Dexmethylphenidate
Brand name: Focalin
Drug class: Respiratory and CNS Stimulants
VA class: CN802
Chemical name: (αR,2R)-α-Phenyl-2-piperidineacetic acid methyl ester hydrochloride
Molecular formula: C14H19NO2•HClC25H30N3O8•Cl
CAS number: 19262-68-1
Warning
- Abuse and Dependence
-
High potential for abuse and dependence. Assess risk of abuse prior to initiating therapy and monitor for signs of abuse and dependence during therapy. (See Potential for Abuse and Dependence under Cautions.)
Introduction
CNS stimulant. Dexmethylphenidate is the more pharmacologically active (d-threo) enantiomer of racemic methylphenidate; pharmacologic actions qualitatively similar to those of amphetamines. Serdexmethylphenidate is a prodrug and lacks pharmacologic activity until converted to dexmethylphenidate in the GI tract.
Uses for Dexmethylphenidate
Attention Deficit Hyperactivity Disorder (ADHD)
Treatment of ADHD in children ≥6 years of age, adolescents, and adults. Multimodal, multidisciplinary treatment approaches that may include pharmacotherapy, behavioral treatment, and psychological, educational, social, and other measures are recommended in the treatment of ADHD.
Patients with ADHD may exhibit pronounced difficulties and impairment across their lifespan. Choice of therapeutic intervention(s) depends on patient's age, comorbid conditions, specific target symptoms, and strengths and weaknesses of the patient, family, school, and community.
Wide variety of treatments have been employed, including stimulants (e.g., amphetamines, methylphenidate, dexmethylphenidate), psychotropic drugs (e.g., antidepressants), and other drugs (e.g., atomoxetine, clonidine, guanfacine, viloxazine); psychosocial treatment; and other measures.
Stimulants remain the most effective and most commonly used first-line drugs for management of ADHD in pediatric patients and adults. Methylphenidate and amphetamines provide moderate to large improvements in ADHD symptoms in children and adolescents and moderate improvements in adults. Response to methylphenidate versus amphetamines is idiosyncratic.
AAP states methylphenidate may be considered for treatment of ADHD in preschool-aged children† (4 years of age to sixth birthday) if first-line treatments (i.e., parent training in behavior management and/or behavioral classroom interventions) do not provide substantial improvement and there is continued, moderate to severe disturbance in the child's functioning. Methylphenidate may be slightly less effective and less well tolerated in preschool-aged children than in school-aged children. (See Pediatric Use under Cautions.) AAP states that nonstimulants and stimulants other than methylphenidate have not been adequately studied in this age group.
For elementary and middle school-aged children (6 years of age to 12th birthday), AAP recommends that drugs with FDA-approved labeling for treatment of ADHD be used in conjunction with parent training in behavior management and/or behavioral classroom intervention (preferably both). Educational interventions and individualized instructional supports are necessary treatment components. AAP states that evidence supporting use of stimulants in elementary school-aged children is particularly strong and evidence is sufficient, but not as strong, for atomoxetine, extended-release guanfacine, and extended-release clonidine, in that order.
For adolescents (12 years of age to 18th birthday), AAP recommends that drugs with FDA-approved labeling for treatment of ADHD be used with the adolescent's assent. Concurrent use of evidence-based training interventions and/or behavioral interventions is encouraged. Educational interventions and individualized instructional supports are necessary treatment components. If concerned about drug diversion or misuse, may consider nonstimulant drugs. Use of longer-acting preparations or addition of a late-afternoon dose of a short-acting preparation may provide symptom control while adolescent is driving.
Some clinicians recommend long-acting stimulants as first-line pharmacologic therapy for adult ADHD, with long-acting nonstimulants (e.g., atomoxetine) and short- or intermediate-acting stimulants used as second-line or adjunctive therapy. Nonpharmacologic therapies (e.g., cognitive behavioral therapy, psychoeducation) also are essential. Because of high frequency of comorbid disorders, consider potential effects on comorbid psychiatric symptoms.
Nonstimulant drugs may be used alone or in combination with stimulants in patients with ADHD and comorbid conditions (e.g., aggression, anxiety, depression, tic disorders).
Although current evidence indicates that stimulants do not worsen comorbid tic disorders in most patients, some patients receiving stimulants may experience worsening of tics, and central α2-adrenergic agonists (e.g., clonidine, guanfacine) or atomoxetine may be alternative treatment options.
In patients with comorbid bipolar disorder, initiating mood stabilizing therapy prior to stimulant therapy may reduce risk of stimulants precipitating manic episodes.
