Levofloxacin (Monograph)
Brand name: Levaquin
Drug class: Quinolones
VA class: AM900
Chemical name: (S)-9-Fluoro-2,3-dihydro-3-methyl-10-(4-methyl-1-piperazinyl)-7-oxo-7H-pyrido[1,2,3-de]-1,4-benzoxazine-6-carboxylic acid hydrate (2:1)
Molecular formula: C18H20FN3O4•½H2O
CAS number: 138199-71-0
Warning
- Serious Adverse Effects
-
Fluoroquinolones, including levofloxacin, have been associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that have occurred together.1 Discontinue immediately and avoid use of fluoroquinolones, including levofloxacin, in patients who have experienced any of these serious adverse reactions.1 (See Warnings under Cautions.)
-
Fluoroquinolones, including levofloxacin, may exacerbate muscle weakness in patients with myasthenia gravis.1 Avoid in patients with known history of myasthenia gravis.1
-
Because of risk of serious adverse reactions, use levofloxacin for treatment of acute bacterial sinusitis, acute bacterial exacerbations of chronic bronchitis, or uncomplicated urinary tract infections (UTIs) only when no other treatment options available.1
Introduction
Antibacterial; fluoroquinolone.1 2 8 12
Uses for Levofloxacin
Respiratory Tract Infections
Treatment of acute bacterial sinusitis caused by susceptible Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis.1 2 8 18 90
Treatment of acute bacterial exacerbations of chronic bronchitis caused by susceptible Staphylococcus aureus, S. pneumoniae, H. influenzae, H. parainfluenzae, or M. catarrhalis.1 2 8 19 20
Use for treatment of acute bacterial sinusitis or acute bacterial exacerbations of chronic bronchitis only when no other treatment options available.1 2 8 140 145 Because systemic fluoroquinolones, including levofloxacin, have been associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that can occur together in the same patient (see Cautions)1 2 8 140 145 and because acute bacterial sinusitis and acute bacterial exacerbations of chronic bronchitis may be self-limiting in some patients,1 2 8 risks of serious adverse reactions outweigh benefits of fluoroquinolones for patients with these infections.140 145
Treatment of community-acquired pneumonia (CAP) caused by susceptible S. aureus, S. pneumoniae (including multidrug-resistant S. pneumoniae [MDRSP]), H. influenzae, H. parainfluenzae, Klebsiella pneumoniae, Legionella pneumoniae, M. catarrhalis, Chlamydophila pneumoniae (formerly Chlamydia pneumoniae), or Mycoplasma pneumoniae.1 2 8 21 95 512 Select regimen for empiric treatment of CAP based on most likely pathogens and local susceptibility patterns; after pathogen is identified, modify to provide more specific therapy (pathogen-directed therapy).512
Treatment of nosocomial pneumonia caused by susceptible S. aureus (oxacillin-susceptible [methicillin-susceptible] strains only), S. pneumoniae, H. influenzae, Escherichia coli, K. pneumoniae, Pseudomonas aeruginosa, or Serratia marcescens.1 2 8 Use adjunctive therapy as clinically indicated;1 2 8 if Ps. aeruginosa known or suspected to be involved, concomitant use of an antipseudomonal β-lactam recommended.1 2 8 Select regimen for empiric treatment of hospital-acquired pneumonia (HAP) not associated with mechanical ventilation or ventilator-associated pneumonia (VAP) based on local susceptibility data.315 If a fluoroquinolone used for initial empiric treatment of HAP or VAP, IDSA and ATS recommend ciprofloxacin or levofloxacin.315
Consult current IDSA clinical practice guidelines available at [Web] for additional information on management of respiratory tract infections.315 512
Skin and Skin Structure Infections
Treatment of mild to moderate uncomplicated skin and skin structure infections (including abscesses, cellulitis, furuncles, impetigo, pyoderma, wound infections) caused by susceptible S. aureus or S. pyogenes (group A β-hemolytic streptococci.1 2 8 27 543
Treatment of complicated skin and skin structure infections caused by susceptible S. aureus (oxacillin-susceptible [methicillin-susceptible] strains only), Enterococcus faecalis, S. pyogenes, or Proteus mirabilis.1 2 8 46 58
Consult current IDSA clinical practice guidelines available at [Web] for additional information on management of skin and skin structure infections.543 544
