Alogliptin (Monograph)
Brand name: Nesina
Drug class: Dipeptidyl Peptidase-4 (DPP-4) Inhibitors
VA class: HS502
Chemical name: 2-[[6-[(3R)-3-Amino-1-piperidinyl]-3,4-dihydro-3-methyl-2,4-dioxo-1(2H)-pyrimidinyl]methyl]-benzonitrile monobenzoate
Molecular formula: C18H21N5O2•C7H6O2
CAS number: 850649-62-6
Introduction
Antidiabetic agent; dipeptidyl peptidase-4 (DPP-4) inhibitor.
Uses for Alogliptin
Type 2 Diabetes Mellitus
Used as monotherapy as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus.
Used in combination with pioglitazone (given separately or as the fixed combination) as initial therapy as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus when treatment with both alogliptin and pioglitazone is appropriate.
Used in combination with metformin (given separately or as the fixed combination) as initial therapy as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus when treatment with both alogliptin and metformin is appropriate.
Used in combination with other oral antidiabetic agents (e.g., metformin, a sulfonylurea, a thiazolidinedione [peroxisome proliferator-activated receptor-γ agonist]) or insulin as an adjunct to diet and exercise in patients with type 2 diabetes mellitus who have not achieved adequate glycemic control.
Current guidelines for the treatment of type 2 diabetes mellitus generally recommend metformin as first-line therapy in addition to lifestyle modifications in patients with recent-onset type 2 diabetes mellitus or mild hyperglycemia due to its well-established safety and efficacy (e.g., beneficial effects on glycosylated hemoglobin [hemoglobin A1c; HbA1c], weight, and cardiovascular mortality).
In patients with metformin contraindications or intolerance (e.g., risk of lactic acidosis, GI intolerance) or in selected other patients, some experts suggest that initial therapy with a drug from another class of antidiabetic agents (e.g., a glucagon-like peptide-1 [GLP-1] receptor agonist, sodium-glucose cotransporter 2 [SGLT2] inhibitor, DPP-4 inhibitor, sulfonylurea, thiazolidinedione, basal insulin) may be acceptable based on patient factors.
May need to initiate therapy with 2 agents (e.g., metformin plus another drug) in patients with high initial HbA1c (>7.5% or ≥1.5% above target). In such patients with metformin intolerance, some experts suggest initiation of therapy with 2 drugs from other drug classes with complementary mechanisms of action.
Consider early initiation of combination therapy for the treatment of type 2 diabetes mellitus to extend the time to treatment failure and more rapidly attain glycemic goals.
For patients with inadequate glycemic control on metformin monotherapy, consider patient comorbidities (e.g., atherosclerotic cardiovascular disease [ASCVD], established kidney disease, heart failure), hypoglycemia risk, impact on weight, cost, risk of adverse effects, and patient preferences when selecting additional antidiabetic agents for combination therapy. DPP-4 inhibitors recommended by some experts as one of several classes of drugs for use in combination therapy, particularly in patients with both postprandial and fasting plasma glucose elevations.
Consider early introduction of insulin for severe hyperglycemia (e.g., blood glucose of ≥300 mg/dL or HbA1c >9–10%), especially if accompanied by catabolic manifestations (e.g., weight loss, hypertriglyceridemia, ketosis) or symptoms of hyperglycemia.
Not indicated for treatment of type 1 diabetes mellitus or diabetic ketoacidosis.
Alogliptin Dosage and Administration
Administration
Oral Administration
If a dose is missed, take missed dose as soon as it is remembered followed by resumption of regular schedule. If the missed dose is not remembered until time of next dose, skip missed dose and resume regular schedule. Do not take double dose to replace missed dose.
Alogliptin Monotherapy
Administer once daily without regard to food.
Alogliptin/Metformin Hydrochloride Fixed Combination
Administer twice daily with food; titrate dosage gradually to minimize adverse GI effects of metformin hydrochloride component.
Swallow tablets whole; do not split before swallowing.
Alogliptin/Pioglitazone Fixed Combination
Administer once daily without regard to food.
Swallow tablets whole; do not split before swallowing.
Dosage
Available as alogliptin benzoate; dosage expressed in terms of alogliptin.