When substance abuse is a concern, avoid immediate-release stimulants; may consider drugs with lower abuse potential (e.g., central α2-adrenergic agonists, atomoxetine, bupropion). Alternatively, since some evidence indicates reduced substance use during periods of ADHD stimulant therapy, may consider stimulant formulations that are less readily abused (e.g., extended-release formulations, the prodrug lisdexamphetamine) if stimulants are required for potentially greater and more rapid onset of effect.
Dexmethylphenidate Dosage and Administration
General
Pretreatment Screening
-
Evaluate pediatric patients and adults for cardiac disease (i.e., obtain careful medical history, perform physical examination, and screen for family history of sudden death or ventricular arrhythmias).
-
Evaluate risk of abuse.
Patient Monitoring
-
Monitor for signs of abuse and dependence during therapy.
Administration
Oral Administration
Dexmethylphenidate Conventional Tablets
Administer orally twice daily without regard to meals; administer doses at least 4 hours apart.
Dexmethylphenidate Extended-release Capsules
Administer orally once daily in the morning with or without food.
Swallow capsules intact. Do not crush, chew, or subdivide the capsule contents.
Alternatively, open capsule(s) and sprinkle entire contents on a small amount (e.g., 1 spoonful) of applesauce immediately prior to administration. Do not store the sprinkle/applesauce mixture for later use.
Serdexmethylphenidate/Dexmethylphenidate Capsules
Administer orally once daily in the morning with or without food.
Swallow capsules intact.
Alternatively, open capsule and sprinkle entire contents into 50 mL of water or over 2 tablespoons of applesauce immediately or within 10 minutes prior to administration. Do not store the mixture for later use.
Dosage
Available as dexmethylphenidate hydrochloride and as a fixed combination containing serdexmethylphenidate chloride and dexmethylphenidate hydrochloride (serdexmethylphenidate/dexmethylphenidate). Dosage of dexmethylphenidate hydrochloride generally is expressed in terms of the salt; however, dosage of the fixed combination is expressed in terms of serdexmethylphenidate and dexmethylphenidate. Each 26.1, 39.2, or 52.3 mg of serdexmethylphenidate is equivalent to 28, 42, or 56 mg, respectively, of serdexmethylphenidate chloride; each 5.2, 7.8, or 10.4 mg of dexmethylphenidate is equivalent to 6, 9, or 12 mg, respectively, of dexmethylphenidate hydrochloride.
Capsules containing serdexmethylphenidate chloride and dexmethylphenidate hydrochloride contain a fixed molar ratio of 70% serdexmethylphenidate and 30% dexmethylphenidate. The combined molar dose of serdexmethylphenidate and dexmethylphenidate in each dosage strength of the fixed combination (i.e., 26.1 mg/5.2 mg, 39.2 mg/7.8 mg, or 52.3 mg/10.4 mg of serdexmethylphenidate/dexmethylphenidate, respectively) is equivalent to 20, 30, or 40 mg, respectively, of dexmethylphenidate hydrochloride.
Carefully adjust dosage according to individual requirements and response.
Discontinue therapy if a beneficial effect is not attained after appropriate dosage adjustment over 1 month.
If paradoxical aggravation of symptoms occurs, reduce dosage or discontinue the drug.
Pediatric Patients
ADHD
For patients whose symptoms are not severe outside school, may attempt planned breaks in drug treatment (i.e., drug holidays) to assess continuing efficacy and need for therapy, as well as to minimize adverse effects.
Dexmethylphenidate Conventional Tablets
OralPediatric patients ≥6 years of age: Initially, 2.5 mg twice daily for children who currently are not receiving racemic methylphenidate or are receiving stimulants other than methylphenidate. Increase dosage by 2.5–5 mg daily at weekly intervals (up to maximum dosage of 20 mg daily).
Pediatric patients ≥6 years of age: Initially administer one-half the current methylphenidate hydrochloride dosage in children who are being transferred from racemic methylphenidate to dexmethylphenidate therapy.
Dexmethylphenidate Extended-release Capsules
OralPediatric patients ≥6 years of age: Initially, 5 mg once daily for children who currently are not receiving dexmethylphenidate or racemic methylphenidate or who are receiving stimulants other than methylphenidate. Increase dosage by 5 mg daily at weekly intervals (up to maximum dosage of 30 mg daily). Within the dosage range of 10–30 mg daily, no clear evidence that higher dosages provide greater average benefits than lower dosages; adverse effects and drug discontinuance are dose related.
Pediatric patients ≥6 years of age: Substitute extended-release capsules for conventional tablets at same total daily dosage.