Urinary Tract Infections (UTIs) and Prostatitis
Treatment of mild to moderate uncomplicated UTIs caused by susceptible E. coli, K. pneumoniae, or S. saprophyticus.1 2 8
Use for treatment of uncomplicated UTIs only when no other treatment options available.1 2 8 140 145 Because systemic fluoroquinolones, including levofloxacin, have been associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that can occur together in the same patient(see Cautions)1 2 8 140 145 and because uncomplicated UTIs may be self-limiting in some patients,1 2 8 risks of serious adverse reactions outweigh benefits of fluoroquinolones for patients with uncomplicated UTIs.140 145
Treatment of mild to moderate complicated UTIs caused by susceptible E. faecalis, Enterobacter cloacae, E. coli, K. pneumoniae, P. mirabilis, or P. aeruginosa.1 2 8
Treatment of acute pyelonephritis caused by susceptible E. coli, including cases with concurrent bacteremia.1 2 8
Treatment of chronic prostatitis caused by susceptible E. coli, E. faecalis, or S. epidermidis.1 2 8
Endocarditis
Alternative for treatment of endocarditis† [off-label] (native or prosthetic valve or other prosthetic material) caused by fastidious gram-negative bacilli known as the HACEK group (Haemophilus, Aggregatibacter, Cardiobacterium hominis, Eikenella corrodens, Kingella).450 AHA and IDSA recommend ceftriaxone (or other third or fourth generation cephalosporin),450 but state that a fluoroquinolone (ciprofloxacin, levofloxacin, moxifloxacin) may be considered in patients who cannot tolerate cephalosporins.450 Consultation with an infectious disease specialist recommended.450
GI Infections
Alternative for treatment of campylobacteriosis† [off-label] caused by susceptible Campylobacter.440 Optimal treatment of campylobacteriosis in HIV-infected patients not identified.440 Some clinicians withhold anti-infective treatment in those with CD4+ T-cells >200 cells/mm3 and only mild campylobacteriosis and initiate treatment if symptoms persist for more than several days.440 In those with mild to moderate campylobacteriosis, treatment with a fluoroquinolone (preferably ciprofloxacin or, alternatively, levofloxacin or moxifloxacin) or azithromycin is reasonable.440 Modify anti-infective therapy based on results of in vitro susceptibility testing;440 resistance to fluoroquinolones reported in 22% of C. jejuni and 35% of C. coli isolates tested in US.440
Treatment of Salmonella gastroenteritis† [off-label].440 CDC, NIH, and HIV Medicine Association of IDSA recommend ciprofloxacin as initial drug of choice for treatment of Salmonella gastroenteritis (with or without bacteremia) in HIV-infected adults;440 other fluoroquinolones (levofloxacin, moxifloxacin) also likely to be effective, but data limited.440 Depending on in vitro susceptibility, alternatives are co-trimoxazole and third generation cephalosporins (ceftriaxone, cefotaxime).440 Role of long-term anti-infective treatment (secondary prophylaxis) against Salmonella in HIV-infected individuals with recurrent bacteremia not well established;440 weigh benefits of such prophylaxis against risks of long-term anti-infective therapy.440
Treatment of shigellosis† [off-label] caused by susceptible Shigella.440 Anti-infectives may not be required for mild infections, but generally indicated in addition to fluid and electrolyte replacement for treatment of patients with severe shigellosis, dysentery, or underlying immunosuppression.292 440 Empiric treatment regimen can be used initially, but in vitro susceptibility testing indicated since resistance is common.292 Fluoroquinolones (preferably ciprofloxacin or, alternatively, levofloxacin or moxifloxacin) have been recommended for treatment of shigellosis in HIV-infected adults, but consider that fluoroquinolone-resistant Shigella reported in the US, especially in international travelers, the homeless, and men who have sex with men (MSM).440 Depending on in vitro susceptibility, other drugs recommended for treatment of shigellosis include co-trimoxazole, ceftriaxone, azithromycin (not recommended in those with bacteremia), or ampicillin.197 292 440
