Gestational Diabetes
Medically reviewed by Drugs.com. Last updated on Nov 10, 2025.
What is gestational diabetes (GDM)?
GDM develops during pregnancy, usually in the second or third trimester. GDM causes your blood sugar level to rise too high. A high blood sugar level can harm you and your unborn baby. The level usually goes back to normal after the baby is born.
What causes GDM?
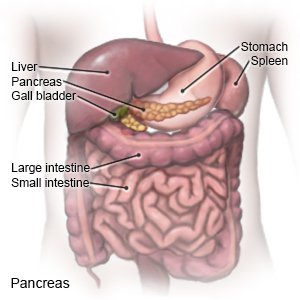
The cause of GDM is not known. Hormones made by the placenta may cause insulin resistance. Insulin helps move sugar out of the blood to be used for energy. Insulin resistance means your pancreas makes insulin, but your body cannot use it. As the placenta grows, more of these hormones are produced. The hormones block insulin and cause your blood sugar level to rise.
 |
What increases my risk for GDM?
- Lack of physical activity
- A family history of diabetes
- A history of high blood sugar, blood pressure, or cholesterol levels
- Overweight or obesity
- Past delivery of a large baby, or being pregnant with more than 1 baby
- Glycosuria (sugar in your urine) or polycystic ovary syndrome (PCOS)
- African American, American Indian, Asian American, or of Latin American or Pacific Islander heritage
What are the signs and symptoms of GDM?
- More hunger or thirst than usual
- Having to urinate often
- Blurred vision
- Feeling more tired than usual
- Bladder, vagina, or skin infections that happen often
- More weight gain than your healthcare provider suggests during your pregnancy
- Nausea or vomiting
How is GDM diagnosed?
An oral glucose tolerance test (OGTT) may be done at or after 24 weeks of pregnancy. Your healthcare provider may check you for GDM sooner if you are at high risk. Your provider may order either a 1-step or 2-step OGTT.
- 1-step OGTT: Your blood sugar level will be tested after you have not eaten for 8 hours (fasting). You will then be given a glucose drink. Your level will be tested again 1 hour and 2 hours after you finish the drink.
- 2-step OGTT: You do not have to fast for the first part of the test. You will have the glucose drink at any time of day. Your blood sugar level will be checked 1 hour later. If your blood sugar is higher than a certain level, another test will be ordered. You will fast and your blood sugar level will be tested. You will have the glucose drink. Your blood will be tested again 1 hour, 2 hours, and 3 hours after you finish the glucose drink.
How is GDM controlled?
GDM may be controlled with meal planning and physical activity. The goal is to keep your blood sugar level as close to normal, as safely as possible. Your healthcare provider and dietitian will help set up a meal and activity plan for you.
- Follow your meal plan as directed. Talk to a dietitian or healthcare provider about the best meal plan for you. Your plan may include 3 small meals and 2 to 4 snacks every day. Control the amount of carbohydrates (such as bread, cereal, and fruit) you eat at each meal and snack. Too much carbohydrate in 1 meal or snack can cause your blood sugar to rise to a high level. Your dietitian or provider will tell you how much carbohydrate to eat at each meal and snack. Eat foods that are a good source of fiber, such as vegetables and legumes (beans and lentils).

- Ask your provider about the best physical activity plan for you. Physical activity helps keep your blood sugar level steady. A good goal is to be active for at least 30 minutes, 5 days a week. Low-impact activities such as walking or swimming are effective.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What do I need to know about blood glucose monitoring?
Your diabetes care team provider may order blood glucose monitoring to check your levels several times each day. The checks will be done if you need to stay in the hospital, and you will need to check at home.
- Your provider will teach you how to check your blood sugar level. You will learn what to do if the level is too high or too low. Make a list of the times you checked your blood sugar level and the results of your checks. Take the list to all follow-up appointments.
- A glucose meter is a device that uses a test strip to check your blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your blood.

- A continuous glucose monitor (CGM) uses a sensor to check your blood sugar level. The sensor is placed on your abdomen or arm. A transmitter on the sensor gets a glucose reading. CGM data may be linked to an insulin pump.