Adults
Type 2 Diabetes Mellitus
Monotherapy
Oral25 mg once daily.
Alogliptin/Metformin Hydrochloride Fixed Combination
OralIndividualize dosage of alogliptin/metformin hydrochloride based on patient's current antidiabetic regimen, effectiveness, and tolerability; increase dosage gradually to reduce adverse GI effects of metformin hydrochloride component.
Alogliptin/Pioglitazone Fixed Combination
OralPatients with inadequate glycemic control on diet and exercise: Alogliptin 25 mg and pioglitazone 15 or 30 mg once daily.
Patients with inadequate glycemic control on alogliptin: Alogliptin 25 mg and pioglitazone 15 or 30 mg once daily.
Patients with inadequate glycemic control on pioglitazone monotherapy: Alogliptin 25 mg and pioglitazone 15, 30, or 45 mg once daily, based on the patient’s current antidiabetic therapy.
Patients with inadequate glycemic control on metformin monotherapy: Alogliptin 25 mg and pioglitazone 15 or 30 mg once daily.
Prescribing Limits
Adults
Type 2 Diabetes Mellitus
Oral
Fixed combination with metformin hydrochloride: Maximum of 25 mg of alogliptin and 2 g of metformin hydrochloride daily.
Fixed combination with pioglitazone: Maximum of 25 mg of alogliptin and 45 mg of pioglitazone.
Special Populations
No dosage adjustment is necessary based on sex or race.
Hepatic Impairment
Alogliptin Monotherapy
Mild or moderate hepatic impairment: No dosage adjustment is recommended.
Severe hepatic impairment: Data are lacking.
Alogliptin/Metformin Hydrochloride Fixed Combination
Fixed combination of alogliptin and metformin hydrochloride not recommended in patients with hepatic impairment.
Renal Impairment
Alogliptin Monotherapy
Mild renal impairment (Clcr ≥60 mL/minute): No alogliptin dosage adjustment is necessary.
Moderate renal impairment (Clcr 30 to <60 mL/minute): 12.5 mg once daily.
Severe renal impairment (Clcr 15–30 mL/minute) or end-stage renal disease (ESRD) (Clcr <15 mL/minute or requiring hemodialysis): 6.25 mg once daily without regard to timing of hemodialysis.
Alogliptin/Metformin Hydrochloride Fixed Combination
Fixed combination of alogliptin and metformin hydrochloride is contraindicated in patients with renal impairment.
Alogliptin/Pioglitazone Fixed Combination
Mild renal impairment (Clcr ≥60 mL/minute): No dosage adjustment necessary.
Moderate renal impairment (Clcr 30 to <60 mL/minute): Alogliptin 12.5 mg and pioglitazone 15, 30, or 45 mg once daily.
Severe renal impairment or ESRD: Not recommended.
Geriatric Patients
Dosage adjustment not necessary.
Patients with CHF
NYHA class III or IV: Do not initiate fixed combination of alogliptin and pioglitazone.
NYHA class I or II: 25 mg of alogliptin and 15 mg of pioglitazone once daily in fixed combination.
Cautions for Alogliptin
Contraindications
-
Known serious hypersensitivity (e.g., anaphylaxis, angioedema, severe adverse cutaneous reactions) to alogliptin.
Warnings/Precautions
Pancreatitis and Pancreatic Precancerous Changes
Acute pancreatitis reported during postmarketing experience. FDA has been evaluating unpublished findings suggesting an increased risk of pancreatitis and precancerous pancreatic cell changes in patients with type 2 diabetes mellitus receiving incretin mimetics. FDA will notify healthcare professionals of its conclusions and recommendations when the review is complete, or when FDA has additional information to report.
FDA has recommended that clinicians continue to follow the recommendations in the prescribing information for incretin mimetics. Manufacturer states that patients should be observed carefully for signs and symptoms of pancreatitis. If pancreatitis is suspected, promptly discontinue alogliptin and institute appropriate management.
Not known if history of pancreatitis increases risk for pancreatitis with alogliptin.
Heart Failure Risk
Possible increased risk of heart failure, particularly in patients with history of heart failure or renal impairment. In a randomized, placebo-controlled, double-blind study in which alogliptin was added to standard care in 5380 patients with type 2 diabetes mellitus and recent acute coronary syndrome, 3.9% of patients receiving alogliptin experienced at least one hospitalization for heart failure compared with 3.3% of patients receiving placebo.
