Niacin (Antilipemic) (Monograph)
Drug class: Antilipemic Agents, Miscellaneous
Introduction
Niacin (nicotinic acid) is a water-soluble, B complex vitamin; certain niacin preparations are used as antilipemic agents.
Niacin preparations available as dietary supplements should not be used interchangeably with prescription-only niacin preparations.
Uses for Niacin (Antilipemic)
Niacin is used as an adjunct to nondrug therapies (i.e., lifestyle modifications) for prevention of cardiovascular events and for the management of dyslipidemias.
Prevention of Cardiovascular Events
Secondary Prevention
Niacin is used as an adjunct to dietary therapy in patients with a history of myocardial infarction (MI) and hyperlipidemia to reduce the risk of recurrent nonfatal MI.
The 2018 American Heart Association (AHA)/American College of Cardiology (ACC) cholesterol management guideline emphasizes lifestyle modification as the foundation of cardiovascular risk reduction. If pharmacologic therapy is needed, hydroxymethyl-glutaryl-CoA (HMG-CoA) reductase inhibitor (statin) therapy is recommended. Statins are considered the first-line drugs of choice for reducing low-density lipoprotein (LDL) cholesterol, the lipoprotein fraction found to be a major cause of clinical atherosclerotic cardiovascular disease (ASCVD). Nonstatin drugs may be considered as adjunctive therapy in certain high-risk patients who do not achieve adequate reductions in LDL-cholesterol concentrations with maximally tolerated statin therapy; however, other drugs (e.g., ezetimibe) are generally recommended for this use. Although niacin can produce mild LDL-lowering effects, randomized controlled studies do not support its use as add-on therapy to statins.
Efficacy of niacin in reducing the risk of recurrent MI has been established in a large, multicenter, placebo-controlled study (Coronary Drug Project). During 5–8.5 years of observation in men with previous MI, therapy with 3 g of niacin daily was shown to reduce the incidence of definite, nonfatal MI. During this period, niacin therapy had no effect on overall or cause-specific mortality rates when compared with placebo, although the 5-year rate of death secondary to coronary heart disease (CHD) was slightly lower in the niacin-treated group. However, follow-up of surviving patients 5–9 years after discontinuance of drug therapy indicated that previous niacin therapy was associated with a long-term overall reduction in mortality when compared with placebo, possibly secondary to the reduction in nonfatal MI observed during the treatment period or to a long-term benefit from the drug’s effects on lipoproteins.
The addition of niacin to statin-based therapy has not been shown to provide an incremental benefit on cardiovascular morbidity and mortality beyond that already demonstrated with statin-based therapy. In the Impact on Global Health Outcomes (AIM-HIGH) study, the combination of extended-release niacin (1.5–2 g daily) and statin-based therapy (simvastatin 40–80 mg once daily, with or without ezetimibe 10 mg daily) was compared with statin-based therapy alone in patients with established cardiovascular disease (i.e., documented stable CHD, cerebrovascular or carotid disease, peripheral arterial disease). Despite a favorable effect on serum lipid concentrations (median high-density lipoprotein [HDL]-cholesterol concentration increased from 35 to 42 mg/dL, triglyceride concentration decreased from 164 to 122 mg/dL, and LDL-cholesterol concentration decreased from 74 to 62 mg/dL), the addition of niacin to simvastatin-based therapy did not further reduce the incidence of the primary end point (i.e., composite of death from CHD, nonfatal MI, ischemic stroke, hospitalization for more than 23 hours for an acute coronary syndrome, or symptom-driven coronary or cerebral revascularization) compared with statin-based therapy alone over a follow-up period of 36 months. The addition of extended-release niacin to existing simvastatin-based therapy, however, did increase the risk of adverse effects (e.g., pruritus, flushing, adverse GI effects, increased blood glucose concentrations). The investigators of this study stated that whether such combination therapy provides incremental benefit in higher-risk patients or in those receiving suboptimal statin therapy remains to be established.
Data from another large randomized, double-blind, multicenter study involving 25,673 adults with cardiovascular disease confirmed findings of the AIM-HIGH study. In the Heart Protection Study 2–Treatment of HDL to Reduce the Incidence of Vascular Events (HPS2-THRIVE), the combination of extended-release niacin/laropiprant (2 g/40 mg daily) (no longer commercially available ) and statin therapy (simvastatin 40 mg once daily, with or without ezetimibe 10 mg daily) was compared with statin therapy alone in patients with established cardiovascular disease (i.e., history of MI, cerebrovascular disease, PAD, diabetes mellitus with evidence of symptomatic coronary disease). Despite a favorable effect on serum lipid concentrations (additional 6-mg/dL increase in HDL-cholesterol concentration, 33-mg/dL reduction in triglyceride concentration, and 10-mg/dL reduction in LDL-cholesterol concentration), the addition of niacin/laropiprant to simvastatin-based therapy did not further reduce the incidence of major cardiovascular events (i.e., nonfatal MI, death from coronary causes, stroke of any type, coronary or noncoronary revascularization) compared with simvastatin-based therapy alone over a median follow-up of 3.9 years. The addition of niacin/laropiprant to existing simvastatin-based therapy, however, did increase the risk of severe adverse effects, including disturbances in glycemic control requiring hospitalization, development of diabetes mellitus, adverse GI effects, myopathy, gout, rash, skin ulceration, and, unexpectedly, infection and bleeding. In light of these findings, some clinicians state that niacin should be reserved as a fourth-line agent (after intensive lifestyle modifications, fibric acid derivatives, and omega-3-acid ethyl esters) for patients with severe hypertriglyceridemia in whom the primary goal of treatment is prevention of pancreatitis.