Pediatric patients ≥6 years of age: Initially administer one-half the current methylphenidate hydrochloride dosage in children who are being transferred from racemic methylphenidate to dexmethylphenidate therapy.
Serdexmethylphenidate/Dexmethylphenidate Capsules
OralChildren 6–12 years of age: Initially, 39.2 mg of serdexmethylphenidate and 7.8 mg of dexmethylphenidate once daily. After one week, may increase dosage to 52.3 mg of serdexmethylphenidate and 10.4 mg of dexmethylphenidate once daily or decrease dosage to 26.1 mg of serdexmethylphenidate and 5.2 mg of dexmethylphenidate once daily based on response and tolerability.
Adolescents 13–17 years of age: Initially, 39.2 mg of serdexmethylphenidate and 7.8 mg of dexmethylphenidate once daily. After one week, increase dosage to 52.3 mg of serdexmethylphenidate and 10.4 mg of dexmethylphenidate once daily.
Also use these dosage titration schedules for patients being transferred from other methylphenidate-containing preparations to serdexmethylphenidate/dexmethylphenidate capsules.
Do not substitute serdexmethylphenidate/dexmethylphenidate capsules for other methylphenidate-containing preparations on mg-per-mg basis because of differences in pharmacokinetic profiles and methylphenidate base composition.
Adults
ADHD
Dexmethylphenidate Extended-release Capsules
OralInitially, 10 mg once daily for patients who currently are not receiving dexmethylphenidate or racemic methylphenidate or who are receiving stimulants other than methylphenidate. Increase dosage by 10 mg daily after 1 week (up to maximum dosage of 40 mg daily). Within the dosage range of 20–40 mg daily, no clear evidence that higher dosages provide greater average benefits than lower dosages; adverse effects and drug discontinuance are dose related.
Substitute extended-release capsules for conventional tablets at same total daily dosage.
Initially administer one-half the current methylphenidate hydrochloride dosage in patients who are being transferred from racemic methylphenidate to dexmethylphenidate therapy.
Serdexmethylphenidate/Dexmethylphenidate Capsules
OralInitially, 39.2 mg of serdexmethylphenidate and 7.8 mg of dexmethylphenidate once daily. After one week, increase dosage to 52.3 mg of serdexmethylphenidate and 10.4 mg of dexmethylphenidate once daily.
Also use this dosage titration schedule for patients being transferred from other methylphenidate-containing preparations to serdexmethylphenidate/dexmethylphenidate capsules.
Do not substitute serdexmethylphenidate/dexmethylphenidate capsules for other methylphenidate-containing preparations on mg-per-mg basis because of differences in pharmacokinetic profiles and methylphenidate base composition.
Prescribing Limits
Pediatric Patients
ADHD
Oral
Dexmethylphenidate: Maximum 20 mg daily (conventional tablets) or 30 mg daily (extended-release capsules).
Serdexmethylphenidate/dexmethylphenidate: Maximum 52.3 mg of serdexmethylphenidate and 10.4 mg of dexmethylphenidate once daily.
Long-term use not studied systematically. If used for long-term therapy, periodically reevaluate the usefulness of the drug and adjust dosage as needed.
Adults
ADHD
Oral
Dexmethylphenidate: Maximum 40 mg daily (extended-release capsules).
Serdexmethylphenidate/dexmethylphenidate: Maximum 52.3 mg of serdexmethylphenidate and 10.4 mg of dexmethylphenidate once daily.
Long-term use not studied systematically. If used for long-term therapy, periodically reevaluate the usefulness of the drug and adjust dosage as needed.
Special Populations
Hepatic Impairment
No specific dosage recommendations. (See Hepatic Impairment under Cautions.)
Renal Impairment
No specific dosage recommendations. (See Renal Impairment under Cautions.)
Cautions for Dexmethylphenidate
Contraindications
-
Concomitant or recent (within 14 days) administration of MAO inhibitors. (See Specific Drugs under Interactions.)
-
Known hypersensitivity to dexmethylphenidate, methylphenidate, serdexmethylphenidate, or any ingredient in the formulation.
Warnings/Precautions
Warnings
Potential for Abuse and Dependence
High potential for abuse and dependence.
Some evidence indicates that stimulant use does not lead to increased risk of substance abuse and that effective stimulant therapy for ADHD actually may reduce the risk for subsequent substance use disorders. However, diversion of stimulants for nonmedical uses has increased in recent decades and is a particular concern among adolescents and young adults seeking enhanced academic or work performance. Ensure that individuals are diagnosed and treated for ADHD when appropriate while limiting the risk of diversion and misuse.
