Liothyronine
Generic name: liothyronine [ LYE-oh-THYE-roe-neen ]
Brand names: Cytomel, Triostat
Dosage form: oral tablet (25 mcg; 5 mcg; 50 mcg)
Drug class: Thyroid drugs
What is liothyronine?
Liothyronine is a man-made form of a hormone that is normally produced by your thyroid gland to regulate the body's energy and metabolism. Liothyronine is given when the thyroid does not produce enough of this hormone on its own.
Liothyronine treats hypothyroidism (low thyroid hormone). Liothyronine is also given as part of a medical test for thyroid disorders.
Liothyronine is also used together with surgery and radioactive iodine therapy in people with thyroid cancer.
Liothyronine should not be used to treat obesity or weight problems.
Liothyronine may also be used for purposes not listed in this medication guide.
Liothyronine side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Stop using liothyronine and call your doctor if you have symptoms of thyroid toxicity, such as chest pain, fast or pounding heartbeats, feeling hot or nervous, or sweating more than usual.
Also call your doctor at once if you have:
-
weak or shallow breathing;
-
confusion;
-
a feeling of being cold all the time;
-
changes in weight or appetite;
-
chest pressure spreading to your jaw or shoulder;
-
a light-headed feeling, like you might pass out;
-
severe headaches, ringing in your ears, dizziness, vision problems, pain behind your eyes;
-
a seizure; or
-
(in a child or teenager) pain, stiffness, and trouble moving the legs.
Common side effects of liothyronine may include:
-
trouble breathing;
-
headache;
-
tremors, feeling nervous or irritable;
-
muscle weakness;
-
increased appetite;
-
diarrhea;
-
irregular menstrual periods;
-
feeling hot;
-
rash; or
-
sleep problems (insomnia).
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Warnings
Liothyronine should not be used to treat obesity or weight problems.
You may not be able to use liothyronine if you have an adrenal gland problem that is not controlled by treatment.
Stop taking liothyronine and call your doctor if you have symptoms of thyroid toxicity, such as chest pain, fast or pounding heartbeats, feeling hot or nervous, or sweating more than usual.
Before taking this medicine
Since thyroid hormone occurs naturally in the body, almost anyone can take liothyronine. However, you may not be able to use this medicine if you have an adrenal gland problem that is not controlled by treatment.
Tell your doctor if you have ever had:
-
problems with your pituitary or adrenal gland;
-
heart disease, angina (chest pain);
-
a bleeding or blood clotting disorder;
-
diabetes; or
-
osteoporosis or low bone mineral density.
Tell your doctor if you are pregnant or breastfeeding.
Follow your doctor's instructions about using this medicine if you are pregnant. Controlling your thyroid hormone levels is very important during pregnancy, and your dose needs may be different during each trimester.
How should I take liothyronine?
Follow all directions on your prescription label and read all medication guides or instruction sheets. Use the medicine exactly as directed.
Older adults may be more sensitive to the effects of liothyronine, and doses are generally lower for people in this age group.
If you are switching to liothyronine from any other thyroid medicine, stop using the other medicine before you start taking liothyronine.
Liothyronine doses are based on weight (especially in children and teenagers). Your dose needs may change if you gain or lose weight.
When given as part of a thyroid suppression test, you will need to take liothyronine for several days in a row in preparation for the test. Tell your doctor if you miss any doses during this time.
Your thyroid function will need to be tested often. Even if you have no symptoms, tests can help your doctor determine if this medicine is effective.
If you need surgery, tell your surgeon you currently use this medicine. You may need to stop for a short time.
This medicine can affect the results of certain medical tests. Tell any doctor who treats you that you are using liothyronine.
Keep using this medicine as directed, even if you feel well. You may need to take thyroid medication for the rest of your life.
Store at room temperature away from moisture and heat.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose symptoms may include headache, sweating, diarrhea, irregular menstrual periods, confusion, weakness, swelling in your hands or feet, fast heart rate, chest pain, feeling short of breath, fainting, or feeling nervous, restless, or irritable.
What should I avoid while taking liothyronine?
Do not change brands or change to a generic product without first asking your doctor. Different brands of liothyronine may not work the same. If you get a prescription refill and your new pills look different, talk with your pharmacist or doctor.
What other drugs will affect liothyronine?
Some medicines can make liothyronine much less effective when taken at the same time. If you take any of the following medicines, take your liothyronine dose 4 hours before you take the other medicine.
Tell your doctor about all your current medicines. Many drugs can affect liothyronine, especially:
-
cancer medicine;
-
birth control pills or hormone replacement therapy;
-
cough or cold medicine;
-
an antidepressant;
-
steroid medicine;
-
seizure medicine;
-
insulin or oral diabetes medicine; or
This list is not complete and many other drugs may affect liothyronine. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
More about liothyronine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (99)
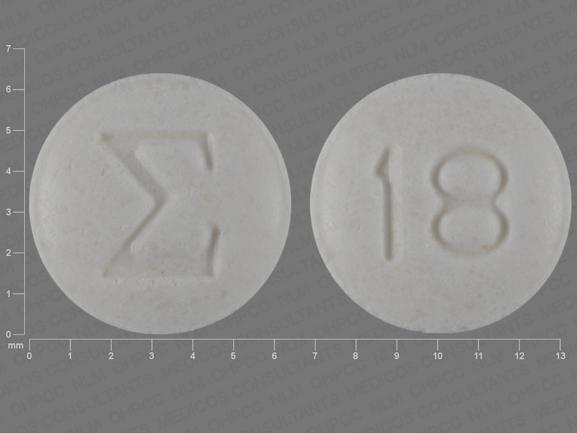
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: thyroid drugs
- Breastfeeding
- En español
Patient resources
- Liothyronine (Intravenous) advanced reading
- Liothyronine (Oral) (Advanced Reading)
- Liothyronine Tablets
- Liothyronine Injection
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 8.01.