The originating document has been archived. We cannot confirm the completeness, accuracy, or currency of the content.
Losartan Potassium (Monograph)
Brand name: Cozaar
Drug class: Angiotensin II Receptor Antagonists
Warning
-
May cause fetal toxicity.
-
When pregnancy is detected, discontinue as soon as possible. Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus.
Introduction
Angiotensin II receptor type 1 (AT1) antagonist (i.e., angiotensin II receptor blocker, ARB).
Uses for Losartan Potassium
Hypertension
Management of hypertension (alone or in combination with other classes of antihypertensive agents, including diuretics). Monotherapy used to treat hypertension in adults and pediatric patients ≥6 years of age.
Angiotensin II receptor antagonists are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines. While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.
Stroke Reduction in Left Ventricular Hypertrophy
Reduction of the risk of stroke in patients with hypertension and left ventricular hypertrophy.
Evidence suggests that the benefit associated with losartan-based antihypertensive therapy does not apply to Black patients.
Preliminary evidence suggests that aspirin therapy at baseline in patients receiving losartan may reduce the risk of combined cardiovascular death, stroke, and acute MI compared with aspirin therapy at baseline in patients receiving atenolol.
Diabetic Nephropathy
Management of diabetic nephropathy manifested by elevated Scr and proteinuria (urinary albumin to creatinine ratio ≥300 mg/g) in patients with type 2 diabetes mellitus and hypertension.
Recommended option in patients with diabetes mellitus, hypertension, and moderately to severely elevated albuminuria (i.e., urine to creatinine ratio >30 mg/g). May also be considered in patients with diabetes and albuminuria who are normotensive† [off-label] .
Angiotensin II receptor antagonists have been used in the management of nondiabetic CKD with moderately or severely increased albuminuria† [off-label] to prevent progression of CKD.
Use may be considered in patients with CKD and normal to mildly increased albuminuria† [off-label] (i.e., urinary albumin to creatinine ratio <30 mg/g) when other compelling indications (e.g., hypertension, heart failure, or low ejection fraction) present.
Heart Failure
Angiotensin II receptor antagonists have been used in the management of heart failure† [off-label].
Current guidelines on management of heart failure recommend ACE inhibitors for treatment of patients with presymptomatic heart failure (i.e., Stage B disease) who have a left ventricular ejection fraction (LVEF) ≤40%; angiotensin II receptor antagonists may be used in such patients with a recent MI who are intolerant to ACE inhibitors. Angiotensin receptor-neprilysin inhibitors (ARNIs) are recommended first-line for treatment of symptomatic heart failure with reduced ejection fraction (HFrEF); angiotensin II receptor antagonists are only recommended when an ARNI is contraindicated, inaccessible, or poorly tolerated. Angiotensin II receptor antagonists may be considered in patients with a LVEF between 41–49% to reduce the risk of hospitalizations for heart failure and cardiovascular mortality.
Mortality Reduction After Acute MI
Used to improve survival in hemodynamically stable patients with acute MI† [off-label] .
Expert guidelines recommend initiation of an oral ACE inhibitor within the first 24 hours of acute MI in patients with an anterior infarct, heart failure, or ejection fraction ≤40% who do not have any contraindications (e.g., hypotension, shock, renal dysfunction). In patients who are intolerant to ACE inhibitors, an angiotensin II receptor antagonist is recommended, and has been shown to have similar benefits on survival.
Losartan Potassium Dosage and Administration
General
Pretreatment Screening
-
Verify pregnancy status in females of reproductive potential.
-
Evaluate and correct sodium or volume depletion.
Patient Monitoring
-
Monitor blood pressure.
-
Monitor renal function periodically.
-
Monitor serum potassium periodically.
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) includes Cozaar (losartan potassium), Colace (docusate sodium), and Zocor (simvastatin) on their ISMP List of Confused Drug Names, and recommends using special safeguards to ensure the accuracy of prescriptions for these drugs.
Other General Considerations
-
May administer with other antihypertensive agents.
-
Blood pressure control should be part of a comprehensive cardiovascular risk management plan, including (as appropriate) lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake.
Administration
Oral Administration
Administer orally without regard to meals. Available as tablets. Also commercially available in fixed-combination tablets containing losartan potassium and hydrochlorothiazide; see the full prescribing information for administration of this combination product.