Assess risk of abuse prior to initiating therapy and monitor for signs of abuse and dependence during therapy.
Maintain careful prescription records, educate patients and their families about CNS stimulant abuse and about proper storage and disposal of the drugs, monitor for signs of abuse and overdosage, and periodically reevaluate the need for continued stimulant therapy.
CNS stimulant abuse by unintended routes (e.g., chewing, snorting, injecting) may result in overdosage and death. Manifestations of CNS stimulant abuse include increased heart rate, respiratory rate, BP, and/or sweating; hyperactivity, restlessness, insomnia, loss of coordination, and tremors; flushed skin; dilated pupils; decreased appetite; and vomiting and abdominal pain. Anxiety, psychosis, hostility, aggression, and suicidal or homicidal ideation also observed.
Abrupt cessation of therapy, rapid dosage reduction, or administration of an antagonist in patients physically dependent on CNS stimulants may result in withdrawal syndrome (e.g., dysphoric mood, fatigue, vivid and unpleasant dreams, insomnia or hypersomnia, increased appetite, psychomotor retardation or agitation).
Other Warnings and Precautions
Dexmethylphenidate shares the toxic potentials of racemic methylphenidate; observe the usual precautions of racemic methylphenidate therapy.
Sudden Death and Serious Cardiovascular Events
Sudden unexplained death, stroke, and MI reported in adults with ADHD receiving usual dosages of stimulants; sudden death also reported in pediatric patients with structural cardiac abnormalities or other serious cardiac conditions receiving usual dosages of the drugs.
Although an initial epidemiologic study showed an association between use of stimulants and sudden unexplained death in healthy children and adolescents, several subsequent large epidemiologic studies in children and young adults or in adults 25–64 years of age found no association between ADHD drug use (stimulants, atomoxetine, pemoline [no longer commercially available in US]) and serious cardiovascular events (MI, stroke, sudden cardiac death), although small increases in cardiovascular risk could not be excluded.
No clinically important changes in corrected QT (QTc) interval observed in healthy individuals following 40-mg dose of extended-release dexmethylphenidate hydrochloride or following intranasal administration of serdexmethylphenidate (at 40 times the peak concentration achieved with the highest recommended serdexmethylphenidate/dexmethylphenidate dosage).
Thoroughly review medical history (including evaluation for family history of sudden death or ventricular arrhythmia) and perform physical examination in all children, adolescents, and adults being considered for stimulant therapy; if initial findings suggest presence of cardiac disease, perform further cardiac evaluation (e.g., ECG, echocardiogram).
In general, avoid use of CNS stimulants in patients with known serious structural cardiac abnormalities, cardiomyopathy, serious heart rhythm abnormalities, CAD, or other serious cardiac conditions.
Patients who develop exertional chest pain, unexplained syncope, arrhythmias, or other manifestations suggestive of cardiac disease during stimulant therapy should undergo prompt cardiac evaluation.
Effects on BP and Heart Rate
Possible modest increases in average BP (i.e., by about 2–4 mm Hg) and heart rate (i.e., by about 3–6 bpm); larger increases may occur. Modest increases not expected to have short-term sequelae; however, monitor all patients for hypertension and tachycardia.
Caution advised in patients with underlying medical conditions that might be affected by increases in BP or heart rate (e.g., hypertension, heart failure, recent MI, ventricular arrhythmia).
Psychiatric Effects
May exacerbate symptoms of behavior disturbance and thought disorder in patients with preexisting psychotic disorder.
May precipitate mixed or manic episodes in ADHD patients with comorbid bipolar disorder. Prior to initiating therapy, carefully screen patients with ADHD to determine if they are at risk for developing a manic episode; screening should include a detailed psychiatric history (e.g., current or prior depressive symptoms; family history of suicide, bipolar disorder, or depression).
Psychotic or manic symptoms (e.g., hallucinations, delusional thinking, mania) also reported with usual stimulant dosages in patients without a history of psychotic illness or mania. Pooled analysis of short-term, placebo-controlled studies identified such symptoms in about 0.1% of patients receiving stimulants and 0% of those receiving placebo. If psychotic symptoms occur, consider discontinuance of therapy.
Priapism
Prolonged and painful erections, in some cases requiring surgical intervention, reported in adult and pediatric patients receiving methylphenidate. Priapism often reported following increase in dosage; also has occurred during temporary interruptions in therapy (e.g., drug holidays) or following drug discontinuance. Risk of permanent penile damage if not treated immediately. (See Advice to Patients.)