Treatment of travelers’ diarrhea† [off-label].305 525 If caused by bacteria, may be self-limited and often resolves within 3–7 days without anti-infective treatment.305 525 CDC states anti-infective treatment not recommended for mild travelers' diarrhea;525 CDC and others state empiric short-term anti-infective treatment (single dose or up to 3 days) may be used if diarrhea is moderate or severe, associated with fever or bloody stools, or extremely disruptive to travel plans.305 525 Fluoroquinolones (ciprofloxacin, levofloxacin) generally have been considered drugs of choice for empiric treatment, including self-treatment;305 525 alternatives include azithromycin and rifaximin.305 525 Consider that increasing incidence of enteric bacteria resistant to fluoroquinolones and other anti-infectives may limit usefulness of empiric treatment in individuals traveling in certain geographic areas;525 also consider possible adverse effects of the anti-infective and adverse consequences of such treatment (e.g., development of resistance, effect on normal gut microflora).525
Prevention of travelers’ diarrhea† in individuals traveling for relatively short periods to areas of risk.305 525 CDC and others do not recommend anti-infective prophylaxis in most travelers.525 May consider prophylaxis in short-term travelers who are high-risk individuals (e.g., HIV-infected or other immunocompromised individuals, travelers with poorly controlled diabetes mellitus or chronic renal failure) and those taking critical trips during which even a short episode of diarrhea could adversely affect purpose of trip.305 525 If anti-infective prophylaxis used, fluoroquinolones (ciprofloxacin, levofloxacin) usually have been recommended;305 525 alternatives include azithromycin and rifaximin.305 525 Weigh use of anti-infective prophylaxis against use of prompt, early self-treatment with an empiric anti-infective if moderate to severe travelers' diarrhea occurs.525 Also consider increasing incidence of fluoroquinolone resistance in pathogens that cause travelers’ diarrhea (e.g., Campylobacter, Salmonella, Shigella).305 525
Has been used as a component of various multiple-drug regimens for treatment of infections caused by Helicobacter pylori†.235 236 237 Data are limited regarding prevalence of fluoroquinolone-resistant H. pylori in the US; possible impact of such resistance on efficacy of fluoroquinolone-containing regimens used for treatment of H. pylori infections not known.235
Anthrax
Inhalational anthrax (postexposure) to reduce incidence or progression of disease following suspected or confirmed exposure to aerosolized Bacillus anthracis spores.1 2 8 CDC, AAP, US Working Group on Civilian Biodefense, and US Army Medical Research Institute of Infectious Diseases (USAMRIID) recommend oral ciprofloxacin and oral doxycycline as initial drugs of choice for prophylaxis following such exposures, including exposures that occur in the context of biologic warfare or bioterrorism.668 671 672 673 683 686 Other oral fluoroquinolones (levofloxacin, moxifloxacin, ofloxacin) are alternatives for postexposure prophylaxis when ciprofloxacin or doxycycline cannot be used.668 671 672 673
Treatment of uncomplicated cutaneous anthrax† (without systemic involvement) that occurs in the context of biologic warfare or bioterrorism.671 672 673 CDC states that preferred drugs for such infections include oral ciprofloxacin, doxycycline, levofloxacin, or moxifloxacin.672 673
Alternative to ciprofloxacin for use in multiple-drug parenteral regimens for initial treatment of systemic anthrax† (inhalational, GI, meningitis, or cutaneous with systemic involvement, head or neck lesions, or extensive edema) that occurs in the context of biologic warfare or bioterrorism.668 671 672 673 For initial treatment of systemic anthrax with possible or confirmed meningitis, CDC and AAP recommend a regimen of IV ciprofloxacin in conjunction with another IV bactericidal anti-infective (preferably meropenem) and an IV protein synthesis inhibitor (preferably linezolid).671 672 673 If meningitis excluded, these experts recommend an initial regimen of IV ciprofloxacin in conjunction with an IV protein synthesis inhibitor (preferably clindamycin or linezolid).671 672 673