Reducing Progression of Coronary Atherosclerosis
Niacin, in combination with a bile acid sequestrant, also is used to slow the progression or promote regression of atherosclerosis in patients with clinical evidence of CHD and hyperlipidemia.
In the Familial Atherosclerosis Treatment Study (FATS), combined therapy with a bile acid sequestrant (colestipol) and either niacin or lovastatin for 2.5 years resulted in decreased progression of coronary atherosclerosis, an increased frequency of coronary atherosclerotic regression, and a reduced incidence of cardiovascular events (e.g., death, myocardial infarction, or the need for revascularization procedures for worsening symptoms) in high-risk men with CHD. Although coronary artery stenosis was reduced by an average of only 1.1 or 0.3% by combined niacin-colestipol or lovastatin-colestipol therapy, respectively, the incidence of clinical cardiovascular events in the 2 drug treatment groups combined was reduced by 73% compared with the placebo group. This disproportionality between the extent of improvement in coronary artery stenosis resulting from cholesterol reduction and decreases in cardiovascular morbidity and mortality also has been noted in other studies, suggesting that other effects of cholesterol reduction (e.g., stabilization of atherosclerotic plaque against rupture, improved coronary endothelial vasomotor function) may potentially contribute to a reduction in ischemic events in patients receiving antilipemic therapy.
In the Cholesterol-Lowering Atherosclerosis Study (CLAS), combined therapy with immediate-release niacin (average dosage 4.3 g daily) and colestipol (average dose 29.5 g daily) for 2–4 years in hypercholesterolemic men with previous coronary bypass surgery resulted in decreased progression of coronary atherosclerosis (measured as the number of lesions that progressed, formation of new lesions in native coronary arteries or in bypass grafts, or any adverse change in bypass grafts) and an increased frequency of coronary atherosclerotic regression.
Dyslipidemias
Intolerable adverse effects may limit the usefulness of niacin therapy in patients with dyslipidemia, and some clinicians reserve niacin as alternative therapy when drugs with fewer and less severe adverse effects do not achieve the desired result.
Primary Hypercholesterolemia and Mixed Dyslipidemia
Niacin is used as an adjunct to dietary therapy to decrease elevated serum total and LDL-cholesterol, apo B, and triglyceride concentrations, and to increase HDL-cholesterol concentrations in the treatment of primary hyperlipidemia and mixed dyslipidemia, including heterozygous familial hypercholesterolemia and other causes of hypercholesterolemia (e.g., polygenic hypercholesterolemia).
Niacin may be used in combination with a bile acid sequestrant to decrease elevated serum total and LDL-cholesterol concentrations in patients with primary hyperlipidemia.
Statins are considered the initial drugs of choice when drug therapy is indicated for the management of hyperlipidemia in adults with increased LDL-cholesterol concentrations. Data from several large randomized studies indicate that the addition of niacin to statin therapy does not further reduce the incidence of major cardiovascular events but may increase the risk of severe adverse effects.
Reductions in cholesterol and triglyceride concentrations produced by usual dosages of niacin substantially exceed those achieved with placebo. Mean reductions of 3–18% in plasma LDL-cholesterol concentration, 5–38% in triglyceride concentration, and increases of 10–32% in HDL-cholesterol concentration have been reported in various controlled studies in patients with primary hyperlipidemia or mixed dyslipidemia who received extended-release niacin (Niaspan) 500–2000 mg daily at bedtime for at least 4 weeks. An analysis of pooled data from these studies indicate that women may exhibit a greater antilipemic response to Niaspan than men; LDL-cholesterol and triglyceride concentrations were reduced by 5–18 and 9–36%, respectively, in women and 2–15 and 3–30%, respectively, in men. Increases in HDL-cholesterol concentrations also were greater among women than men (8–26% versus 11–23%).
The addition of a bile acid sequestrant or a statin to niacin therapy has been shown to further reduce LDL-cholesterol concentrations in patients with primary hyperlipidemia or mixed dyslipidemia. In a long-term, open-label study in such patients, combined therapy for 48–96 weeks with extended-release niacin and a bile acid sequestrant or a statin was associated with overall LDL-cholesterol reductions of 20–28 and 32%, respectively; these reductions averaged 2–10 or 14% greater, respectively, than those achieved with niacin monotherapy after 48–96 weeks. In patients with primary hypercholesterolemia or mixed dyslipidemia who received extended-release niacin (1–2 g daily) in fixed combination with lovastatin (20–40 mg daily) for at least 12 weeks, LDL-cholesterol or triglyceride concentrations were reduced by 30–42 or 32–44%, respectively, and HDL-cholesterol concentrations were increased by 20–30%. Additional reductions in total cholesterol, LDL-cholesterol, and triglyceride concentrations also were reported in patients with CHD who received combined therapy with niacin and a statin for 2.5 years. It should be noted that, in patients with established cardiovascular disease, the combination of niacin and statin-based therapy has not been shown to provide additional ASCVD risk reduction benefit beyond that already established with statin-based therapy.
