Insulin Regular
Generic name: insulin regular [ IN-soo-lin-REG-yoo-lar ]
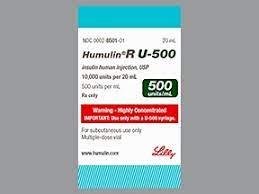
Brand names: HumuLIN R, Myxredlin, NovoLIN R
Drug class: Insulin
What is regular insulin?
Insulin is a hormone that is produced naturally in our bodies. Its main role is to allow cells throughout the body to uptake glucose (sugar) and convert it into a form that can be used by these cells for energy. Naturally occurring human insulin is made by beta cells within the pancreas, but people with diabetes have little or no natural insulin release.
Regular insulin is a short-acting insulin that takes 30 minutes to 1 hour to start working, peaks in 2 to 5 hours, and lasts for up to 6 hours. It may be used to improve blood sugar control in adults and children with diabetes mellitus and is usually always used in combination with an intermediate or long-acting insulin. Regular insulins are available in the U.S. without a prescription.
Insulin is mostly used to treat type 1 diabetes but can be used in people with type 2 diabetes if insulin levels remain low despite the use of other types of medications. Insulin may also be given to pregnant women who develop a type of diabetes during pregnancy called gestational diabetes.
Warnings
You should not use insulin if you are having an episode of hypoglycemia (low blood sugar).
Hypoglycemia, or low blood sugar, is the most common side effect of insulin. Symptoms include headache, hunger, dizziness, sweating, irritability, trouble concentrating, rapid breathing, fast heartbeat, fainting, or seizure (severe hypoglycemia can be fatal). Carry hard candy or glucose tablets with you in case you have low blood sugar.
Before taking this medicine
You should not use insulin regular if you are allergic to insulin, or if you are having an episode of hypoglycemia (low blood sugar).
Regular insulin is not approved for use by anyone younger than 2 years old. This medicine should not be used to treat type 2 diabetes in a child of any age.
Tell your doctor if you have ever had:
-
liver or kidney disease; or
Taking certain oral diabetes medicines while using insulin may increase your risk of serious heart problems. Tell your doctor if you also take medicine that contains pioglitazone or rosiglitazone.
Tell your doctor if you are pregnant or breastfeeding.
Follow your doctor's instructions about using regular insulin if you are pregnant or you become pregnant. Controlling diabetes is very important during pregnancy, and having high blood sugar may cause complications in both the mother and the baby.
How should I use regular insulin?
Use insulin exactly as directed. Follow all directions on your prescription label and read all medication guides or instruction sheets.
Regular insulin is injected under the skin. A healthcare provider may teach you how to properly use the medication by yourself. Regular insulin must not be given with a pump. Do not inject this medicine into a vein or a muscle.
Read and carefully follow any Instructions for Use provided with your medicine. Do not use insulin if you don't understand all instructions for proper use. Ask your doctor or pharmacist if you don't understand all instructions.
Prepare an injection only when you are ready to give it. Do not use if the medicine looks cloudy, has changed colors, or has particles in it. Call your pharmacist for new medicine.
Your care provider will show you where on your body to inject this medicine. Use a different place each time you give an injection. Do not inject into the same place two times in a row.
Do not inject this medicine into skin that is damaged, tender, bruised, pitted, thickened, scaly, or has a scar or hard lump.
After using regular insulin, you should eat a meal within 30 minutes.
Never share a syringe with another person, even if the needle has been changed. Sharing syringes can allow infections or disease to pass from one person to another.
You may have low blood sugar (hypoglycemia) and feel very hungry, dizzy, irritable, confused, anxious, or shaky. To quickly treat hypoglycemia, eat or drink a fast-acting source of sugar (fruit juice, hard candy, crackers, raisins, or non-diet soda).
Your doctor can prescribe a glucagon emergency injection kit to use in case you have severe hypoglycemia and cannot eat or drink. Be sure your family and close friends know how to give you this injection in an emergency.
Also watch for signs of high blood sugar (hyperglycemia) such as increased thirst or urination, blurred vision, headache, and tiredness.
Blood sugar levels can be affected by stress, illness, surgery, exercise, alcohol use, medications, or skipping meals. Ask your doctor before changing your dose or medication schedule.
Insulin is only part of a complete treatment program that may also include diet, exercise, weight control, blood sugar testing, and special medical care. Follow your doctor's instructions very closely.
