF.
Avoid use in patients with decompensated heart failure, may use cautiously in patients with well-compensated heart failure (e.g., those controlled with ACE inhibitors, cardiac glycosides, and/or diuretics).
Adequate treatment (e.g., with a cardiac glycoside and/or diuretic) and close observation recommended if signs or symptoms of impending heart failure occur; if heart failure continues, discontinue therapy, gradually if possible.
Abrupt Withdrawal of Therapy
Abrupt discontinuance of therapy is not recommended as it may exacerbate angina symptoms or precipitate MI in patients with CAD. Gradually decrease dosage over a period of about 1–2 weeks. Monitor patients carefully and advise to temporarily limit their physical activity. If exacerbation of angina occurs, reinstitute therapy promptly, and initiate appropriate measures for the management of unstable angina pectoris.
Bronchospastic Disease
Possible inhibition of bronchodilation produced by endogenous catecholamines.
Generally should not be used in patients with bronchospastic disease, but may be used with caution in patients with nonallergic bronchospasm (e.g., chronic bronchitis, emphysema). (See Contraindications under Cautions.)
Major Surgery
Possible risks associated with general anesthesia (e.g., severe hypotension, difficulty maintaining heart beat) due to decreased ability of the heart to respond to reflex β-adrenergic stimuli. Use with caution in patients undergoing major surgery involving general anesthesia.
Diabetes and Hypoglycemia
Possible decreased signs and symptoms of hypoglycemia (e.g., tachycardia, palpitation, BP changes, tremor, feelings of anxiety, but not sweating or dizziness).
Use with caution in patients with diabetes mellitus receiving hypoglycemic drugs.
Thyrotoxicosis
Signs of hyperthyroidism (e.g., tachycardia) may be masked. Possible thyroid storm if therapy is abruptly withdrawn; carefully monitor patients having or suspected of developing thyrotoxicosis.
Sensitivity Reactions
Anaphylactic Reactions
Possible increased reactivity to repeated, accidental, diagnostic, or therapeutic challenges with a variety of allergens while taking β-blockers in patients with a history of anaphylactic reactions to a variety of allergens. Such patients may be unresponsive to usual doses of epinephrine.
Specific Populations
Pregnancy
Category B.
Lactation
Distributed into milk. Use not recommended.
Pediatric Use
Safety and efficacy not established.
Hepatic Impairment
Hepatic elimination; use with caution.
Common Adverse Effects
Insomnia, dizziness, fatigue, nervousness, bizarre dreams or increased dreaming, weakness, paresthesia, edema, dyspnea, muscle pain, joint pain, chest pain, muscle cramps, nausea, abdominal discomfort, pruritus.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Aspirin |
Pharmacokinetic interaction unlikely |
|
|
Digoxin |
Possible decreases in serum digoxin concentrations |
Not considered clinically important |
|
Reserpine |
Additive effects |
Monitor for signs of hypotension and bradycardia (e.g., vertigo, syncope, postural hypotension) |
|
Hypotensive agents (hydralazine, hydrochlorothiazide) |
Possible increased hypotensive effects |
Adjust dosage carefully |
|
Thioridazine |
Increased serum concentrations of thioridazine and metabolites; higher than expected serum concentrations of pindolol Increased thioridazine concentrations may cause prolongation of the QTc interval and a possible increase in the risk of serious, potentially fatal cardiac arrhythmia (e.g., torsades de pointes) |
Concomitant use is contraindicated |
|
Warfarin |
Pharmacokinetic interaction unlikely |
Pindolol Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from the GI tract with peak plasma concentrations reached within 1–2 hours.
Bioavailability 50 –95%.
Onset
Effect on heart rate is seen within 3 hours.
Hypotensive effect is usually seen within 1 week, but maximum therapeutic response may not be observed until 2 weeks or longer.
Duration
Acute hemodynamic effects persist for 24 hours after administration.
Food
Food may increase the rate, but not the extent of absorption.
Special Populations
Bioavailability may be at the lower end of the range in uremic patients; extent of absorption may be decreased in patients with impaired renal function.
Distribution
Extent
Distributed into milk.
Plasma Protein Binding
Approximately 40–60%.
Elimination
Metabolism
Extensively metabolized in the liver (approximately 60–65%) to metabolites.
Elimination Route
Excreted in urine (35–50%) unchanged.
Half-life
3–4 hours.
Special Populations
In patients with creatinine clearances <20 mL/minute, <15% is excreted in urine unchanged.
In patients with renal failure, plasma half-life is 3–11.5 hours.
In geriatric patients, plasma half-life is 7–15 hours.
In patients with hepatic cirrhosis, half-life is 2.5–30 hours.
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at 15–30°C.
Actions
-
Inhibits response to adrenergic stimuli by competitively blocking β-adrenergic receptors within the myocardium (β1-receptors) and within bronchial and vascular smooth muscle (β2-receptors).
-
In addition, causes slight activation of the β-receptors, making the drug a partial β-agonist.
-
At higher than therapeutically obtained plasma concentrations, the drug has membrane-stabilizing activity or a quinidine-like effect.
-
Decreases stress- and exercise-stimulated heart rate. Has a lesser effect on resting heart rate (usually decreasing resting heart rate only by about 4–8 bpm or not at all), slowing of conduction in the AV node, and cardiac output, than do β-blockers that do not possess intrinsic sympathomimetic activity (ISA).
-
The precise mechanism of hypotensive effect has not been determined; the drug does not consistently affect cardiac output or renin release, and other mechanisms (e.g., decreased peripheral resistance) probably contribute to its hypotensive effect.
-
May increase airway resistance, depending on the patient’s pretreatment sympathetic tone; patients with high pretreatment tone show a decrease in forced expiratory volume in 1 second (FEV1), whereas those with low pretreatment tone may show little, if any, change in FEV1.
Advice to Patients
-
Importance of taking pindolol exactly as prescribed.
-
Importance of not interrupting or discontinuing therapy without consulting clinician.
-
Importance of immediately informing clinician at the first sign or symptom of impending cardiac failure (e.g., weight gain, increased shortness of breath) or if any difficulty in breathing occurs.
-
In patients with heart failure, importance of informing clinician of signs or symptoms of exacerbation (e.g., weight gain, difficulty in breathing).
-
Importance of patients informing anesthesiologist or dentist that they are receiving pindolol therapy prior to undergoing major surgery.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
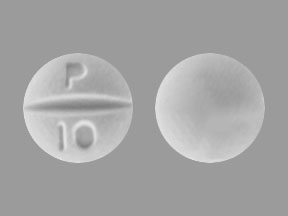
Oral |
Tablets |
5 mg* |
Pindolol Tablets |
|
|
10 mg* |
Pindolol Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about pindolol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (3)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: non-cardioselective beta blockers
- Breastfeeding
- En español