Hypertriglyceridemia
Niacin is used as adjunctive therapy in the management of severe hypertriglyceridemia in patients at risk of developing pancreatitis (typically those with serum triglyceride concentrations exceeding 2000 mg/dL and elevated concentrations of VLDL-cholesterol and fasting chylomicrons) who do not respond adequately to dietary management. The drug also may be used in patients with triglyceride concentrations of 1000–2000 mg/dL who have a history of pancreatitis or of recurrent abdominal pain typical of pancreatitis. The effect of niacin therapy on risk of pancreatitis in patients with type IV hyperlipoproteinemia and triglyceride concentrations less than 1000 mg/dL who exhibit type V patterns subsequent to dietary or alcoholic indiscretion has not been adequately studied. Niacin is not indicated for use in patients with type I hyperlipoproteinemia who have elevated triglyceride and chylomicron concentrations but normal VLDL-cholesterol concentrations.
The 2018 AHA/ACC cholesterol management guideline recommends nonpharmacologic therapy (e.g., lifestyle modification) and management of underlying factors whenever possible in adults with moderate hypertriglyceridemia (fasting or nonfasting triglyceride concentrations of 175–499 mg/dL). Because most patients with severe hypertriglyceridemia (fasting triglyceride concentrations of 500 mg/dL or greater) have multiple risk factors for ASCVD and are at increased risk of developing atherosclerotic disease, the guidelines state that it is reasonable to initiate statin therapy in selected patients with severe hypertriglyceridemia. Niacin may be useful as adjunctive therapy in some patients with severe hypertriglyceridemia because of the drug's triglyceride-lowering effects.
The principal aim of therapy in patients with very high triglyceride concentrations (500 mg/dL or greater) is to prevent acute pancreatitis; therefore, these patients should be treated more intensively to prevent development of acute pancreatitis. Before initiating antilipemic therapy, patients with triglyceride concentrations of 500 mg/dL or greater should be evaluated to rule out secondary causes of hyperlipidemia.
Niacin (Antilipemic) Dosage and Administration
Administration
Niacin is administered orally. As an antilipemic agent, immediate-release niacin (Niacor) preferably is administered orally with meals. Extended-release niacin (Niaspan) should be administered at bedtime following a low-fat snack. In addition, the manufacturers state that Niaspan tablets should be taken whole and should not be broken, crushed, or chewed before swallowing.
Concomitant administration of niacin with alcohol, hot drinks, or spicy foods may increase the risk of flushing or pruritus; these beverages or foods should be avoided at the time of drug ingestion.
Dosage
Dosage of niacin must be carefully adjusted according to the patient’s response and tolerance.
Because the pharmacokinetics and, therefore, metabolism of different formulations (i.e., immediate-release, extended-release) of niacin may vary, the manufacturers state that these preparations should not be used interchangeably.
Symptoms of flushing, pruritus, and GI distress associated with niacin therapy may be reduced by initiating therapy with low dosages, gradual escalation of dosage, and avoiding administration of niacin on an empty stomach. Because niacin-induced cutaneous vasodilation appears to be mediated by prostaglandins (e.g., prostacyclin, prostaglandin D2), pretreatment with an inhibitor of prostaglandin synthesis (e.g., aspirin up to the recommended dose of 325 mg administered up to approximately 30 minutes prior to administration of niacin) may reduce flushing.
Dyslipidemias
Immediate-Release Niacin
Some experts state that the usual adult dosage of immediate-release niacin for the management of hyperlipoproteinemia is 1.5–3 g daily given in 2–3 divided doses.
The manufacturer of Niacor recommends an immediate-release niacin dosage of 1–2 g 2 or 3 times daily in adults; therapy with Niacor may be initiated with 250 mg of niacin as a single daily dose following the evening meal, and the frequency of dosing and total daily dosage may be increased at 4- to 7-day intervals until the desired antilipemic effect is achieved or the first-level therapeutic dosage of 1.5–2 g daily is reached. Other clinicians recommend initiating therapy with 100 mg of niacin 3 times daily and increasing the dose by 300 mg daily at 4- to 7-day intervals; alternatively, therapy may be initiated with 500 mg of niacin 3 times daily and dosage increased gradually until the desired antilipemic effect is achieved. If an adequate response is not achieved after 2 months of therapy, dosage of niacin may be increased at 2- to 4-week intervals to 3 g daily (1 g 3 times daily). Some patients may require a higher dosage, and at least one manufacturer states that total dosage of immediate-release niacin generally should not exceed 6 g daily.
