Diabetes and Pregnancy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about diabetes and pregnancy?
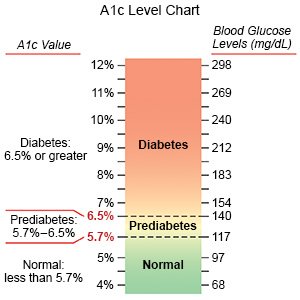
Plan your pregnancy so healthcare providers can help you have a healthy pregnancy and baby. Your diabetes care team providers may help you create meal and physical activity plans. The plans can help you control your A1c and glucose (blood sugar) levels. Your providers may recommend A1c levels less than 6.5% before you get pregnant, if possible. Good control before and during pregnancy helps lower the risk for health problems diabetes can cause.
What can I do to prepare for a healthy pregnancy?
- Have a physical exam. Your care team provider may recommend tests to make sure you are as healthy as possible. Tests may be used to check for sexually transmitted infections, thyroid disease, or complications of diabetes, such as retinopathy. If you already have retinopathy, you will be checked often to make sure it does not get worse. Depending on your age and family history, your provider may also recommend screenings to check for genetic conditions.
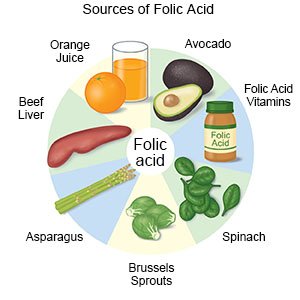
- Start taking folic acid supplements as directed. Folic acid helps prevent certain conditions, such as spina bifida. Your provider will tell you how long before you become pregnant to start. Your provider will recommend prenatal vitamins that contain folic acid and tell you how much folic acid you need each day.
- Talk with your provider if you currently use any medicines, drugs, or alcohol. Include prescription and over the counter medicines and supplements. Your provider will tell you if you should stop any before you become pregnant. Tell your provider if you currently smoke cigarettes, vape, drink alcohol, or use street drugs. These are not safe for your unborn baby. Your provider can help you quit.
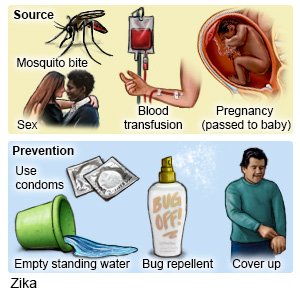
- Tell your provider if you have upcoming travel plans. You should not travel to an area where the Zika virus is common. The Zika virus can be passed from a mother to her unborn baby. This may cause birth defects such as poor brain development or pregnancy loss. There is no vaccine to prevent Zika virus infection. The Zika virus can stay in your body for several months. Tell your provider if you recently traveled to an area where Zika is common. You may need to be tested for Zika before you become pregnant.
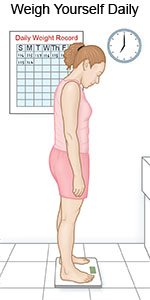
- Reach or maintain a healthy weight. Your provider can tell you if your weight is healthy. Your provider may recommend that you lose or gain weight before you become pregnant. A healthy weight helps control blood sugar and blood pressure. A healthy weight also lowers the risk for problems such as premature labor.
- Learn about pregnancy and nutrition. A dietitian can help you plan healthy meals to control your blood sugar and A1c levels before pregnancy. The dietitian can also help you plan for changes during and after pregnancy. Your calorie needs depend on your weight before pregnancy. Your dietitian will tell you how many calories you need each day.
- Ask about physical activity. Physical activity, such as exercise, helps with weight management and blood sugar control. Make physical activity a routine before you become pregnant.
- Ask about vaccines you may need. Some diseases are dangerous for unborn babies. Some vaccines are given routinely before pregnancy, such as the hepatitis B vaccine. You may also need the hepatitis A vaccine. You will also be given 1 dose of Tdap (tetanus, diphtheria, and pertussis) when you are 27 to 36 weeks along. The flu, rubella, chickenpox, and COVID-19 vaccines are also recommended during pregnancy. Tell your provider about all vaccines you have had, or if you do not know your vaccine history. Your provider will recommend vaccines for you. Your provider will also tell you how long after you get a vaccine to wait before you become pregnant, if needed.
How can I manage diabetes during pregnancy?
During pregnancy and after delivery, your obstetrician (OB) becomes part of your care team. Tell your OB about your diabetes care team providers. Your team will provide a plan for your care during your pregnancy. Your diabetes care team provider may order blood glucose checks several times each day. These checks will be done if you need to stay in the hospital. You will also need to check at home. Your team will help you with the following:
- Continue to take folic acid supplements until you are at least 12 weeks pregnant. Your providers will tell you how much folic acid you need each day.
- Check your blood sugar levels as directed. Ask your providers when and how often you should check. Your fasting blood sugar target may be 70 to 95 mg/dL. You will also need to check before and after you eat throughout the day. Your target may be 110 to 140 mg/dL 1 hour after you eat or 100 to 120 mg/dL 2 hours after you eat. Write down your results and show them to your provider. Your providers may use the results to adjust your medicine, food, and physical activity plans.

- Use a continuous glucose monitoring (CGM) device, if recommended. A CGM device works with a glucose monitor. A sensor is placed in your abdomen or on your arm. You put a transmitter on the sensor to get a reading that shows up on the monitor. You will learn what to do if your level is too high or too low. Write down the times of your checks and your levels. Bring them to all follow-up appointments.