FDA states clinicians should be cautious if they consider switching patients from methylphenidate because of this risk; certain alternative ADHD treatments (e.g., atomoxetine) also may cause priapism.
Peripheral Vascular Effects
Peripheral vascular disorders, including Raynaud's phenomenon, reported in patients in all age groups receiving stimulants at therapeutic dosages and at various times throughout treatment course. Manifestations usually intermittent and mild, but ulceration of digits and/or breakdown of soft tissue occur rarely. Carefully observe for digital changes.
Improvement generally observed following dosage reduction or drug discontinuance; however, some patients may require further evaluation (e.g., referral to a rheumatologist).
Growth Suppression
Long-term administration of stimulants in children with ADHD associated with at least a temporary suppression of normal weight and/or height patterns in some patients.
In the Multimodal Treatment Study of Children with ADHD (MTA), slowing in growth rate (on average, height gain suppressed by about 2 cm and weight gain suppressed by 2.7 kg over 3 years) observed with methylphenidate treatment for up to 3 years in children 7–13 years of age, without evidence of growth rebound during this period of development. Longer-term follow-up into early adulthood suggested that consistent extended use of stimulants from childhood through adolescence may be associated with suppression of adult height.
Manufacturer recommends monitoring growth during treatment; patients not growing or gaining weight as expected may require temporary discontinuance of treatment.
Hypersensitivity Reactions
Hypersensitivity reactions, including angioedema and anaphylaxis, reported.
Specific Populations
Pregnancy
National Pregnancy Registry for ADHD Medications (866-961-2388 or [Web]).
Available data on methylphenidate use during pregnancy have not identified a drug-associated risk of major birth defects, spontaneous abortion, or adverse maternal or fetal outcomes; however, CNS stimulant use during pregnancy may have fetal risks. CNS stimulants can cause vasoconstriction and thereby decrease placental perfusion. Although no fetal or neonatal adverse reactions reported with therapeutic methylphenidate dosages during pregnancy, premature delivery and low birthweight reported in women dependent on amphetamines.
Decreased pup weight (in males) and delayed fetal skeletal ossification observed in animal studies with dexmethylphenidate.
Lactation
Limited data (case reports) suggest that exclusively breast-fed infants receive about 0.16–0.7% of the maternal weight-adjusted dosage of racemic methylphenidate; milk-to-plasma ratio of 1.1–2.7 reported.
No reports of adverse effects of methylphenidate on breast-fed infants and no reported effects on milk production. Long-term neurodevelopmental effects resulting from infant exposure to CNS stimulants unknown.
Consider developmental and health benefits of breast-feeding along with the mother’s clinical need for dexmethylphenidate and any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition. Monitor infants exposed to dexmethylphenidate through breast milk for adverse effects (e.g., agitation, insomnia, anorexia, reduced weight gain).
Pediatric Use
Safety and efficacy not established in children <6 years of age.
Long-term efficacy of dexmethylphenidate in pediatric patients not established.
Sudden death reported in children and adolescents with structural cardiac abnormalities or other serious cardiac conditions receiving usual dosages of stimulants. (See Sudden Death and Serious Cardiovascular Events under Cautions.)
Long-term administration expected to cause at least a temporary suppression of normal weight and/or height patterns in some children and adolescents. (See Growth Suppression under Cautions.)
Long-term behavioral effects (decreased spontaneous locomotor activity in adulthood, deficit in acquisition of a specific learning task in females) observed in juvenile animal toxicity studies in rats receiving racemic methylphenidate from the early postnatal period through sexual maturation. Clinical relevance is unknown.
Geriatric Use
Safety and efficacy not established.
Hepatic Impairment
Safety and efficacy not established.
Renal Impairment
Safety and efficacy not established. Renal impairment expected to have minimal effect on pharmacokinetics of the drug.
Common Adverse Effects
Dexmethylphenidate conventional tablets: Abdominal pain, fever, anorexia, nausea.
Dexmethylphenidate extended-release capsules: Decreased appetite/anorexia, headache, dyspepsia, dry mouth, anxiety, insomnia, vomiting, pharyngolaryngeal pain.
Interactions for Dexmethylphenidate
Methylphenidate is not metabolized by CYP isoenzymes to a clinically important extent; the d- and l-enantiomers of methylphenidate do not substantially inhibit CYP isoenzymes 1A2, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A.