Extended-release Niacin
The usual initial dosage of extended-release niacin (Niaspan) is 500 mg daily at bedtime following a low-fat snack. If an adequate response is not achieved after 4 weeks of therapy, dosage may be increased by no more than 500 mg at 4-week intervals until the desired effect on lipoprotein concentrations is observed or a maximum daily dosage of 2 g is reached. The usual adult maintenance dosage of Niaspan is 1–2 g daily at bedtime.
The manufacturer of Niaspan states that dosage generally should be titrated as with initial therapy in patients previously treated with immediate-release niacin preparations or in those in whom therapy with Niaspan has been discontinued for an extended period.
Dosage in Renal and Hepatic Impairment
Niacin should be used with caution in patients with renal or hepatic impairment. In addition, the drug also should be used with caution in patients who consume substantial amounts of alcohol and/or who have a history of liver disease; such patients should be closely monitored. Use of niacin is contraindicated in patients with active liver disease or unexplained, persistent increases in serum aminotransferase concentrations.
Cautions for Niacin (Antilipemic)
At usual antilipemic dosages, niacin generally is well tolerated, and adverse effects have been mild and transient. Most adverse effects of niacin are dose related and generally subside with reduction in dosage. The most common adverse effects in the dosages used to treat dyslipidemia are GI upset, flushing (especially of the face and neck), and pruritus. In controlled clinical trials, approximately 15% of patients receiving extended-release niacin (Niaspan) discontinued the drug because of adverse effects.
Cardiovascular Effects
Flushing (i.e., warmth, redness, itching, and/or tingling) reportedly occurs in approximately 53–91% of patients who received niacin in controlled clinical trials. Although the incidence of flushing appears to be similar among patients treated with immediate- or extended-release niacin, fewer episodes of flushing were reported by patients who received the extended-release preparation (Niaspan) (1.88 versus 8.56 episodes per patient). In controlled clinical trials, approximately 6% of patients receiving extended-release niacin (Niaspan) discontinued the drug because of flushing.
Flushing usually occurs within 20 minutes or 2–4 hours after administration of immediate-release (e.g., Niacor) or extended-release (Niaspan) niacin, respectively, and generally persists for 0.5–1.5 hours; flushing usually subsides after several weeks of consistent niacin use. Flushing episodes often may be accompanied by symptoms of dizziness, tachycardia, palpitations, shortness of breath, sweating, chills, and/or edema, that rarely may result in syncope. A sensation of burning, stinging or tingling of the skin, increased sebaceous gland activity, nausea, bloating, flatulence, hunger pains, vomiting, heartburn, and diarrhea also have occurred. Within 2–6 weeks after initiating chronic oral high-dose niacin therapy, the flushing and skin sensations, increased sebaceous gland activity, and increased GI motility disappear in most patients.
Tolerance to niacin-induced flushing may be increased if patients are advised of the likelihood of its occurrence during initiation of therapy. Avoidance of hot beverages, which may exacerbate flushing, during initiation of niacin therapy may reduce the occurrence of this adverse effect. Use of an extended-release niacin preparation (Niaspan) to lessen adverse effects has been suggested; however, use of this preparation has been shown to reduce only the frequency (i.e., number of episodes per patient) but not the incidence of flushing. In one study in patients receiving 3 g of niacin daily as immediate-release tablets or extended-release capsules, the frequency of flushing was slightly less in patients receiving the extended-release capsules versus the tablets, but patient compliance was substantially less with the extended-release preparation principally because of intolerable GI effects.
Other cardiovascular adverse effects, including atrial fibrillation and other cardiac arrhythmias, hypotension, orthostasis, vasovagal attacks, and generalized edema, also have been reported with niacin therapy.
GI Effects
The most frequent adverse GI effects of niacin are diarrhea, nausea, and vomiting. Abdominal pain and dyspepsia occurred in about 2–6% of patients receiving the drug in controlled clinical trials. Constipation, flatulence, eructation, anorexia, heartburn, activation of peptic ulcers, and/or peptic ulceration have been reported in patients receiving niacin therapy; bloating, hunger pains, or xerostomia also has been reported.
Hepatic Effects
Abnormal liver function test results (including increased serum bilirubin, AST [SGOT], ALT [SGPT], and LDH concentrations), jaundice, and chronic liver damage have occurred during niacin therapy. Reversible increases in serum aminotransferase concentrations to more than 3 times the upper limit of normal have been reported in up to 52% of patients receiving sustained-release preparations of niacin. Elevations in serum aminotransferase concentrations appear to be dose related and usually return slowly to pretreatment values following discontinuance of niacin.
Some evidence suggests that the frequency and severity of adverse hepatic effects are dose dependent and may be increased with sustained- or extended-release preparations of the drug. However, hepatotoxicity also has been reported with relatively low dosages of niacin and relatively early in a course of therapy. In addition, although hepatotoxicity is uncommon and usually mild and reversible, cases of severe hepatotoxicity, including fulminant hepatic necrosis, have occurred in patients who have substituted sustained-release niacin preparations for equivalent dosages of immediate-release niacin. Therefore, different formulations (immediate-release, extended-release) of niacin should not be used interchangeably, and dietary supplement niacin preparations should not be used for cholesterol lowering or as substitutes for prescription-only niacin preparations.