Preparation of an Oral Suspension from Losartan Tablets
Administer extemporaneously prepared oral suspension in patients unable to swallow tablets. Preparation of extemporaneous suspension containing losartan potassium 2.5 mg/mL: Add 10 mL of purified water to a 240-mL amber polyethylene terephthalate (PET) bottle containing ten 50-mg tablets of losartan potassium; shake contents for ≥2 minutes. Allow concentrated suspension to stand for 1 hour following reconstitution, then shake for an additional minute. Separately, prepare a mixture containing equal parts (by volume) of syrup (Ora-Sweet SF) and suspending vehicle (Ora-Plus). Dilute the concentrated suspension of losartan potassium with 190 mL of the Ora-Sweet SF and Ora-Plus mixture; shake the container an additional minute to disperse ingredients. Shake suspension before dispensing each dose.
Dosage
Available as losartan potassium; dosage expressed in terms of the salt.
Pediatric Patients
Hypertension
Oral
Children ≥6 years of age: Initially, 0.7 mg/kg (up to 50 mg) once daily. .Adjust dosage based on BP response.
Dosages >1.4 mg/kg (or >100 mg) daily not studied in pediatric patients.
Adults
Hypertension
Oral
Adults without intravascular volume depletion: 50 mg once daily initially. May increase to 100 mg once daily if needed for BP control.
Adults with possible depletion of intravascular volume (e.g., on diuretic therapy): 25 mg once daily initially.
Stroke Reduction in Left Ventricular Hypertrophy
Oral
50 mg once daily initially. Depending on BP response, add hydrochlorothiazide 12.5 mg daily and/or increase losartan dosage to 100 mg once daily.
Diabetic Nephropathy
Oral
50 mg once daily initially; may increase to 100 mg once daily based on BP response.
Heart Failure†
Oral
25–50 mg once daily initially; target dosage of 150 mg daily.
Special Populations
Hepatic Impairment
Mild to moderate hepatic impairment: initiate at 25 mg once daily.
Severe hepatic impairment: not studied.
Renal Impairment
No dosage adjustment necessary for adults with renal impairment unless volume depleted.
Not recommended for use in pediatric patients with eGFR <30 mL/minute per 1.73 m2.
Geriatric Patients
No dosage recommendations at this time.
Cautions for Losartan Potassium
Contraindications
-
Known hypersensitivity to losartan or any ingredient in the formulation.
-
Concomitant therapy with aliskiren in patients with diabetes mellitus.
Warnings/Precautions
Warnings
Fetal/Neonatal Morbidity and Mortality
Risk of fetal harm when administered to a pregnant woman (See Boxed Warning). Possible reduction in fetal renal function and increase in fetal and neonatal morbidity and mortality when drugs that act on the renin-angiotensin system (RAS) are used during the second and third trimesters of pregnancy. Oligohydramnios caused by drugs that act on the RAS can result in fetal lung hypoplasia, skeletal deformations (including skull hypoplasia), anuria, hypotension, renal failure, and death. Discontinue losartan immediately when pregnancy detected. If there is no appropriate alternative therapy, apprise the mother of the potential risk to the fetus. If losartan is taken during pregnancy, perform serial ultrasound examinations to assess intra-amniotic environment; if oligohydramnios observed, discontinue losartan, unless it is considered life-saving for the mother. Oligohydramnios may not appear until after irreversible injury to the fetus. Closely observe neonates exposed to losartan in utero for signs of hypotension, oliguria, and hyperkalemia. If oliguria or hypotension occurs, support BP and renal perfusion. Exchange transfusions or dialysis may be required.
Other Warnings and Precautions
Hypotension in Volume- or Salt-Depleted Patients
Possible symptomatic hypotension, particularly in volume- and/or salt-depleted patients (e.g., those treated with diuretics). Correct volume or salt depletion prior to losartan administration.
Renal Function Deterioration
Changes in renal function, including acute renal failure, possible. Patients with renal artery stenosis, CKD, severe congestive heart failure, or volume depletion at higher risk of acute renal failure.
Monitor renal function periodically. Consider withholding or discontinuing losartan in patients who develop a clinically important reduction in renal function while receiving losartan.
Hyperkalemia
Hyperkalemia can develop with concomitant use of agents that increase serum potassium concentration (e.g., potassium-sparing diuretics, potassium supplements, potassium-containing salt substitutes).
Monitor serum potassium periodically and treat appropriately. Dosage reduction or discontinuation of therapy may be required.
Use of Fixed Combinations
When losartan is used in fixed combination with hydrochlorothiazide, the cautions, precautions, and contraindications associated with both drugs must be considered. Consult the full prescribing information for the fixed combination preparation for specific information.
Specific Populations
Pregnancy
May cause fetal harm when administered to a pregnant woman. Possible reduction in fetal renal function and increase in fetal and neonatal morbidity and mortality when drugs that act on the RAS are used during the second and third trimesters of pregnancy. Oligohydramnios caused by drugs that act on the RAS can result in fetal lung hypoplasia, skeletal deformations (including skull hypoplasia), anuria, hypotension, renal failure, and death.