Serdexmethylphenidate does not appear to be a substrate or inhibitor of P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), organic anion transport protein (OATP) 1B1 or 1B3, organic anion transporter (OAT) 1 or 3, organic cation transporter (OCT) 2, or multidrug and toxin extrusion protein (MATE) 1 or 2K in vitro.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interaction is unlikely. CYP inducers or inhibitors not expected to have a clinically important effect on the pharmacokinetics of methylphenidate, and methylphenidate did not increase plasma concentrations of desipramine (CYP2D6 substrate).
Interactions Involving Methylphenidate
The possibility that drug interactions reported with racemic methylphenidate also could occur with dexmethylphenidate should be considered.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
No clinically important effect on rate or extent of release of either component of serdexmethylphenidate/dexmethylphenidate capsules in vitro |
|
|
Anesthetics, halogenated (e.g., desflurane, enflurane, halothane, isoflurane, sevoflurane) |
Possible sudden increase in BP and heart rate during surgery |
Avoid dexmethylphenidate use on day of surgery |
|
Antihypertensive agents (e.g., ACE inhibitors, angiotensin II receptor antagonists, β-adrenergic blocking agents, central α2-adrenergic agonists, calcium-channel blocking agents, potassium-sparing and thiazide diuretics) |
Antagonism of hypotensive effect |
Monitor BP and increase antihypertensive agent dosage as necessary |
|
MAO inhibitors (e.g., isocarboxazid, linezolid, methylene blue, phenelzine, selegiline, tranylcypromine) |
Hypertensive crisis, possibly resulting in death, stroke, MI, aortic dissection, ophthalmologic complications, eclampsia, pulmonary edema, and renal failure |
Dexmethylphenidate contraindicated in patients who are receiving or have received MAO inhibitors within 14 days |
|
Risperidone |
Possible increased risk of extrapyramidal symptoms following a change (either increase or decrease) in dosage of either or both drugs |
Monitor for extrapyramidal symptoms |
Dexmethylphenidate Pharmacokinetics
Absorption
Bioavailability
Dexmethylphenidate: Readily absorbed following oral administration. Mean absolute bioavailability is 22–25% due to high first-pass metabolism.
Serdexmethylphenidate: Prodrug; inactive until converted to dexmethylphenidate in GI tract (thought to occur mainly in lower GI tract). Oral bioavailability of serdexmethylphenidate is <3%.
Dexmethylphenidate conventional tablets: Peak plasma concentrations are achieved within 60–90 minutes following oral administration in fasting patients.
Dexmethylphenidate extended-release capsules: Peak plasma concentrations are attained at 1.5 hours and again at 6.5 hours after a dose.
Extended-release capsules are absorbed more slowly but to the same extent as conventional tablets. AUC is similar for extended-release capsules (administered once daily) and conventional tablets (same daily dosage administered in 2 divided doses 4 hours apart).
Comparable plasma concentrations achieved following single-dose administration of dexmethylphenidate hydrochloride capsules or single-dose administration of racemic methylphenidate hydrochloride capsules at equimolar doses (twice the total mg amount of dexmethylphenidate hydrochloride).
Serdexmethylphenidate/dexmethylphenidate capsules: Inclusion of immediate-release dexmethylphenidate in the fixed-combination preparation allows for rapid attainment of therapeutic concentrations of the active drug. Peak plasma dexmethylphenidate concentrations attained approximately 2 hours after oral administration of the fixed combination, but approximately 8 hours after oral administration of serdexmethylphenidate alone.
Food
Dexmethylphenidate conventional tablets: High-fat meal slows rate of absorption but does not alter peak concentration or extent of absorption compared with administration in fasting state. Food prolonged time to peak concentration from 1.5 hours (fasted state) to 2.9 hours (fed state).
Dexmethylphenidate extended-release capsules: Administration with food may slow onset of action.
Serdexmethylphenidate/dexmethylphenidate capsules: Food may delay absorption but does not alter extent of absorption. No clinically important differences in dexmethylphenidate exposure observed whether administered with high-fat, high-calorie meal; sprinkled in applesauce or water; or in fasting state. Food prolonged median time to peak plasma concentration from 2 hours (fasted state) to 4–4.5 hours (fed state).
Special Populations
Sex, dexmethylphenidate conventional tablets: AUC is higher in women than in men; pharmacokinetics parameters are similar between boys and girls (mean age 10 years).
Sex, dexmethylphenidate extended-release capsules: Peak plasma concentration during first absorption phase is higher in women than in men.
Age, dexmethylphenidate conventional tablets: Following single dose, peak concentrations are similar but AUC is lower in children 6–12 years of age than in adults. Pharmacokinetics not studied in children <6 years of age.