Hypoalbuminemia, cholelithiasis, jaundice, hepatitis, and hepatic failure have also been reported in patients receiving niacin therapy.
Musculoskeletal Effects
Elevations in serum creatine kinase (CK, creatine phosphokinase, CPK), myalgia, myopathy, and rhabdomyolysis have been reported in patients receiving niacin alone or combined with other antilipemic agents (e.g., gemfibrozil, various statins).
Dermatologic and Sensitivity Reactions
Pruritus and rash are the most common dermatologic reactions of niacin, occurring in up to 12% of patients receiving the drug in controlled clinical trials. Hyperpigmentation, acanthosis nigricans, urticaria, dry skin, and sweating, also have been reported with niacin therapy.
Hypersensitivity reactions (e.g., anaphylaxis, angioedema, urticaria, flushing, dyspnea, tongue edema, laryngeal edema, facial edema, peripheral edema, laryngismus, vesiculobullous rash) have been reported rarely with niacin therapy.
Metabolic Effects
Decreased glucose tolerance has been reported in patients receiving niacin in controlled clinical trials. In one study in patients with type 2 diabetes mellitus, antilipemic therapy with niacin (1.5 g 3 times daily) for 8 weeks resulted in a mean increase in blood glucose concentrations of 16% and glycosylated hemoglobin concentrations of 21%, and the induction of marked glycosuria in some patients. However, it has been suggested that such increases in blood glucose concentrations may reflect short-term effects from rapid institution of antilipemic dosages of niacin.
Data from a randomized, placebo-controlled study in diabetic patients receiving immediate-release niacin (3 g daily) for 60 weeks indicated no appreciable alterations in glycosylated hemoglobin concentrations and only modest increases in blood glucose concentrations that were not associated with substantially increased rates of niacin discontinuance or alterations in antidiabetic therapy. Similar findings were reported in a limited number of diabetic patients receiving extended-release niacin (Niaspan), with less than 15% of those receiving the highest dose (1500 mg daily) requiring alterations in their antidiabetic therapy. Some clinicians state that niacin should only be used in diabetic patients not responding adequately to first-line therapy (i.e., statins) or in whom other antilipemic therapy is contraindicated or not tolerated. If used in diabetic or potentially diabetic patients, blood glucose concentrations should be monitored periodically, especially early in the course of therapy, and dosages of niacin and/or antidiabetic agents should be adjusted appropriately.
Hyperuricemia and gout also have been reported in patients receiving niacin in controlled clinical studies.
Reductions in phosphorus concentrations have been reported in patients receiving niacin.
Nervous System Effects
Headache is the most common adverse nervous system effect of niacin, occurring in about 4–11% of patients in controlled studies. Asthenia, dizziness, fatigue, insomnia, leg cramps, migraine, myasthenia, nervousness, and paresthesia also have been reported with niacin therapy.
Other Adverse Effects
Other adverse effects of niacin include toxic amblyopia, blurred vision, dry eyes, dyspnea, proptosis, loss of central vision secondary to an atypical form of cystoid macular edema, pain, rhinitis, decreased platelet count, increased prothrombin time (PT), impotence, and increased amylase concentrations.
Precautions and Contraindications
Prior to institution of niacin therapy, a vigorous attempt should be made to control serum cholesterol by appropriate dietary regimens, weight reduction, and the treatment of any underlying disorder that might be the cause of the lipid abnormality. Serum cholesterol and triglyceride concentrations should be determined prior to and regularly (e.g., every 3–6 months) during niacin therapy. Serum cholesterol and triglyceride concentrations usually decrease within the first 2 weeks of niacin administration, and treatment should be continued as long as serum cholesterol and triglyceride concentrations remain below baseline concentrations. When niacin is discontinued, serum lipids generally return to pretreatment concentrations within 2–6 weeks. If no appreciable cholesterol- or triglyceride-lowering effect occurs after 1–2 months of therapy, the drug should be discontinued.
Different formulations (immediate-release, extended-release) of niacin should not be used interchangeably; severe hepatic toxicity (e.g., fulminant hepatic necrosis) has occurred in individuals who substituted certain sustained-release niacin preparations for immediate-release niacin at equivalent dosages. Niacin preparations available as dietary supplements are not labeled by FDA for the prevention of cardiovascular events or management of dyslipidemias. Such dietary supplements may contain widely varying amounts of niacin, and the American Heart Association (AHA) states that dietary supplement niacin preparations should not be used for cholesterol lowering or as substitutes for prescription-only niacin preparations because of the potential for serious adverse effects.