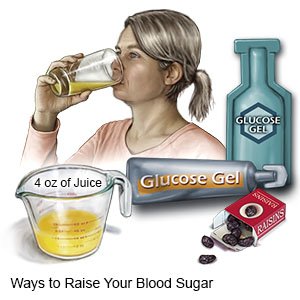
- Help prevent hypoglycemia. Your risk is higher during pregnancy because you may not feel the symptoms. This risk is highest during the first trimester. Eat regular meals and snacks to avoid hypoglycemia. Always keep glucose tablets with you in case your blood sugar level gets low. If you do not have glucose tablets, drink milk, juice, or regular soda. Tell your family about the symptoms of hypoglycemia so they can help you if you cannot help yourself. Ask your care team provider how to manage hypoglycemia.
- Have your A1c checked as often as directed. An A1c of 6% or lower is usually recommended during pregnancy. Your target level may be between 6% and 7% if you are at risk for hypoglycemia. Your care team can help you reach or maintain your target A1c level.
- Ask about medicines. Some medicines are not safe to take during pregnancy. If you have type 2 diabetes and take diabetes pills, you may need to stop taking them and start using insulin. Insulin is safe to use during pregnancy.
- Check your blood pressure (BP) as often as directed. BP readings are written as 2 numbers, such as 120/80. The first number is the systolic BP, and the second is the diastolic BP. If you did not have high BP before pregnancy, your systolic BP should be between 110 and 135. Your diastolic BP should be between 60 and 85. If you had high BP before pregnancy, your systolic BP should be between 120 and 140. Your diastolic BP should be between 80 and 90. Check your BP 2 times, 1 minute apart. Keep a record of your readings and bring it to your follow-up visits.

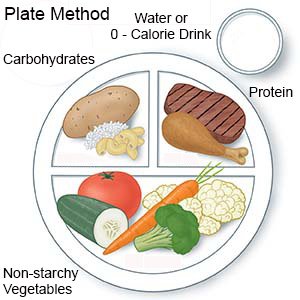
- Gain the recommended amount of weight. The amount depends on your weight when you became pregnant. Your providers may help you make a new meal plan. The plan will include healthy foods, such as non-starchy vegetables and lean protein. The plan will also havethe right amount of carbohydrates for you. Examples of carbohydrates are potatoes, pasta, and whole grains. Your plan may allow a serving of low-fat dairy or a small fruit as a carbohydrate. Healthy foods may also help you reach or maintain your target blood sugar levels.
- Continue to get regular physical activity. Physical activity can help control your blood sugar level and blood pressure. Your provider will tell you which activities are safe during pregnancy. Your provider will help you create a safe physical activity plan.
- Help prevent diabetic ketoacidosis (DKA). This is a serious condition that can happen when your blood sugaris too high. Pregnancy increases your risk for DKA. The symptoms of DKA include stomach pain, nausea, vomiting, and confusion. Your care team provider may suggest that you test the ketone levels in your urine when your blood sugar is high. Your provider may also ask you to check your ketones regularly if you are sick.
What else can I do to have a healthy baby?
- Keep all appointments with your care team providers. They will help you manage your diabetes during pregnancy. You may need to see your care team provider every 1 to 2 weeks during the first and second trimesters. As the end of your pregnancy gets closer, you may need to see your provider each week. During these exams, your provider may check your eyes, your A1c levels, and how you and your baby are doing.
- Do not smoke. Nicotine is harmful to your baby and makes it more difficult to manage your diabetes. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your care team provider for information if you currently smoke and need help to quit.
- Do not drink alcohol. Alcohol is dangerous for your unborn baby. Alcohol can also increase your blood sugar levels and make your diabetes harder to manage. Ask your care team provider for help if you need information or support to quit drinking alcohol.
 |
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Related medications
How will my diabetes be managed during and after delivery?
Healthcare providers will check your blood sugar levels while you are in labor. They will give you insulin or glucose to keep your blood sugar at the right level. Do the following after delivery:
- Go to all follow-up appointments. Your care team providers will continue to help you manage your diabetes after delivery. Talk with your provider about birth control options. It is important to prepare for your next pregnancy if you plan to have another child.
- Take your medicine as directed. If you have type 2 diabetes, you may be able to take your diabetes medicine again. If you have type 1 diabetes, the amount of insulin you need will decrease after delivery. You may not be able to take certain medicines if you breastfeed. Ask your care team provider when and how often to test your blood sugar levels. You will need to check several times each day. Examples include before you eat or drink anything (fasting), after meals, and during activity.
- Help prevent hypoglycemia if you breastfeed. Your risk for hypoglycemia is higher if you breastfeed. Your dietitian will help you create a meal plan that works for you. Eat a snack before you breastfeed. Eat regular meals and snacks to keep your blood sugar level steady.
What are the risks of diabetes and pregnancy?
You have an increased risk for high blood pressure, eye disease, premature (early) labor, and miscarriage. A miscarriage is the loss of a fetus before 20 weeks of pregnancy. High blood sugar levels can increase your risk for having a large baby, a baby with birth defects, and stillbirth. Stillbirth is the loss of a fetus (unborn baby) after 20 weeks of pregnancy.
When should I seek immediate care?
- Your blood sugar level is over 200 mg/dL and you have stomach pain, nausea, vomiting, or confusion.
When should I call my doctor or care team provider?
- You are shaky or dizzy.
- You are sweaty or have a headache.
- You have changes in your vision.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Diabetes and Pregnancy
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
