Minoxidil (Monograph)
Drug class: Direct Vasodilators
Warning
-
Risk of developing potentially serious cardiac effects.110 b (See Cardiovascular Effects under Cautions.) Pericardial effusion, progressing to tamponade may occur and angina pectoris may be exacerbated.110 b Reserve for hypertensive patients who do not respond to maximum therapeutic doses of a diuretic and 2 other antihypertensive agents.110 b
-
In animal studies, minoxidil caused myocardial lesions and other adverse cardiac effects.110 b
-
Administer under close supervision, usually concomitantly with a β-adrenergic blocking agent (β-blocker) and a diuretic, usually a loop diuretic, to prevent adverse effects.110 b
-
Hospitalize and monitor patients with malignant hypertension or those already receiving concomitant guanethidine therapy to prevent too rapid or severe orthostatic decreases in BP.110 b
Introduction
Vasodilating agent.b
Uses for Minoxidil
Hypertension
Management of severe symptomatic hypertension or hypertension associated with end-organ damage in patients with uncontrolled hypertension not manageable with maximal therapeutic dosages of a diuretic and 2 other antihypertensive agents.110 b
Not recommended for mild or moderate hypertension or severe hypertension controllable with other drugs.110 143 b
Not for initial management of hypertension according to current guidelines for the management of hypertension in adults, but may be used as add-on therapy if BP not adequately controlled with the recommended antihypertensive drug classes (i.e., ACE inhibitors, angiotensin II receptor antagonists, calcium-channel blockers, thiazide diuretics).501 502 503 504 1200
May be used in combination with other antihypertensive therapies (e.g., a diuretic and a β-blocker, an ACE inhibitor, a calcium-channel blocking agent, and/or an angiotensin II receptor antagonist).110 504 1200 b
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).501 502 503 504 515 1200 1201
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension.1200 (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP.1200 However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.501 503 504 505 506 507 508 515 523 526 530 1200 1201 1207 1209 1222 1223 1229
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk.1200 In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg.1200 These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.1200 1202 1210
Other hypertension guidelines generally have based target BP goals on age and comorbidities.501 504 536 Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk, and have used higher BP thresholds and target BPs in elderly patients501 504 536 compared with those recommended by the 2017 ACC/AHA hypertension guideline.1200
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.1222 1223 1224 1229
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.1200 1220
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors.1200 1207 ASCVD risk assessment is recommended by ACC/AHA for all adults with hypertension.1200
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).1200
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.1200
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg.1200 Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.502 1200
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP.1200 Consider initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.1200
Androgenetic Alopecia
Used topically to stimulate regrowth of hair in patients with androgenetic alopecia106 107 108 109 116 117 118 119 122 123 124 128 129 130 131 132 133 134 135 137 b (male pattern alopecia, hereditary alopecia, common male baldness) or alopecia areata†.102 103 104 105 106 107 116 117 118 125 126 127 b Safety and efficacy of extemporaneously prepared formulations of topical minoxidil in promoting hair growth not fully evaluated and such preparations may vary in strength and efficacy.110 b FDA requests that physicians and pharmacists refrain from preparing extemporaneous topical formulations using the commercially available tablets.113
Minoxidil Dosage and Administration
General
-
A β-blocker (equivalent to 80–160 mg of propranolol daily) must be given before initiation of minoxidil therapy and continued for duration of therapy, to minimize minoxidil-induced tachycardia and increased myocardial workload.110 b If a β-blocker is contraindicated, methyldopa (250–750 mg twice daily) should be initiated at least 24 hours prior to minoxidil therapy; clonidine (0.1–0.2 mg twice daily) may be used as an alternative.110 b
-
May cause sodium and water retention; a thiazide or loop diuretic must be used in patients dependent on renal function for maintenance of sodium and water balance.110 b
BP Monitoring and Treatment Goals
-
Monitor BP regularly during therapy and adjust dosage of the antihypertensive drug until BP controlled.1200 (See Patient Monitoring under Cautions.)