Liver function tests should be performed before initiation of niacin therapy, every 6–12 weeks during the first year of therapy, and periodically thereafter (e.g., semiannually). Patients who develop increased serum aminotransferase concentrations should have the liver function test repeated to confirm the results and should receive frequent liver function tests thereafter until the abnormalities return to normal. If increases in serum aminotransferase (AST or ALT) concentrations of 2–3 times the upper limit of normal or higher occur or persist, or if these elevations are associated with manifestations of nausea, fever, and/or malaise, niacin therapy should be discontinued. Liver biopsy should be considered if elevations persist after discontinuance of the drug. Niacin should be used with caution in patients who consume substantial amounts of alcohol and/or have a history of liver disease; such patients should be closely monitored. Niacin is contraindicated in patients with active liver disease or unexplained, persistent increases in liver function tests.
Rhabdomyolysis has been reported rarely in patients receiving niacin concomitantly with statins. Patients receiving niacin therapy, alone or in fixed combination with lovastatin, should be carefully monitored for signs and symptoms of muscle pain, tenderness, or weakness, especially early in the course of therapy or during upward titration of either drug. The manufacturers state that periodic monitoring of serum CK (CPK) and potassium concentrations should be considered in patients exhibiting such symptoms; however, there is no assurance that such monitoring will prevent the occurrence of severe myopathy.
Decreased glucose tolerance has been reported in patients receiving niacin in controlled clinical trials. Therefore, the manufacturers and many clinicians suggest that patients with (or those at risk of developing) diabetes mellitus be observed closely. If niacin is used in diabetic or potentially diabetic patients, dosages of niacin and/or antidiabetic agents should be adjusted appropriately.
Niacin should be used with caution in patients with unstable angina, acute myocardial infarction (MI), or coronary heart disease (CHD), particularly when these patients also are receiving vasoactive drugs such as nitrates, calcium-channel blockers, or adrenergic blocking agents. Since niacin therapy has been associated with small, but statistically significant, increases in prothrombin time (PT), the drug should be used with caution in patients undergoing surgery. PT and platelet count should be monitored closely in patients receiving niacin concomitantly with anticoagulants.
Because hyperuricemia has been reported with niacin therapy, the drug should be used with caution in patients predisposed to gout.
Use of niacin has been associated with reductions in phosphorus concentrations; therefore, phosphorus concentrations should be monitored periodically in patients at risk for developing hypophosphatemia.
Since data in patients with renal or hepatic impairment currently are lacking, the manufacturers state that niacin should be used with caution in these patients.
Niacin is contraindicated in patients with hypersensitivity to any component of the drug formulations. The drug also is contraindicated in patients with active liver disease or unexplained persistent elevations of serum transaminases, active peptic ulcer disease, or arterial bleeding.
Pediatric Precautions
Safety and efficacy of large dosages of niacin in children younger than 16 years of age have not been established. The manufacturers state that safety and efficacy of extended-release niacin (Niaspan) have not been evaluated in pediatric patients.
A National Heart, Lung, and Blood Institute (NHLBI)-appointed expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents states that antilipemic drug therapy in children should be individualized. The expert panel suggests that niacin therapy may be used in children and adolescents only in consultation with a specialist in the treatment of dyslipidemia.
Geriatric Precautions
In clinical trials of extended-release niacin (Niaspan) involving 979 patients, approximately 21% of the patients were 65 years of age or older. Although no overall differences in safety or efficacy were observed between geriatric and younger patients, and other clinical experience has not revealed evidence of age-related differences, the possibility that some geriatric patients may exhibit increased sensitivity to the drug cannot be ruled out.
Mutagenicity and Carcinogenicity
Niacin did not exhibit mutagenic potential in the Ames test. Niacin administered to mice for a lifetime as a 1% solution in drinking water was not carcinogenic. The mice in this study received approximately 6–8 times the human dose of 3 g daily as determined on a mg/m2 basis. No mutagenicity or carcinogenicity studies have been conducted with extended-release niacin (Niaspan).
Pregnancy, Fertility, and Lactation
Pregnancy
Animal reproduction studies have not been performed with niacin, and it is also not known whether the drug (at antilipemic dosages) can cause fetal harm or affect reproduction capacity when administered to pregnant women. Niacin should not be used in women who are or may become pregnant or in nursing women unless the possible benefits outweigh the potential risks. Currently, most experts recommend that hyperlipoproteinemias in pregnant women be managed with dietary measures; consultation with a lipid specialist may be indicated for pregnant women with severe forms of hyperlipidemia. If the patient becomes pregnant while receiving niacin for primary hypercholesterolemia, the drug should be discontinued. If the patient being treated with niacin for hypertriglyceridemia or mixed dyslipidemia becomes pregnant, the benefits and risks of continued therapy should be assessed on an individual basis.
Fertility
No studies on impairment of fertility have been conducted to date with niacin.
Lactation
Niacin is distributed in human milk. Because of the potential for serious adverse effects in nursing infants, a decision should be made whether to discontinue nursing or the drug, taking into account the importance of the drug to the woman.