Age, dexmethylphenidate extended-release capsules: Pharmacokinetics not studied in pediatric patients <18 years of age; however, following administration of a similar formulation of racemic methylphenidate, between-peak minimum and second peak concentrations were delayed and more variable in children than in adults.
Age, serdexmethylphenidate/dexmethylphenidate capsules: Dexmethylphenidate exposure in children 6–12 years of age is approximately twice that in adults and adolescents 13–17 years of age.
Distribution
Extent
Not known whether dexmethylphenidate crosses placenta or distributes into milk.
Elimination
Metabolism
Metabolized principally by de-esterification to form d-ritalinic acid, which has little or no pharmacologic activity.
Elimination Route
Excreted in urine, principally as ritalinic acid.
Half-life
Dexmethylphenidate: 2–3 hours in children or 3 hours in adults.
Serdexmethylphenidate/dexmethylphenidate capsules: Mean terminal elimination half-lives of 5.7 hours (serdexmethylphenidate) and 11.7 hours (dexmethylphenidate) in adults.
Stability
Storage
Oral
Dexmethylphenidate Conventional Tablets
25°C (may be exposed to 15–30°C). Protect from light and moisture.
Dexmethylphenidate Extended-release Capsules
Tight container at 25°C (may be exposed to 15–30°C).
Serdexmethylphenidate/Dexmethylphenidate Capsules
Tight container at 20–25°C (may be exposed to 15–30°C). Protect from moisture.
Actions
-
Appears to block norepinephrine and dopamine reuptake into the presynaptic neuron and increases their release into the extraneuronal space. Mechanism of action for treatment of ADHD not determined.
-
Serdexmethylphenidate is a prodrug and has no pharmacologic activity until converted to dexmethylphenidate in the GI tract.
Advice to Patients
-
Provide patient or caregiver with a copy of manufacturer’s patient information (medication guide).
-
Risk of abuse and dependence. Importance of not sharing dexmethylphenidate with others and of storing the drug in a safe (preferably locked) location to prevent abuse. Advise patient or caregiver on proper disposal of any remaining unused or expired drug.
-
Potential risk for serious cardiovascular events, including sudden death, MI, stroke, and hypertension. Importance of informing clinicians immediately of any adverse cardiovascular effects (e.g., exertional chest pain, unexplained syncope, other symptoms suggestive of cardiac disease).
-
Advise patient or caregiver that dexmethylphenidate can elevate BP and pulse rate.
-
Potential for recommended dosages of dexmethylphenidate to cause psychotic or manic symptoms, even in patients without a history of psychotic symptoms or mania.
-
Inform male patients and their caregivers about the signs and symptoms of priapism, stressing the need for immediate treatment if it occurs. Younger males, especially prepubertal males, may not recognize the problem or may be embarrassed to tell anyone if it occurs.
-
Inform patient or caregiver about the risk of peripheral vascular disorders, including Raynaud's phenomenon, and the associated signs and symptoms (e.g., feelings of numbness, coolness, or pain in fingers or toes; changes in color from pale to blue to red). Advise patients to report any new numbness, pain, skin color change, or sensitivity to temperature in fingers or toes and to immediately contact their clinician if any signs of unexplained wounds appear on fingers or toes; further clinical evaluation may be appropriate.
-
Potential for dexmethylphenidate to slow growth and cause weight loss.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Inform women about pregnancy registry for ADHD medications. (See Pregnancy under Cautions.) Advise nursing women to monitor their infants for agitation, poor feeding, and reduced weight gain.
-
Importance of not chewing or crushing the beads contained in dexmethylphenidate extended-release capsules and of not storing the sprinkle/food mixture for later use. If the contents of serdexmethylphenidate/dexmethylphenidate capsules are sprinkled in water or over applesauce, importance of administering the mixture immediately or within 10 minutes of mixing and of not storing the mixture for later use.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal products, as well as any concomitant illnesses/conditions (e.g., cardiac/cardiovascular disease, mental/psychiatric disorder, suicidal ideation or behaviors, history of substance abuse).