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.1200 1216
Administration
Oral Administration
Administer orally once daily if patient’s supine DBP has been reduced by <30 mm Hg; administer twice daily (in equally divided doses) if patient’s supine DBP reduced >30 mm Hg.110 b
If rapid control needed, may give dose every 6 hours; monitor BP closely.110 b
Dosage
Pediatric Patients
Hypertension
Oral
Children <12 years of age: Initially, 0.2 mg/kg once daily.b 600 May increase dosage at intervals of at least 3 days in increments of 50–100% until optimum BP response is achieved.600 b If rapid BP control needed, adjust dosage every 6 hours; monitor BP closely.600 b Usual effective dosage is 0.25–1 mg/kg (maximum 50 mg) daily.600 b
Children >12 years of age: Initially, 5 mg once daily.600 May increase dosage at intervals of least 3 days to 10 mg, 20 mg, and then 40 mg daily in 1 or 2 divided doses until optimum BP response is achieved.600 b If rapid BP control needed, adjust dosage every 6 hours; monitor BP closely.600 b Usual effective dosage is 10–40 mg (maximum 100 mg) daily.600 b
Severe Hypertension with Non-Life-threatening Symptoms† [off-label]
Oral
For rapid reduction of blood pressure, 0.1–0.2 mg/kg (up to 10 mg per dose) may be used;1150 b administer every 8–12 hours.1150
Adults
Hypertension
Oral
Initially, 5 mg once daily.600 b Dosages may be increased at intervals of least 3 daysb to 10 mg, 20 mg, and then 40 mg daily in 1 or 2 divided doses until optimum BP response is achieved.600 b If rapid control needed, adjust dosage every 6 hours; monitor BP closely.600 b
Usual effective dosage is 10–40 mg daily up to maximum dosage of 100 mg daily.600 b
Some experts state usual dosage range is 5–100 mg daily given as a single dose or in 2–3 divided doses.1200
Prescribing Limits
Pediatric Patients
Hypertension
Oral
Children <12 years of age: maximum 50 mg daily.600 b
Children >12 years of age: maximum 100 mg daily.600 b
Adults
Hypertension
Oral
Special Populations
Renal Impairment
Lower dosage may be required in renal failure or dialysis (about one-third less than in patients who are not receiving dialysis).110 b
Removed during dialysis.b Some clinicians recommend administering minoxidil immediately after dialysis (if dialysis is at 9 a.m.); if dialysis is after 3 p.m., the daily dose is given at 7 a.m. (i.e., 8 hours before dialysis). b
Geriatric Patients
Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.110 b
Cautions for Minoxidil
Contraindications
Warnings/Precautions
Warnings
Cardiovascular Effects
Sodium and water retention occur frequently; may result in edema, weight gain, CHF, pulmonary edema, and refractoriness to the antihypertensive effects of minoxidil.110 b Concomitant administration of a diuretic (usually a loop diuretic) generally required.110 b (See General under Dosage and Administration.) Ascites also reported.110 b
Tachycardia occurs commonly and angina pectoris may worsen or occur without previous angina; these effects may be minimized by concomitant administration of a β-adrenergic blocking agent.110 b (See General under Dosage and Administration.)
Pericarditis and pericardial effusion (occasionally with tamponade) reported mainly in patients with connective tissue disease, uremic syndrome, CHF, or marked fluid retention; idiopathic cases also reported.110 b Observe patients closely.110 b (See Boxed Warning.)
Rapid or excessive BP reductions in patients with severe BP elevation may precipitate syncope, cerebrovascular accidents, MI, and ischemia of special sense organs resulting in decrease or loss of vision or hearing;110 b hospitalize patients with malignant hypertension and those already receiving guanethidine (see Specific Drugs under Interactions) during initial minoxidil therapy and monitor closely to assure that BP is decreasing but not too rapidly.110 b
Use with caution in patients with recent MI (within previous month); decreased arterial BP may further limit myocardial blood flow.110 b
Sensitivity Reactions
Possible hypersensitivity (skin rash); may consider discontinuance depending on alternative therapies.110 b
General Precautions
Patient Monitoring
Monitor fluid and electrolyte balance and body weight.110 b Closely supervise patients with renal failure or those undergoing dialysis to prevent exacerbation of renal failure or precipitation of cardiac failure.110 b Observe patients for signs and symptoms of pericardial effusion.110 b
Repeat any abnormal laboratory test (e.g., urinalysis, renal function, ECG, chest radiograph, echocardiogram) occurring at initiation of therapy, initially at 1- to 3-month intervals and as stabilization occurs, at 6- to 12-month intervals.110
Specific Populations
Pregnancy
Category C.110
Lactation
Distributed into milk. 110 b Use not recommended by manufacturers.110
Pediatric Use
Clinical experience with minoxidil for management of hypertension in children, especially infants, is limited.110 b Careful titration of dosage required.110 b
Geriatric Use
Insufficient experience in patients ≥ 65 years of age to determine whether geriatric patients respond differently than younger adults.110 b
Select dosage with caution because of greater frequency of hepatic, renal, and/or cardiac function and of concomitant disease and drug therapy in the elderly.110 b (See Geriatric Patients under Dosage and Administration.)