Drug Interactions
HMG-CoA Reductase Inhibitors (Statins)
The risk of developing myopathy and rhabdomyolysis is increased in patients receiving niacin (particularly at antilipemic dosages [exceeding 1 g daily]) concomitantly with statins. Other severe adverse effects, including disturbances in glycemic control requiring hospitalization, development of diabetes mellitus, adverse GI effects, myopathy, gout, rash, skin ulceration, infection, and bleeding, have been reported in patients receiving extended-release niacin with statin therapy. Therefore, the potential benefits (e.g., further alterations in lipid concentrations) of concomitant use of antilipemic dosages of niacin with statins should be weighed carefully against the possible risks of severe adverse effects, and caution is advised if such concomitant therapy is employed.
Cases of myopathy and rhabdomyolysis have been reported with concomitant use of simvastatin and niacin dosages of 1 g or greater daily, and the risk is greater in Chinese patients. Therefore, concomitant use of simvastatin and niacin dosages of 1 g or greater daily is not recommended in Chinese patients.
Bile Acid Sequestrants
Limited data indicate that cholestyramine or colestipol resin may decrease the bioavailability of niacin, as 10–30 or 98% of the dose of niacin binds to cholestyramine or colestipol, respectively, following concomitant administration. Therefore, some manufacturers recommend that cholestyramine or colestipol and niacin be administered at least 4–6 hours apart.
Coumarin Anticoagulants
Increased prothrombin time (PT) and decreased platelet count have been reported in patients receiving niacin. Therefore, niacin should be used with caution in patients receiving concomitant anticoagulant therapy; PT and platelet count should be monitored closely in such patients.
Other Drugs
Niacin reportedly potentiates the hypotensive effects of ganglionic blocking and vasoactive drugs, resulting in postural hypotension.
Concomitant use of aspirin may decrease the metabolic clearance of niacin; the clinical relevance of this interaction has not been fully elucidated.
Vitamins or other nutritional supplements containing large doses of niacin or related compounds (i.e., nicotinamide) also may potentiate the adverse effects of niacin.
Laboratory Test Interferences
Niacin may produce fluorescent substances in the urine which cause false elevations in some fluorometric determinations of urinary catecholamines. Niacin may also give false-positive reactions with cupric sulfate solution (Benedict’s reagent) for urine glucose determination.
Acute Toxicity
Limited information is available on the acute toxicity of niacin. If acute niacin overdosage occurs, supportive and symptomatic treatment should be initiated and the patient observed closely.
Pharmacology
Antilipemic Effects
The antilipemic effect of niacin results principally from reductions in LDL- and very-low-density (VLDL)-cholesterol concentrations. In daily doses of 1 g or greater, niacin decreases serum total-cholesterol, LDL-cholesterol, VLDL-cholesterol, and triglyceride concentrations, and increases serum HDL concentrations in healthy individuals and in patients with type II, III, IV, or V hyperlipoproteinemia. Niacin also has been shown to reduce serum concentrations of apolipoprotein B (apo B), lipoprotein (a) (Lp[a]), and phospholipids, and to increase concentrations of apolipoprotein A-I (apo AI) in these patients. Effects of niacin on cardiovascular morbidity and mortality in patients without documented coronary heart disease (CHD) have not been fully elucidated.
The exact mechanism by which niacin decreases serum cholesterol and triglyceride concentrations is unknown but is independent of the drug’s role as a vitamin. The principal antilipemic effect of niacin appears to result mainly from decreased production of VLDL-cholesterol. Decreased production of VLDL-cholesterol by niacin may be related to the partial inhibition of free fatty acid release from adipose tissue, a decreased delivery of free fatty acids to the liver, and a decrease in triglyceride synthesis and VLDL-triglyceride transport. Enhanced clearance of VLDL-cholesterol and chylomicron triglycerides also may occur, possibly as a result of enhanced activity of lipoprotein lipase. Reductions in LDL-cholesterol concentrations may be related to decreased production and enhanced hepatic clearance of LDL-cholesterol precursors (i.e., VLDL-cholesterol). The mechanism by which niacin increases HDL-cholesterol concentrations has not been fully elucidated but may be related to a decreased hepatic clearance of apo A-I-containing particles and decreased synthesis of apo A-II. Niacin has no effect on cholesterol synthesis or fecal excretion of fats, sterols, or bile acids.
Antilipemic response to niacin may be related to the severity and type of underlying lipid abnormality. In daily doses of 3–6 g, the drug has been shown to decrease serum total and LDL-cholesterol concentrations by 10–20%, triglyceride concentrations by 20–80%, and to increase HDL-cholesterol concentrations by 20–35%. Effects on HDL-cholesterol concentrations appear to be variable, with more pronounced increases being reported in patients with relatively normal compared with low (i.e., less than 30 mg/dL) baseline HDL-cholesterol concentrations. Dose-related reductions in Lp(a) concentrations (e.g., 3–36%) also have been observed in patients receiving niacin therapy.
Reductions in triglyceride concentrations are apparent within 1–4 days after initiating niacin therapy, although a much longer duration (approximately 3–5 weeks) is required to achieve similar reductions in LDL-cholesterol concentrations. Refractoriness to the antilipemic effect of large doses of niacin has been reported.
Antiatherogenic Effects
Some investigators have reported regression or disappearance of xanthomata, including xanthelasma, following long-term therapy with niacin.