Consider potential risks and benefits of alogliptin therapy prior to use in patients at higher risk for heart failure. Monitor patients for manifestations of heart failure. (See Advice to Patients.) If heart failure develops, institute appropriate evaluation and management according to current standards of care and consider discontinuance of alogliptin.
Severe Arthralgia
Severe, disabling joint pain reported in patients receiving DPP-4 inhibitors (e.g., alogliptin, linagliptin, saxagliptin, sitagliptin). Onset of such symptoms has ranged from 1 day to years following initiation of therapy. Symptoms resolved upon discontinuance of the DPP-4 inhibitor; symptoms recurred in some patients when the same or another DPP-4 inhibitor was restarted. Consider DPP-4 inhibitors as a possible cause of severe joint pain and discontinue if appropriate. (See Advice to Patients.)
Sensitivity Reactions
Hypersensitivity reactions (e.g., anaphylaxis, angioedema, severe adverse cutaneous reactions, including Stevens-Johnson syndrome) reported.
Promptly discontinue alogliptin if a serious hypersensitivity reaction is suspected, investigate other potential causes, and institute alternative antidiabetic therapy. (See Advice to Patients.)
Use with caution in patients with a history of angioedema to other DDP-4 inhibitors; unknown whether such patients will be predisposed to angioedema with alogliptin.
Hepatic Effects
Fatal and nonfatal hepatic failure reported. Assess hepatic function prior to alogliptin initiation; use with caution in patients with abnormal liver function test results.
Promptly assess liver function in patients with signs or symptoms indicating liver injury (e.g., fatigue, anorexia, right upper abdominal discomfort, dark urine, jaundice). Interrupt alogliptin treatment if clinically important liver enzyme elevations and if liver function test abnormalities persist or worsen. Do not restart the drug in these patients without another explanation for the test abnormalities.
Concomitant Therapy with Hypoglycemic Agents
When used in combination with an insulin secretagogue (e.g., a sulfonylurea) or insulin, consider reducing the dosage of the insulin secretagogue or insulin to reduce the risk of hypoglycemia.
Macrovascular Outcomes
Manufacturer states that evidence of macrovascular risk reduction with alogliptin or any other antidiabetic agent not conclusively demonstrated in clinical trials.
Use of Fixed Combinations
When used in fixed combination with metformin hydrochloride or pioglitazone, consider the cautions, precautions, and contraindications associated with metformin or pioglitazone in addition to those of alogliptin.
Specific Populations
Pregnancy
Category B.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Use caution.
Pediatric Use
Safety and efficacy of alogliptin alone, in fixed combination with metformin, or in fixed combination with pioglitazone not established in pediatric patients <18 years of age.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.
Hepatic Impairment
Moderate hepatic impairment decreased alogliptin total exposure. (See Absorption: Special Populations, under Pharmacokinetics.) Data lacking in severe hepatic impairment.
Fixed combination of alogliptin and metformin hydrochloride not recommended in patients with hepatic impairment.
Renal Impairment
Renal impairment increases AUC. (See Absorption: Special Populations, under Pharmacokinetics.) Dosage adjustment recommended for patients with moderate or severe renal impairment or ESRD. (See Renal Impairment under Dosage and Administration.)
Fixed combination of alogliptin and metformin hydrochloride contraindicated in patients with renal impairment.
Assess renal function prior to initiation of therapy and periodically thereafter.
Common Adverse Effects
Alogliptin monotherapy: Nasopharyngitis, headache, upper respiratory tract infection.
Alogliptin/metformin hydrochloride fixed combination: Upper respiratory tract infection, nasopharyngitis, diarrhea, hypertension, headache, back pain, urinary tract infection.
Alogliptin/pioglitazone fixed combination: Nasopharyngitis, back pain, upper respiratory tract infection.
Drug Interactions
Mainly renally excreted; CYP-related metabolism is negligible.
Does not induce CYP1A2, 2B6, 2C9, 2C19, or 3A4 and does not inhibit CYP1A2, 2C8, 2C9, 2C19, 3A4, or 2D6.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
CYP2C8, 2C9, and 3A4 inhibitors: No clinically important interactions observed with the inhibitors tested.