- A glucose meter is a device that uses a test strip to check your blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your blood.
- Your provider will teach you what your level should be at certain times each day. Your fasting blood sugar level target may be 70 to 95 mg/dL. You will also need to check before and after you eat throughout the day. Your target may be 110 to 140 mg/dL 1 hour after you eat or 100 to 120 mg/dL 2 hours after you eat. Your provider may give you higher target levels if you are at risk for hypoglycemia. You will learn what to do if the level is too high or too low. Write down your results, and show them to your provider. Your provider may use the results to make changes to your medicine, food, and physical activity schedules.
What do I need to know about insulin?
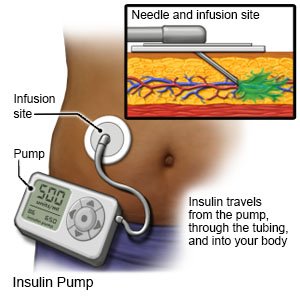
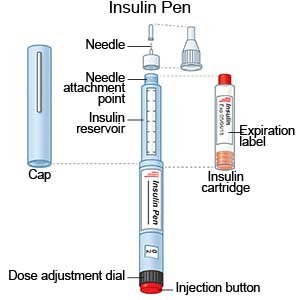
Insulin may be needed if your diabetes is not controlled by nutrition and physical activity. Insulin is safe to use during pregnancy. Insulin may be given through a pump or pen, or injected. You and your care team will discuss the best method for you:
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
- An insulin pen is a device prefilled with insulin. Most insulin pens are disposable. You throw the pen away after it is empty or used for a certain amount of time. Some pens have a replaceable cartridge filled with insulin. You keep the pen and only throw away the cartridge.
- Insulin injections are given with a needle and syringe. You and your family members will be taught how to draw up and give insulin if this is the best method for you. You will also be taught how to dispose of used needles and syringes.
What else can I do to manage GDM?
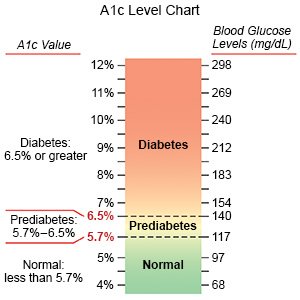
- Have your A1c level checked as often as directed. A hemoglobin A1c is a blood test that measures your average blood sugar level for the past 2 to 3 months. It is also called an HbA1c or glycohemoglobin test. The level is given as a percentage. An A1c of 6% or lower is usually recommended during pregnancy. If you are at risk for hypoglycemia, your goal may be between 6% and 7%. Changes to your nutrition, physical activity, or medicine plan may be made to help you reach your goal.
- Check your blood pressure (BP) as often as directed. BP readings are usually written as 2 numbers, such as 120/80. The first number is the systolic BP, and the second is the diastolic BP. If you did not have high BP before pregnancy, your systolic BP should be between 110 and 135. Your diastolic BP should be between 60 and 85. If you did have high BP before pregnancy, your systolic BP should be between 120 and 140. Your diastolic BP should be between 80 and 90. Check your BP 2 times, 1 minute apart. Keep a record of your readings and bring it to your follow-up visits.

- Maintain a healthy weight. A healthy weight can help you control your GDM. Ask your healthcare provider how much weight is healthy for you to gain during your pregnancy. If your weight was higher than recommended before you became pregnant, your provider may recommend a safe weight loss plan during pregnancy. Your provider or a dietitian can help you create a healthy meal plan for you and your baby. Do not try to go on a crash diet or try to lose weight without your provider's approval. You may not get enough calories or nutrients for you and your baby.
- Do not smoke. Nicotine is dangerous for you and your baby and can make it harder to manage GDM. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your provider for information if you currently smoke and need help quitting.
- Have diabetes screening after you give birth, as directed. Screening may be done 4 to 12 weeks after your baby is born. This is to check if you have developed diabetes, problems with your fasting glucose levels, or glucose intolerance. You may need other tests or treatment if you have any of these. Testing may be repeated every 1 to 3 years if you had GDM but normal tests within 12 weeks of giving birth.
Call your local emergency number (911 in the US) if:
- Your heartbeat is fast and weak, or your breathing is fast and shallow.
- You are more sleepy than usual or become confused.
- You have blurred or double vision.
When should I seek immediate care?
- Your breath has a fruity, sweet smell.
- You are shaking or sweating.
- Your blood sugar level is below 70 mg/dL or above 250 mg/dL and does not improve with treatment.
- You have a headache, or you are dizzy.
When should I call my doctor or diabetes care team provider?
- You think your baby is not moving as much as usual.
- You have more hunger or thirst than usual.
- You are urinating more often than usual.
- You have an upset stomach and are vomiting.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Gestational Diabetes
Treatment options
- Medications for Abnormal Glucose Tolerance
- Medications for Diabetes Mellitus
- Medications for Gestational Diabetes
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