Has been suggested as possible alternative to ciprofloxacin for treatment of inhalational anthrax† when a parenteral regimen not available (e.g., supply or logistic problems because large numbers of individuals require treatment in a mass-casualty setting).668
Chlamydial Infections
Alternative for treatment of urogenital infections caused by Chlamydia trachomatis†.344 CDC recommends azithromycin or doxycycline;344 alternatives are erythromycin, levofloxacin, or ofloxacin.344
Gonorrhea and Associated Infections
Was used in the past for treatment of uncomplicated gonorrhea† caused by susceptible Neisseria gonorrhoeae.114
Because quinolone-resistant N. gonorrhoeae (QRNG) widely disseminated worldwide, including in the US,344 857 CDC states fluoroquinolones no longer recommended for treatment of gonorrhea and should not be used routinely for any associated infections that may involve N. gonorrhoeae (e.g., pelvic inflammatory disease [PID], epididymitis).344
Alternative for treatment of PID†.344 (See Pelvic Inflammatory Disease under Uses.)
Alternative for treatment of acute epididymitis†.344 CDC recommends a single IM dose of ceftriaxone in conjunction with oral doxycycline for acute epididymitis most likely caused by sexually transmitted chlamydia and gonorrhea or a single IM dose of ceftriaxone in conjunction with oral levofloxacin or ofloxacin for treatment of acute epididymitis most likely caused by sexually transmitted chlamydia and gonorrhea and enteric bacteria (e.g., in men who practice insertive anal sex).344 Levofloxacin or ofloxacin can be used alone if acute epididymitis most likely caused by enteric bacteria (e.g., in men who have undergone prostate biopsy, vasectomy, or other urinary tract instrumentation procedure) and gonorrhea ruled out (e.g., by gram, methylene blue, or gentian violet stain).344
Tuberculosis
Alternative (second-line) agent for use in multiple-drug regimens for treatment of active tuberculosis† caused by Mycobacterium tuberculosis.218 231 276 440
Although potential role of fluoroquinolones and optimal length of therapy not fully defined, ATS, CDC, IDSA, and others state that use of fluoroquinolones as alternative (second-line) agents can be considered for treatment of active tuberculosis in patients intolerant to certain first-line agents and in those with relapse, treatment failure, or M. tuberculosis resistant to certain first-line agents.218 231 276 440 If a fluoroquinolone used in multiple-drug regimens for treatment of active tuberculosis, ATS, CDC, IDSA, and others recommend levofloxacin or moxifloxacin.218 231 276 440
Consider that fluoroquinolone-resistant M. tuberculosis reported and there are increasing reports of extensively drug-resistant tuberculosis (XDR tuberculosis).70 71 72 74 75 XDR tuberculosis is caused by M. tuberculosis resistant to rifampin and isoniazid (multiple-drug resistant strains) that also are resistant to a fluoroquinolone and at least one parenteral second-line antimycobacterial (capreomycin, kanamycin, amikacin).71 72
Consult most recent ATS, CDC, and IDSA recommendations for treatment of tuberculosis for more specific information.218 440
Other Mycobacterial Infections
Has been used in multiple-drug regimens for treatment of disseminated infections caused by M. avium complex† (MAC).440
ATS and IDSA state that role of fluoroquinolones in treatment of MAC infections not established.675 If a fluoroquinolone is included in multiple-drug treatment regimen (e.g., for macrolide-resistant MAC infections), moxifloxacin or levofloxacin may be preferred,440 675 although many strains are resistant in vitro.675
Consult most recent ATS, CDC, and IDSA recommendations for treatment of other mycobacterial infections for more specific information.440 675
Nongonococcal Urethritis
Alternative for treatment of nongonococcal urethritis† (NGU).344 CDC recommends azithromycin or doxycycline;344 alternatives are erythromycin, levofloxacin, or ofloxacin.344
Pelvic Inflammatory Disease
Alternative for treatment of acute PID†.344 Do not use in any infections that may involve N. gonorrhoeae.114 116 344