Discontinue losartan immediately when pregnancy detected. If no appropriate alternative exists, apprise the mother of the potential risk to the fetus. If losartan is taken during pregnancy, perform serial ultrasound examinations to assess intra-amniotic environment; if oligohydramnios observed, discontinue losartan, unless it is considered life-saving for the mother. Oligohydramnios may not appear until after irreversible injury to the fetus. Closely observe neonates exposed to losartan in utero for signs of hypotension, oliguria, and hyperkalemia. If oliguria or hypotension occurs, support BP and renal perfusion. Exchange transfusions or dialysis may be required.
Lactation
Losartan and its active metabolite are distributed into milk in rats; not known whether distributed into human milk. Discontinue breastfeeding or the drug.
Pediatric Use
Antihypertensive effects of losartan established in hypertensive pediatric patients 6–16 years of age.
Safety and efficacy not established in children <6 years of age or in pediatric patients with glomerular filtration rate <30 mL/minute per 1.73 m2.
Geriatric Use
No substantial differences in pharmacokinetics, safety, or efficacy of losartan monotherapy relative to younger adults, but increased sensitivity cannot be ruled out.
Hepatic Impairment
Systemic exposure to losartan and its active metabolite may be increased. Initial dosage adjustment recommended in mild to moderate hepatic impairment; losartan not studied in severe hepatic impairment.
Renal Impairment
Plasma concentrations and AUCs of losartan and its active metabolite increased and renal clearance reduced in patients with mild (Clcr 50–74 mL/minute) or moderate (Clcr 30–49 mL/minute) renal insufficiency. Not removed by hemodialysis. No dosage adjustments recommended in patients with renal impairment unless they are also volume depleted.
Black Patients
BP reduction may be smaller in Black patients. No evidence that the benefits of losartan in reducing the risk of cardiovascular events in hypertensive patients with left ventricular hypertrophy apply to Black patients.
Common Adverse Effects
Adverse effects (incidence ≥2%) include dizziness, upper respiratory infection, nasal congestion, back pain.
Drug Interactions
In vitro studies indicate CYP2C9 and 3A4 are involved in biotransformation of losartan to active and inactive metabolites.
Drugs Affecting Hepatic Microsomal Enzymes
Pharmacodynamic consequences of concomitant use of losartan and CYP2C9 inhibitors have not been studied.
Drugs Increasing Serum Potassium
Hyperkalemia may occur with concomitant administration of losartan and other drugs that raise serum potassium levels. Monitor serum potassium levels if used concomitantly.
Specific Drugs
|
Drug |
Interaction |
Comment |
|---|---|---|
|
ACE inhibitors |
Increased risk of renal impairment, hyperkalemia, and hypotension |
Generally avoid concomitant use Monitor BP, renal function, and electrolytes if used concomitantly |
|
Aliskiren |
Increased risk of renal impairment, hyperkalemia, and hypotension |
Generally avoid concomitant use Monitor BP, renal function, and electrolytes if used concomitantly Concomitant use contraindicated in patients with diabetes mellitus Avoid concomitant use in patients with GFR <60 mL/minute |
|
Angiotensin II receptor antagonists |
Increased risk of renal impairment, hyperkalemia, and hypotension |
Generally avoid concomitant use Monitor BP, renal function, and electrolytes if used concomitantly |
|
Cimetidine |
Pharmacokinetic interaction unlikely |
|
|
Digoxin |
Pharmacokinetic interaction unlikely |
|
|
Erythromycin |
Losartan AUC increased by 30%; no impact on conversion of losartan to active metabolite |
|
|
Fluconazole |
Decreased AUC of active metabolite of losartan by approximately 40% and increased losartan AUC by approximately 70% |
|
|
Hydrochlorothiazide |
Pharmacokinetic interaction unlikely |
|
|
Ketoconazole |
Conversion of losartan to its active metabolite unaffected |
|
|
Lithium |
Increased serum lithium concentrations, potentially leading to lithium toxicity |
Carefully monitor serum lithium concentrations |
|
NSAIAs (including COX-2 inhibitors) |
Attenuated hypotensive effects may be observed Possible deterioration of renal function, including possible acute renal failure, in patients who are elderly, volume-depleted (including those receiving concomitant diuretic therapy), or with compromised renal function. Effects usually reversible. |
Monitor renal function periodically during concomitant use |
|
Phenobarbital |
Pharmacokinetic interaction unlikely |
|
|
Rifampin |
Decreased AUCs of losartan and its active metabolite by 30 and 40%, respectively |
|
|
Warfarin |
Pharmacokinetic interaction unlikely |
Losartan Potassium Pharmacokinetics
Absorption
Bioavailability
Well absorbed after oral administration but undergoes substantial first-pass metabolism.