Common Adverse Effects
Hypertrichosis,110 salt and water retention,110 b pericardial effusion,110 b nausea, 110 b vomiting. 110
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Diuretics |
Additive hypotensive effect;b concomitant use may prevent sodium retention and increased plasma volume that may occur with minoxidil therapy110 b |
Usually used to therapeutic advantage; adjust dosage carefully and monitor for excessive BP reduction110 b |
|
Guanethidine |
Withdraw guanethidine110 b 1–3 weeks prior to initiating minoxidil therapy;b if not possible, initiate minoxidil in hospital setting and monitor until orthostasis no longer present110 b |
|
|
Hypotensive agents |
Additive hypotensive effect;b concomitant use may prevent sodium retention and increased plasma volume that may occur with minoxidil therapy110 b |
Usually used to therapeutic advantage; adjust dosage carefully and monitor for excessive BP reduction110 b |
Minoxidil Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration; at least 90% of an oral dose is absorbed.110 Peak plasma concentrations of unchanged drug usually attained within 1 hour.110 b
Onset
Following oral administration, antihypertensive effect occurs within 30 minutes and is maximum in 2–8 hours.110 b
Duration
Distribution
Extent
Readily distributed into body tissues.b
Plasma Protein Binding
Does not bind to plasma proteins.110 b
Elimination
Metabolism
Approximately 90% of an oral dose is metabolized to less active metabolites than parent drug, principally by conjugation with glucuronic acid and by conversion to more polar metabolites.110 b
Elimination Route
Excreted principally in urine by glomerular filtration.110 b
Half-life
Special Populations
Clearance is directly affected by GFR.110
Stability
Storage
Oral
Tablets
Actions
-
Reduces peripheral vascular resistance and BP through direct vasodilation of vascular smooth muscle.110 b
-
Reduces BP in both supine and standing patients; does not produce orthostatic hypotension.b
-
Increases heart rate, cardiac output, and stroke volume.110 b
-
Causes sodium and water retention and increased plasma volume.110 b
Advice to Patients
-
Importance of informing patients about continuing all antihypertensive drug therapy and taking only as prescribed.110
-
Do not discontinue minoxidil unless instructed by a clinician.110
-
Importance of informing patients about symptoms of fluid overload and cardiac effects.110 Importance of reporting these symptoms to a clinician.110
-
Importance of providing patient a copy of manufacturer's patient information.110
-
Inform patients of the likelihood of unwanted hair growth, which may develop within 3 to 6 weeks after starting therapy and may be especially disturbing to children and women.110 Inform patients about this effect before initiating therapy.110
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as concomitant illnesses.110
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.110
-
Importance of informing patients about other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
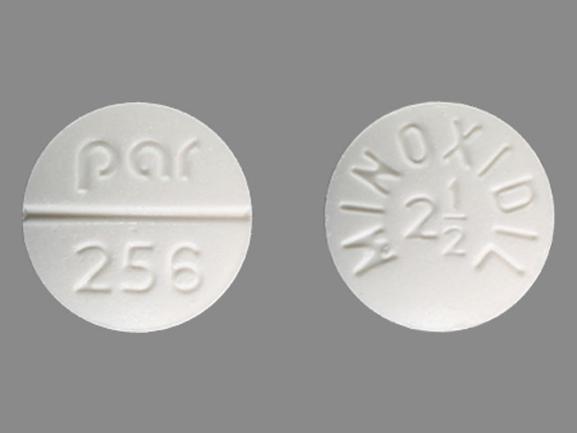
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
2.5 mg* |
Minoxidil Tablets |
|
|
10 mg* |
Minoxidil Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
Only references cited for selected revisions after 1984 are available electronically.