CYP1A2, 2C8, 2C9, 2D6, and 3A4 substrates: No clinically important interactions observed with the substrates tested.
Substrates or Inhibitors of P-glycoprotein (P-gp) Transport Systems
No clinically important interactions observed with the substrates or inhibitors tested.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Atorvastatin |
Did not alter peak plasma concentrations or AUC of either drug |
No dosage adjustment necessary |
|
Caffeine |
Did not alter peak plasma concentrations or AUC of caffeine |
No dosage adjustment necessary |
|
Cimetidine |
Did not alter peak plasma concentrations or AUC of either drug |
No dosage adjustment necessary |
|
Contraceptives, hormonal |
Did not alter peak plasma concentrations or AUC of ethinyl estradiol or norethindrone |
No dosage adjustment necessary |
|
Cyclosporine |
Did not alter peak plasma concentrations or AUC of alogliptin |
No dosage adjustment necessary |
|
Dextromethorphan |
Did not alter peak plasma concentrations or AUC of dextromethorphan |
No dosage adjustment necessary |
|
Digoxin |
Did not alter peak plasma concentrations or AUC of either drug |
No dosage adjustment necessary |
|
Fexofenadine |
Did not alter peak plasma concentrations or AUC of fexofenadine |
No dosage adjustment necessary |
|
Fluconazole |
Did not alter peak plasma concentrations or AUC of alogliptin |
No dosage adjustment necessary |
|
Gemfibrozil |
Did not alter peak plasma concentrations or AUC of alogliptin |
No dosage adjustment necessary |
|
Glyburide |
Did not alter peak plasma concentrations or AUC of glyburide |
No dosage adjustment necessary |
|
Ketoconazole |
Did not alter peak plasma concentrations or AUC of alogliptin |
No dosage adjustment necessary |
|
Metformin |
Did not alter peak plasma concentrations or AUC of either drug |
No dosage adjustment necessary |
|
Midazolam |
Did not alter peak plasma concentrations or AUC of midazolam |
No dosage adjustment necessary |
|
Pioglitazone |
Did not alter peak plasma concentrations or AUC of either drug |
No dosage adjustment necessary |
|
Tolbutamide |
Did not alter peak plasma concentrations or AUC of tolbutamide |
No dosage adjustment necessary |
|
Warfarin |
No change in peak plasma concentrations or AUC of warfarin; no change in PT or INR |
No dosage adjustment necessary |
Alogliptin Pharmacokinetics
Absorption
Bioavailability
Approximately 100%.
Onset
Median time to peak plasma concentration was 1–2 hours following single oral dose.
Food
Food does not appear to affect absorption.
Special Populations
Total alogliptin exposure in patients with moderate hepatic impairment (Child-Pugh class B) is about 10% lower than in healthy individuals.
In patients with renal impairment, AUC increased 1.2-fold in those with Clcr 60 to <90 mL/minute, twofold in those with Clcr 30 to <60 mL/minute, threefold in those with Clcr 15 to <30 mL/minute, and fourfold in those with ESRD (Clcr <15 mL/minute or requiring dialysis).
Age does not substantially affect alogliptin pharmacokinetics.
Distribution
Extent
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
20%.
Elimination
Metabolism
Does not undergo extensive metabolism.
Elimination Route
Excreted in urine (76%) mainly as unchanged drug and in the feces (13%).
Half-life
Approximately 21 hours.
Special Populations
Hemodialysis (3-hour session) removes about 7% of the drug.
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).
Keep alogliptin/pioglitazone fixed-combination tablets in tightly closed container and protect from moisture and humidity.
Keep alogliptin/metformin hydrochloride fixed-combination tablets in tightly closed container.
Actions
-
Inhibits DPP-4, an enzyme that inactivates incretin hormones glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP).
-
Increases circulating concentrations of GLP-1 and GIP in a glucose-dependent manner.
-
GLP-1 and GIP stimulate insulin secretion from pancreatic β-cells in a glucose-dependent manner (i.e., when glucose concentrations are elevated).
-
GLP-1 also decreases glucagon secretion from pancreatic α-cells, leading to reduced hepatic glucose production.