Systemic bioavailability of losartan is about 33%.
Peak plasma concentrations of losartan and its active metabolite attained at 1 and 3–4 hours, respectively, following oral administration.
Onset
Antihypertensive effect evident within 1 week, with maximum BP reduction after 3–6 weeks.
Food
Food slows absorption of losartan and decreases its peak plasma concentration but has minimal effect on AUC of losartan or its active metabolite.
Special Populations
In patients with hepatic impairment, oral bioavailability is about 2 times higher than in those with normal hepatic function.
In patients with mild to moderate alcoholic cirrhosis, plasma concentration of losartan and its active metabolite were about 5 and 1.7 times those of healthy individuals, respectively.
In patients with mild (Clcr 50–74 mL/minute) or moderate (Clcr 30–49 mL/minute) renal impairment, plasma concentrations and AUC of losartan and its active metabolite are increased by 50–90%.
Distribution
Extent
Crosses the blood-brain barrier poorly in animals.
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
Losartan and its active metabolite highly protein bound (plasma free fractions: 1.3 and 0.2%, respectively).
Elimination
Metabolism
CYP2C9 and 3A4 involved in metabolism of losartan.
Elimination Route
Urine: 35% (4% unchanged, 6% active metabolite)
Feces (via bile): 60%
Half-life
Losartan terminal half-life: 2 hours.
Active metabolite: 6-9 hours.
Special Populations
In patients with mild to moderate alcoholic cirrhosis, total plasma clearance of losartan is about 50% lower than in those with normal hepatic function.
In patients with mild or moderate renal impairment, renal clearance of losartan and its active metabolite is decreased by 55–85%. Neither losartan nor its active metabolite is removed by hemodialysis.
Stability
Storage
Oral
Extemporaneous Suspension
2.5-mg/mL preparation of losartan potassium tablets in a mixture of syrup (Ora-Sweet SF) and suspending vehicle (Ora-Plus) : Up to 4 weeks at 2–8°C.
Tablets
25°C (excursions permitted between 15–30°C). Protect from light.
Actions
-
Nonpeptide tetrazole derivative; reversible, non-competitive inhibitor of the angiotensin II receptor (type AT1).
-
Losartan (prodrug) requires activation in the liver to exert pharmacologic activity
-
Active carboxylic acid metabolite is 10-40 times more potent by weight than losartan and appears to be a reversible, noncompetitive inhibitor of the AT1 receptor.
-
Blocks the physiologic actions of angiotensin II, including vasoconstrictor and aldosterone-secreting effects.
-
Does not inhibit ACE; does not bind to or block other hormone receptors or ion channels known to be important in cardiovascular regulation.
Advice to Patients
-
Advise patients not to use potassium supplements or salt substitutes containing potassium without consulting their clinician.
-
Advise females of reproductive potential on the risks of losartan use during pregnancy. Discuss treatment options with women planning to become pregnant.
-
Advise patients to inform their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
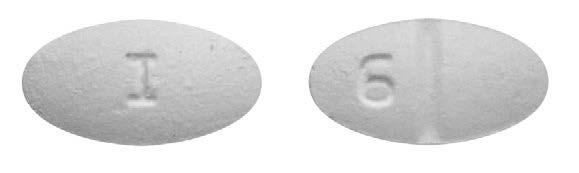
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
25 mg* |
Cozaar |
Organon LLC |
|
Losartan Tablets |
||||
|
50 mg* |
Cozaar |
Organon LLC |
||
|
Losartan Tablets |
||||
|
100 mg* |
Cozaar |
Organon LLC |
||
|
Losartan Tablets |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
50 mg with Hydrochlorothiazide 12.5 mg* |
Hyzaar |
Organon LLC |
|
Losartan with Hydrochlorothiazide Tablets |
||||
|
100 mg with Hydrochlorothiazide 12.5 mg* |
Hyzaar |
Organon LLC |
||
|
Losartan with Hydrochlorothiazide Tablets |
||||
|
100 mg with Hydrochlorothiazide 25 mg* |
Hyzaar |
Organon LLC |
||
|
Losartan with Hydrochlorothiazide Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions January 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Does Losartan block COVID-19 Coronavirus Receptors?
- Can you eat bananas when taking losartan?
- Losartan vs Valsartan - What's the difference between them?
- Does losartan cause rapid heart rate, irregular heartbeat or low blood pressure?
- Are losartan and losartan potassium the same or different drugs?
More about losartan
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (582)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: angiotensin receptor blockers
- Breastfeeding
- En español