101. Valdivieso A, Valdés G, Spiro TE et al. Minoxidil in breast milk. Ann Intern Med. 1985; 102:135. https://pubmed.ncbi.nlm.nih.gov/3966734
102. Weiss VC, West DP, Mueller CE. Topical minoxidil in alopecia areata. J Am Acad Dermatol. 1981; 5:224-6. https://pubmed.ncbi.nlm.nih.gov/7263970
103. Fenton DA, Wilkinson JD. Topical minoxidil in the treatment of alopecia areata. BMJ. 1983; 287:1015-7. https://pubmed.ncbi.nlm.nih.gov/6412929 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1549582/
104. King CM, Harrop B, Dave VK. Topical minoxidil in the treatment of alopecia areata. BMJ. 1983; 287:1380. https://pubmed.ncbi.nlm.nih.gov/6416428 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1549503/
105. Weiss VC, West DP, Fu TS et al. Alopecia areata treated with topical minoxidil. Arch Dermatol. 1984; 120:457-63. https://pubmed.ncbi.nlm.nih.gov/6703751
106. Vanderveen EE, Ellis CN, Kang S et al. Topical minoxidil for hair regrowth. J Am Acad Dermatol. 1984; 11:416-21. https://pubmed.ncbi.nlm.nih.gov/6384289
107. Novak E, Franz TJ, Headington JT et al. Topically applied minoxidil in baldness. Int J Dermatol. 1985; 24:82-7. https://pubmed.ncbi.nlm.nih.gov/3886571
108. Vermorken AJM. Reversal of androgenic alopecia by minoxidil: lack of effect of simultaneously administered intermediate doses of cyproterone acetate. Acta Derm Venereol. 1983; 63:268-9. https://pubmed.ncbi.nlm.nih.gov/6192653
109. De Villez RL. Topical minoxidil therapy in hereditary androgenetic alopecia. Arch Dermatol. 1985; 121:197-202. https://pubmed.ncbi.nlm.nih.gov/3883902
110. Par Pharmaceutical, Inc. Minoxidil tablets prescribing information. Spring Valley, NY; 2003 Apr.
111. Weiss VC, West DP. Topical minoxidil therapy and hair regrowth. Arch Dermatol. 1985; 121:191-2. https://pubmed.ncbi.nlm.nih.gov/3977331
112. Franz TJ. Percutaneous absorption of minoxidil in man. Arch Dermatol. 1985; 121:203-6. https://pubmed.ncbi.nlm.nih.gov/3977334
113. Anon. Unapproved use of minoxidil. FDA Drug Bull. 1985; 15(4):38.
114. Kaler SG, Patrinos ME, Lambert GH et al. Hypertrichosis and congenital anomalies associated with maternal use of minoxidil. Pediatrics. 1987; 79:434-6. https://pubmed.ncbi.nlm.nih.gov/3547299
115. Rosa FW, Idanpaan-Heikkila J, Asanti R. Fetal minoxidil exposure. Pediatrics. 1987; 80:120. https://pubmed.ncbi.nlm.nih.gov/3601507
116. Anon. Topical minoxidil for baldness. Med Lett Drugs Ther. 1987; 29:87-8. https://pubmed.ncbi.nlm.nih.gov/3306300
117. Rumsfield JA, West DP, Fiedler-Weiss VC. Topical minoxidil therapy for hair regrowth. Clin Pharm. 1987; 6:386-92. https://pubmed.ncbi.nlm.nih.gov/3311578
118. Clissold SP, Heel RC. Topical minoxidil: a preliminary review of its pharmacodynamic properties and therapeutic efficacy in alopecia areata and alopecia androgenetica. Drugs. 1987; 33:107-22. https://pubmed.ncbi.nlm.nih.gov/3552591
119. de Groot AC, Nater JP, Herxheimer A. Minoxidil: hope for the bald? Lancet. 1987; 1:1019-21.