In case of emergency, wear or carry medical identification to let others know you have diabetes.
Keep this medicine in its original container protected from heat and light. Do not freeze or store near the cooling element in a refrigerator. Throw away any insulin that has been frozen.
Storing unopened (not in use) pens of vials:
-
Refrigerate and use until expiration date; or
-
Store at room temperature and use within the number of days shown in your Instructions for Use.
Storing opened (in use) pens or vials:
-
Store at room temperature and use within the number of days shown in your Instructions for Use.
Use a needle and syringe only once and then place them in a puncture-proof "sharps" container. Follow state or local laws about how to dispose of this container. Keep it out of the reach of children and pets.
What happens if I miss a dose?
Use the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not use two doses at one time.
Keep insulin on hand at all times. Get your prescription refilled before you run out of medicine completely.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. Insulin overdose can cause life-threatening hypoglycemia. Symptoms include drowsiness, confusion, blurred vision, numbness or tingling in your mouth, trouble speaking, muscle weakness, clumsy or jerky movements, seizure (convulsions), or loss of consciousness.
What should I avoid while using regular insulin?
Do not change the brand of insulin or syringe you are using without first talking to your doctor or pharmacist. Some brands are interchangeable, while others are not. Your doctor and/or pharmacist know which brands can be substituted for one another.
Insulin can cause low blood sugar. Avoid driving or operating machinery until you know how this medicine will affect you.
Avoid medication errors by always checking the medicine label before injecting your dose.
Avoid drinking alcohol. It can interfere with your diabetes treatment.
Regular insulin side effects
Get emergency medical help if you have signs of insulin allergy: redness, swelling, sweating, itchy skin rash over the entire body, trouble breathing, fast heartbeats, feeling like you might pass out, or swelling in your tongue or throat.
Call your doctor at once if you have:
-
low potassium - leg cramps, constipation, irregular heartbeats, fluttering in your chest, increased thirst or urination, numbness or tingling, muscle weakness or limp feeling.
Common insulin side effects may include:
-
low blood sugar;
-
swelling in your hands or feet;
-
weight gain; or
-
thickening or hollowing of the skin where you injected the medicine.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
What other drugs will affect regular insulin?
Many other medicines can affect your blood sugar, or increase/decrease the effects of insulin. Some drugs can also cause you to have fewer symptoms of hypoglycemia, making it harder to tell when your blood sugar is low. Tell your doctor about all your current medicines and any medicine you start or stop using. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed here.
Popular FAQ
How and where should I inject insulin?
Injecting insulin is not difficult, but it does take a bit of practice. There are three main sites where insulin can be injected: the stomach area except for a 2-inch circle around your navel, and the soft part of your waist, but not anywhere near your spine; the top and outer part of your thighs, but not your inner thighs or anywhere close to your knee; the outer back of your upper arm where there is a pocket of fatty tissue. Continue reading
Can Trulicity be used with insulin?
Trulicity can be used with insulin, but because the combination of Trulicity and insulin increases the risk of low blood sugar levels (hypoglycemia), the dosage of insulin may need to be reduced. Continue reading
What are the different types of insulin?
Insulins are usually grouped as fast-acting, intermediate-acting, or long-acting. Within these groups, they can be further classified as human insulin and human insulin analogs. An insulin analog is a human insulin that has one or two amino acids changed which affects how quickly it is absorbed after injection and how fast or slow it acts. Insulin analogs are usually given within 15 minutes of a meal or at the same time as food. Continue reading
More FAQ
- What is the difference between regular insulin and lispro (Humalog)?
- How long can Humulin be unrefrigerated?
- Is Humulin fast or long-acting insulin?
- How long does Humulin last?
- Can regular and lispro insulin (Humalog) be mixed?
References
More about insulin regular
- Check interactions
- Compare alternatives
- Reviews (23)
- Side effects
- Dosage information
- During pregnancy
- Drug class: insulin
Patient resources
- Insulin Regular (U-100) Cartridges & Prefilled Pens patient information
- Insulin Regular (U-100) Vials
- Insulin Regular (U-500) Prefilled Pens
- Insulin Regular IV Infusion
Other brands
Humulin R, Humulin R U-500 KwikPen, Humulin R U-500 (Concentrated), Myxredlin
Professional resources
Other brands
Humulin R, Novolin R, Humulin R U-500 (Concentrated)
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use insulin only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 9.04.