-
Selectively inhibits DPP-4 with no effect on DPP-8 or DPP-9 in vitro at concentrations approximating those from therapeutic exposures.
Advice to Patients
-
Importance of patient reading medication guide before initiating therapy and each time the drug is dispensed.
-
Importance of informing patients of the potential risks and benefits of alogliptin. Importance of not using alogliptin in patients with type 1 diabetes mellitus or diabetic ketoacidosis.
-
Risk of acute pancreatitis; may be severe or fatal. Importance of patient informing clinicians about a history of pancreatitis, gallstones, alcoholism, or kidney or liver problems. Importance of patient discontinuing alogliptin and promptly notifying clinician if signs and symptoms of pancreatitis, including persistent severe abdominal pain that may radiate to the back and may or may not be accompanied by vomiting, occur.
-
Importance of informing patients about possibility of heart failure with alogliptin therapy. Importance of patients informing clinicians about a history of heart failure or renal impairment. Importance of informing patients about signs and symptoms of heart failure (e.g., shortness of breath, weight gain, edema); importance of patients immediately contacting a clinician if manifestations of heart failure occur.
-
Importance of informing patients of the possibility of severe and disabling joint pain. Advise patients to contact a clinician promptly if severe and persistent joint pain occurs; patients should not discontinue therapy without consulting their clinician.
-
Risk of hypoglycemia, particularly if concomitant therapy with a sulfonylurea (i.e., insulin secretagogue) or insulin is used.
-
Risk of serious allergic (hypersensitivity) reaction. If signs or symptoms of such reactions occur (e.g., rash, hives, swelling of the face, lips, tongue, and throat that may cause difficulty in breathing or swallowing), importance of discontinuing alogliptin and informing clinician promptly.
-
Possibility of liver injury, sometimes fatal. If signs or symptoms of liver injury (e.g., nausea, vomiting, abdominal pain, unusual/unexplained fatigue, anorexia, dark urine, jaundice) occur, importance of discontinuing alogliptin and informing clinician promptly.
-
Importance of taking alogliptin exactly as directed by clinician. (See Administration under Dosage and Administration.)
-
Importance of women informing their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
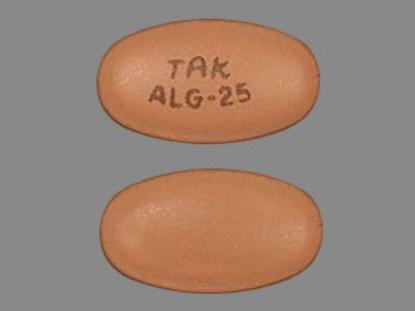
Oral |
Tablets, film-coated |
6.25 mg (of alogliptin) |
Nesina |
Takeda |
|
12.5 mg (of alogliptin) |
Nesina |
Takeda |
||
|
25 mg (of alogliptin) |
Nesina |
Takeda |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
12.5 mg (of alogliptin) with Metformin Hydrochloride 500 mg |
Kazano |
Takeda |
|
12.5 mg (of alogliptin) with Metformin Hydrochloride 1 g |
Kazano |
Takeda |
||
|
12.5 mg (of alogliptin) with Pioglitazone Hydrochloride 15 mg (of pioglitazone) |
Oseni |
Takeda |
||
|
12.5 mg (of alogliptin) with Pioglitazone Hydrochloride 30 mg (of pioglitazone) |
Oseni |
Takeda |
||
|
12.5 mg (of alogliptin) with Pioglitazone Hydrochloride 45 mg (of pioglitazone) |
Oseni |
Takeda |
||
|
25 mg (of alogliptin) with Pioglitazone Hydrochloride 15 mg (of pioglitazone) |
Oseni |
Takeda |
||
|
25 mg (of alogliptin) with Pioglitazone Hydrochloride 30 mg (of pioglitazone) |
Oseni |
Takeda |
||
|
25 mg (of alogliptin) with Pioglitazone Hydrochloride 45 mg (of pioglitazone) |
Oseni |
Takeda |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 21, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about alogliptin
- Check interactions
- Compare alternatives
- Reviews (9)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: dipeptidyl peptidase 4 inhibitors
- Breastfeeding
- En español