120. Mitchell AD, De Villez R. Minoxidil for male-pattern baldness. Lancet. 1987; 1:1436. https://pubmed.ncbi.nlm.nih.gov/2884528
121. de Groot AC, Nater JP, Herxheimer A. Minoxidil for male-pattern baldness. Lancet. 1987; 2:563. https://pubmed.ncbi.nlm.nih.gov/2887848
122. Koperski JA, Orenberg EK, Wilkinson DI. Topical minoxidil therapy for androgenetic alopecia: a 30-month study. Arch Dermatol. 1987; 123:1483-7. https://pubmed.ncbi.nlm.nih.gov/3314717
123. Olsen EA, Weiner MS. Topical minoxidil in male pattern baldness: effects of discontinuation of treatment. J Am Acad Dermatol. 1987; 17:97-101. https://pubmed.ncbi.nlm.nih.gov/3301926
124. Roenigk HH Jr, Pepper E, Kuruvilla S. Topical minoxidil therapy for hereditary male pattern alopecia. Cutis. 1987; 39:337-42. https://pubmed.ncbi.nlm.nih.gov/3556042
125. Fiedler-Weiss VC. Topical minoxidil solution (1% and 5%) in the treatment of alopecia areata. J Am Acad Dermatol. 1987; 16(3 Part 2):745-8. https://pubmed.ncbi.nlm.nih.gov/3549811
126. Price VH. Topical minoxidil (3%) in extensive alopecia areata, including long-term efficacy. J Am Acad Dermatol. 1987; 16(3 Part 2):737-44. https://pubmed.ncbi.nlm.nih.gov/3549810
127. Price VH. Double-blind, placebo-controlled evaluation of topical minoxidil. J Am Acad Dermatol. 1987; 16(3 Part 2):730-6. https://pubmed.ncbi.nlm.nih.gov/3549809
128. Kreindler TG. Topical minoxidil in early androgenetic alopecia. J Am Acad Dermatol. 1987; 16(3 Part 2):718-24. https://pubmed.ncbi.nlm.nih.gov/3549807
129. Katz HI, Hien NT, Prawer SE et al. Long-term efficacy of topical minoxidil in male pattern baldness. J Am Acad Dermatol. 1987; 16(3 Part 2):711-8. https://pubmed.ncbi.nlm.nih.gov/3549806
130. Roberts JL. Androgenetic alopecia: results with topical minoxidil. J Am Acad Dermatol. 1987; 16(3 Part 2):705-10. https://pubmed.ncbi.nlm.nih.gov/3549805
131. Savin RC. Use of topical minoxidil in the treatment of male-pattern baldness. J Am Acad Dermatol. 1987; 16(3 Part 2):696-704. https://pubmed.ncbi.nlm.nih.gov/3549804
132. Olsen EA, DeLong ER, Weiner MS. Long-term follow-up of men with male pattern baldness treated with topical minoxidil. J Am Acad Dermatol. 1987; 16(3 Part 2):688-85. https://pubmed.ncbi.nlm.nih.gov/3549803
133. Rietschel RL, Duncan SH. Safety and efficacy of topical minoxidil in the management of androgenetic alopecia. J Am Acad Dermatol. 1987; 16(3 Part 2):677-85. https://pubmed.ncbi.nlm.nih.gov/3549802
134. Shupack JL, Kassimir JJ, Thirumoorthy T et al. Dose-response study of topical minoxidil in male pattern alopecia. J Am Acad Dermatol. 1987; 16(3 Part 2):673-6. https://pubmed.ncbi.nlm.nih.gov/3549801
135. De Villez RL. Androgenetic alopecia treated with topical minoxidil. J Am Acad Dermatol. 1987; 16(3 Part 2):669-72. https://pubmed.ncbi.nlm.nih.gov/3549800
136. Stern RS. Topical minoxidil: a survey of use and complications. Arch Dermatol. 1987; 123:62-5. https://pubmed.ncbi.nlm.nih.gov/3800424
137. Olsen EA, Weiner MS, Delong ER et al. Topical minoxidil in early male pattern baldness. J Am Acad Dermatol. 1985; 13(2 Part 1):185-92. https://pubmed.ncbi.nlm.nih.gov/3900155
138. Franz TJ. Percutaneous absorption of minoxidil. Arch Dermatol. 1986; 122:15-6. https://pubmed.ncbi.nlm.nih.gov/3942404
139. Lustig S, Pitlik SD, Garty M et al. Pericarditis after minoxidil reinstitution. Drug Intell Clin Pharm. 1985; 19:763. https://pubmed.ncbi.nlm.nih.gov/4053985
140. Krehlik JM, Hindson DA, Crowley JJ Jr et al. Minoxidil-associated pericarditis and fatal cardiac tamponade. West J Med. 1985; 143:527-9. https://pubmed.ncbi.nlm.nih.gov/4090485 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1306401/
141. Evans CW, Tucker SC. Pericarditis: a complication of minoxidil therapy. South Med J. 1983; 76:815-6. https://pubmed.ncbi.nlm.nih.gov/6857316
143. Anon. Drugs for hypertension. Med Lett Drugs Ther. 1989; 31:25-30. https://pubmed.ncbi.nlm.nih.gov/2927361
145. National Heart, Lung, and Blood Institute National High Blood Pressure Education Program. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). Bethesda, MD: National Institutes of Health; 1997 Nov. (NIH publication No. 98-4080.)