Other Effects
Niacin is also a vitamin and in large doses produces peripheral vasodilation. However, at usual antilipemic dosages, niacin-induced vasodilation generally is limited to cutaneous vessels. Cutaneous vasodilation induced by the drug appears to be mediated by prostaglandins (e.g., prostacyclin, prostaglandin D2). Niacin reportedly releases histamine, causing an increase in gastric motility and acid secretion; the drug also activates the fibrinolytic system. Large doses of niacin have been reported to decrease uric acid excretion and to impair glucose tolerance.
Niacin (Antilipemic) Pharmacokinetics
Information on the pharmacokinetics of niacin is limited. Because the pharmacokinetics and, therefore, metabolism of different formulations (i.e., immediate-release, extended-release) of niacin may vary, the manufacturers state that these preparations should not be used interchangeably.
Absorption
Niacin is rapidly and extensively (60–76% of dose) absorbed following oral administration. Peak plasma concentrations of niacin following administration of an immediate-release (Niacor) or extended-release (Niaspan) niacin preparation generally are attained within 30–60 minutes or 4–5 hours after oral administration, respectively.
Peak plasma concentrations of niacin and metabolites following oral administration of Niaspan extended-release tablets appear to be slightly higher in women than in men, possibly because of differences in metabolism. Limited data suggest that women may exhibit greater antilipemic response to niacin than men, possibly because of gender-specific differences in the metabolic rate or volume of distribution of the drug.
Distribution
Niacin is distributed mainly to the liver, kidney, and adipose tissue. The drug also has been shown to distribute into milk in humans.
Elimination
Niacin is rapidly metabolized and undergoes extensive first-pass metabolism. The drug is converted to several metabolites, including nicotinuric acid (NUA), nicotinamide, and nicotinamide adenine dinucleotide (NAD). At doses used to treat hyperlipoproteinemia, the principal metabolic pathways appear to be saturable, and niacin is thought to exhibit nonlinear, dose-dependent pharmacokinetics. Nicotinamide does not appear to exert antilipemic effects; the activity of other metabolites on lipoprotein fractions currently are unknown. The plasma half-life of niacin has been reported to range from 20–60 minutes.
Niacin and its metabolites are rapidly excreted in urine. Following oral administration of single and multiple doses of an immediate-release (Niacor) or extended-release (Niaspan) niacin preparation, approximately 88 or 60–76% of the dose, respectively, was excreted in urine as unchanged drug and inactive metabolites.
Chemistry and Stability
Chemistry
Niacin (nicotinic acid) is an antilipemic agent. Niacin is commercially available as conventional (immediate-release) and extended-release preparations. Niacin also is available as a dietary supplement; these preparations are not FDA-labeled for management of dyslipidemias and should not be used as substitutes for prescription-only niacin preparations. Niacin occurs as white crystals or crystalline powder with an acidic taste and is sparingly soluble in water, having an aqueous solubility of 16.7 mg/mL; the drug is freely soluble in boiling water and in boiling alcohol. Niacin has a pKa of 4.85.
Stability
Niacin should be stored in well-closed, light-resistant containers at 20–25°C. When stored under these conditions, Niaspan extended-release and Niacor immediate-release tablets are stable for 3 and 2 years, respectively, after the date of manufacture.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, extended-release |
250 mg* |
Niacin Extended-release Capsules |
|
|
500 mg* |
Niacin Extended-release Capsules |
|||
|
Tablets |
500 mg |
Niacor (scored) |
Avondale |
|
|
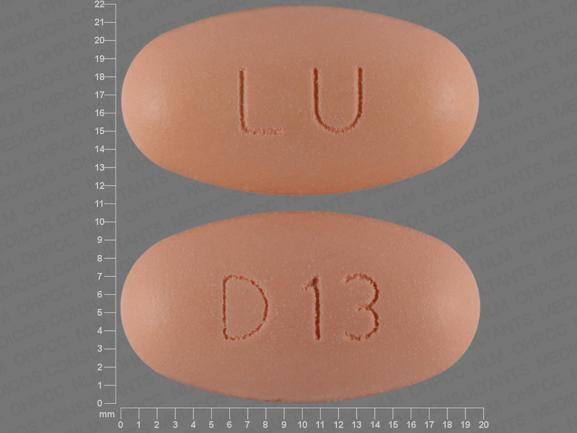
Tablets, extended-release |
250 mg |
Slo-Niacin |
Mainpointe |
|
|
500 mg* |
Niacin Extended-release Tablets |
|||
|
Slo-Niacin |
Mainpointe |
|||
|
Niaspan |
AbbVie |
|||
|
750 mg* |
Niacin Extended-release Tablets |
|||
|
Slo-Niacin |
Mainpointe |
|||
|
Niaspan |
AbbVie |
|||
|
1000 mg* |
Niacin Extended-release Tablets |
|||
|
Niaspan |
AbbVie |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about niacin
- Check interactions
- Compare alternatives
- Reviews (118)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: miscellaneous antihyperlipidemic agents