-
Importance of informing patients or caregivers of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as a schedule II (C-II) drug.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, extended-release (containing beads) |
5 mg (beads, delayed-release, enteric-coated extended-release 2.5 mg with immediate-release 2.5 mg)* |
Dexmethylphenidate Hydrochloride Extended-release Capsules ( C-II) |
|
|
Focalin XR ( C-II) |
Novartis |
|||
|
10 mg (beads, delayed-release, enteric-coated extended-release 5 mg with immediate-release 5 mg)* |
Dexmethylphenidate Hydrochloride Extended-release Capsules ( C-II) |
|||
|
Focalin XR ( C-II) |
Novartis |
|||
|
15 mg (beads, delayed-release, enteric-coated extended-release 7.5 mg with immediate-release 7.5 mg)* |
Dexmethylphenidate Hydrochloride Extended-release Capsules ( C-II) |
|||
|
Focalin XR ( C-II) |
Novartis |
|||
|
20 mg (beads, delayed-release, enteric-coated extended-release 10 mg with immediate-release 10 mg)* |
Dexmethylphenidate Hydrochloride Extended-release Capsules ( C-II) |
|||
|
Focalin XR ( C-II) |
Novartis |
|||
|
25 mg (beads, delayed-release, enteric-coated extended-release 12.5 mg with immediate-release 12.5 mg) |
Focalin XR ( C-II) |
Novartis |
||
|
30 mg (beads, delayed-release, enteric-coated extended-release 15 mg with immediate-release 15 mg)* |
Dexmethylphenidate Hydrochloride Extended-release Capsules ( C-II) |
|||
|
Focalin XR ( C-II) |
Novartis |
|||
|
35 mg (beads, delayed-release, enteric-coated extended-release 17.5 mg with immediate-release 17.5 mg) |
Focalin XR ( C-II) |
Novartis |
||
|
40 mg (beads, delayed-release, enteric-coated extended-release 20 mg with immediate-release 20 mg)* |
Dexmethylphenidate Hydrochloride Extended-release Capsules ( C-II) |
|||
|
Focalin XR ( C-II) |
Novartis |
|||
|
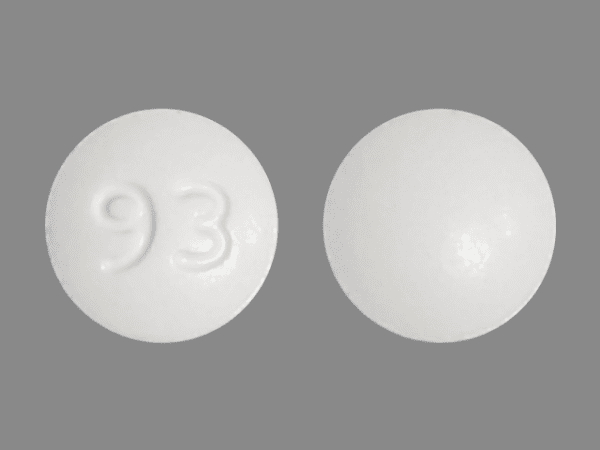
Tablets |
2.5 mg* |
Dexmethylphenidate Hydrochloride Capsules ( C-II) |
||
|
Focalin ( C-II) |
Novartis |
|||
|
5 mg* |
Dexmethylphenidate Hydrochloride Capsules ( C-II) |
|||
|
Focalin ( C-II) |
Novartis |
|||
|
10 mg* |
Dexmethylphenidate Hydrochloride Capsules ( C-II) |
|||
|
Focalin ( C-II) |
Novartis |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
Serdexmethylphenidate Chloride 26.1 mg (of serdexmethylphenidate) and Dexmethylphenidate Hydrochloride 5.2 mg (of dexmethylphenidate) (equivalent to 28 mg serdexmethylphenidate chloride and 6 mg dexmethylphenidate hydrochloride) |
Azstarys (C-II) |
Corium |
|
Serdexmethylphenidate Chloride 39.2 mg (of serdexmethylphenidate) and Dexmethylphenidate Hydrochloride 7.8 mg (of dexmethylphenidate) (equivalent to 42 mg serdexmethylphenidate chloride and 9 mg dexmethylphenidate hydrochloride) |
Azstarys (C-II) |
Corium |
||
|
Serdexmethylphenidate Chloride 52.3 mg (of serdexmethylphenidate) and Dexmethylphenidate Hydrochloride 10.4 mg (of dexmethylphenidate) (equivalent to 56 mg serdexmethylphenidate chloride and 12 mg dexmethylphenidate hydrochloride) |
Azstarys (C-II) |
Corium |
AHFS DI Essentials™. © Copyright 2022, Selected Revisions December 13, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about dexmethylphenidate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (300)
- Drug images
- Latest FDA alerts (2)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: CNS stimulants
- Breastfeeding
- En español
Patient resources
- Dexmethylphenidate drug information
- Dexmethylphenidate Tablets
- Dexmethylphenidate Extended-Release Capsules
Professional resources
- Dexmethylphenidate Hydrochloride and Serdexmethylphenidate Chloride monograph
- Dexmethylphenidate (FDA)
- Dexmethylphenidate ER Capsule (FDA)