146. Kaplan NM. Choice of initial therapy for hypertension. JAMA. 1996; 275:1577-80. https://pubmed.ncbi.nlm.nih.gov/8622249
147. Izzo JL, Levy D, Black HR. Importance of systolic blood pressure in older Americans. Hypertension. 2000; 35:1021-4. https://pubmed.ncbi.nlm.nih.gov/10818056
148. Frohlich ED. Recognition of systolic hypertension for hypertension. Hypertension. 2000; 35:1019-20. https://pubmed.ncbi.nlm.nih.gov/10818055
149. Bakris GL, Williams M, Dworkin L et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. Am J Kidney Dis. 2000; 36:646-61. https://pubmed.ncbi.nlm.nih.gov/10977801
150. Hansson L, Zanchetti A, Carruthers SG et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998; 351:1755-62. https://pubmed.ncbi.nlm.nih.gov/9635947
153. Pharmacia & Upjohn. Rogaine (minoxidil) topical solution prescribing information. In: Physicians’ desk reference. 50th ed. Montvale, NJ: Medical Economics Company. 1996; 2637- 41.
154. Appel LJ. The verdict from ALLHAT—thiazide diuretics are the preferred initial therapy for hypertension. JAMA. 2002; 288:3039-60. https://pubmed.ncbi.nlm.nih.gov/12479770
155. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002; 288:2981-97. https://pubmed.ncbi.nlm.nih.gov/12479763
157. Whelton PK, Appel LJ, Espeland MA et al. for the TONE Collaborative Research Group. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). JAMA. 1998; 279:839-46. https://pubmed.ncbi.nlm.nih.gov/9515998
159. Psaty BM, Smith NL, Siscovick DS et al. Health outcomes associated with antihypertensive therapies used as first-line agents: a systematic review and meta-analysis. JAMA. 1997; 277:739-45. https://pubmed.ncbi.nlm.nih.gov/9042847
162. The Guidelines Subcommittee of the WHO/ISH Mild Hypertension Liaison Committee. 1999 guidelines for the management of hypertension. J Hypertension. 1999; 17:392-403.
b. AHFS drug information 2015. McEvoy GK, ed. Minoxidil. Bethesda, MD: American Society of Health-System Pharmacists; 2015:.
501. James PA, Oparil S, Carter BL et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507-20. https://pubmed.ncbi.nlm.nih.gov/24352797
502. Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013; 31:1281-357. https://pubmed.ncbi.nlm.nih.gov/23817082
503. Go AS, Bauman MA, Coleman King SM et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014; 63:878-85. https://pubmed.ncbi.nlm.nih.gov/24243703
504. Weber MA, Schiffrin EL, White WB et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014; 16:14-26. https://pubmed.ncbi.nlm.nih.gov/24341872
505. Wright JT, Fine LJ, Lackland DT et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014; 160:499-503. https://pubmed.ncbi.nlm.nih.gov/24424788
506. Mitka M. Groups spar over new hypertension guidelines. JAMA. 2014; 311:663-4. https://pubmed.ncbi.nlm.nih.gov/24549531
507. Peterson ED, Gaziano JM, Greenland P. Recommendations for treating hypertension: what are the right goals and purposes?. JAMA. 2014; 311:474-6. https://pubmed.ncbi.nlm.nih.gov/24352710
508. Bauchner H, Fontanarosa PB, Golub RM. Updated guidelines for management of high blood pressure: recommendations, review, and responsibility. JAMA. 2014; 311:477-8. https://pubmed.ncbi.nlm.nih.gov/24352759
515. Thomas G, Shishehbor M, Brill D et al. New hypertension guidelines: one size fits most?. Cleve Clin J Med. 2014; 81:178-88. https://pubmed.ncbi.nlm.nih.gov/24591473
523. Fihn SD, Gardin JM, Abrams J et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012; 126:e354-471.
526. Kernan WN, Ovbiagele B, Black HR et al. Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2014; :. https://pubmed.ncbi.nlm.nih.gov/24788967
530. Myers MG, Tobe SW. A Canadian perspective on the Eighth Joint National Committee (JNC 8) hypertension guidelines. J Clin Hypertens (Greenwich). 2014; 16:246-8. https://pubmed.ncbi.nlm.nih.gov/24641124
536. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012: 2: 337-414.
600. Par Pharmaceutical, Inc. Minoxidil tablets prescribing information. Chestnut Ridge, NY; 2015 Oct.
1150. Flynn JT, Kaelber DC, Baker-Smith CM et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017; 140 https://pubmed.ncbi.nlm.nih.gov/28827377
1200. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:el13-e115. https://pubmed.ncbi.nlm.nih.gov/29133356
1201. Bakris G, Sorrentino M. Redefining hypertension - assessing the new blood-pressure guidelines. N Engl J Med. 2018; 378:497-499. https://pubmed.ncbi.nlm.nih.gov/29341841
1202. Carey RM, Whelton PK, 2017 ACC/AHA Hypertension Guideline Writing Committee. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association hypertension guideline. Ann Intern Med. 2018; 168:351-358. https://pubmed.ncbi.nlm.nih.gov/29357392
1207. Burnier M, Oparil S, Narkiewicz K et al. New 2017 American Heart Association and American College of Cardiology guideline for hypertension in the adults: major paradigm shifts, but will they help to fight against the hypertension disease burden?. Blood Press. 2018; 27:62-65. https://pubmed.ncbi.nlm.nih.gov/29447001
1209. Qaseem A, Wilt TJ, Rich R et al. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017; 166:430-437. https://pubmed.ncbi.nlm.nih.gov/28135725
1210. SPRINT Research Group, Wright JT, Williamson JD et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103-16. https://pubmed.ncbi.nlm.nih.gov/26551272
1216. Taler SJ. Initial treatment of hypertension. N Engl J Med. 2018; 378:636-644. https://pubmed.ncbi.nlm.nih.gov/29443671
1220. Cifu AS, Davis AM. Prevention, detection, evaluation, and management of high blood pressure in adults. JAMA. 2017; 318:2132-2134. https://pubmed.ncbi.nlm.nih.gov/29159416
1222. Bell KJL, Doust J, Glasziou P. Incremental benefits and harms of the 2017 American College of Cardiology/American Heart Association high blood pressure guideline. JAMA Intern Med. 2018; 178:755-7. https://pubmed.ncbi.nlm.nih.gov/29710197
1223. LeFevre M. ACC/AHA hypertension guideline: what is new? what do we do?. Am Fam Physician. 2018; 97(6):372-3. https://pubmed.ncbi.nlm.nih.gov/29671534
1224. Brett AS. New hypertension guideline is released. From NEJM Journal Watch website. Accessed 2018 Jun 18. https://www.jwatch.org/na45778/2017/12/28/nejm-journal-watch-general-medicine-year-review-2017
1229. Ioannidis JPA. Diagnosis and treatment of hypertension in the 2017 ACC/AHA guidelines and in the real world. JAMA. 2018; 319(2):115-6. https://pubmed.ncbi.nlm.nih.gov/29242891
Related/similar drugs
Frequently asked questions
- Does minoxidil really work for women’s hair loss?
- Oral vs Topical Minoxidil: Which Should You Choose?
- Can you use Finasteride and Minoxidil together safely?
- How long does minoxidil take to work?
More about minoxidil
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (10)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: vasodilators
- Breastfeeding
- En español