When combined IM and oral regimen used for treatment of mild to moderately severe acute PID, CDC recommends a single IM dose of ceftriaxone, cefoxitin (with oral probenecid), or cefotaxime given in conjunction with oral doxycycline (with or without oral metronidazole).344 If a parenteral cephalosporin not feasible (e.g., because of cephalosporin allergy), CDC states regimen of oral levofloxacin, ofloxacin, or moxifloxacin given in conjunction with oral metronidazole can be considered if community prevalence and individual risk of gonorrhea is low and diagnostic testing for gonorrhea performed.344 If QRNG are identified or if in vitro susceptibility cannot be determined (e.g., only nucleic acid amplification test [NAAT] for gonorrhea available), consultation with infectious disease specialist recommended.344
Plague
Treatment of plague, including pneumonic and septicemic plague, caused by Yersinia pestis.1 2 8 683 688 Streptomycin (or gentamicin) historically has been considered regimen of choice for treatment of plague;197 292 683 688 alternatives are doxycycline (or tetracycline), chloramphenicol (a drug of choice for plague meningitis), fluoroquinolones (ciprofloxacin [a drug of choice for plague meningitis], levofloxacin, moxifloxacin), or co-trimoxazole (may be less effective than other alternatives).197 292 683 688 Regimens recommended for treatment of naturally occurring or endemic bubonic, septicemic, or pneumonic plague also recommended for plague that occurs following exposure to Y. pestis in the context of biologic warfare or bioterrorism.683 688
Postexposure prophylaxis following high-risk exposure to Y. pestis (e.g., household, hospital, or other close contact with an individual who has pneumonic plague; laboratory exposure to viable Y. pestis; confirmed exposure in the context of biologic warfare or bioterrorism).1 2 8 683 688 Drugs of choice for such prophylaxis are doxycycline (or tetracycline) or a fluoroquinolone (ciprofloxacin, levofloxacin, moxifloxacin, ofloxacin).683 688
Levofloxacin Dosage and Administration
Administration
Administer orally1 8 or by slow IV infusion.2 Do not give IM, sub-Q, intrathecally, or intraperitoneally.2
IV route indicated in patients who do not tolerate or are unable to take the drug orally and in other patients when the IV route offers a clinical advantage.2 Oral and IV routes considered interchangeable because pharmacokinetics are similar.1 2 8
Patients receiving oral or IV levofloxacin should be well hydrated and instructed to drink fluids liberally to prevent highly concentrated urine and formation of crystals in urine.1 2 8
Oral Administration
Tablets: Administer without regard to meals.1 Do not use tablets in pediatric patients weighing <30 kg.1
Oral solution: Administer 1 hour before or 2 hours after meals.8 (See Food under Pharmacokinetics.)
Tablets or oral solution: Administer orally at least 2 hours before or 2 hours after antacids containing magnesium or aluminum, metal cations (e.g., iron), sucralfate, multivitamins or dietary supplements containing iron or zinc, or buffered didanosine (pediatric oral solution admixed with antacid).1 5 8 (See Interactions.)
IV Infusion
Premixed injection for IV infusion containing 5 mg/mL in 5% dextrose (single-use flexible container): Use without further dilution.2
Concentrate for injection containing 25 mg/mL (single-use vials): Must be diluted prior to IV infusion.2
Do not admix with other drugs or infuse simultaneously through same tubing with other drugs.2 Do not infuse through same tubing with any solution containing multivalent cations (e.g., magnesium).2 If same administration set is used for sequential infusion of several different drugs, flush tubing before and after administration using an IV solution compatible with levofloxacin and the other drug(s).2
Premixed injection for IV infusion and concentrate for injection for IV infusion contain no preservatives;2 discard any unused portions.2
For solution and drug compatibility information, see Compatibility under Stability.
Dilution
Concentrate for injection containing 25 mg/mL (single-use vials): Dilute with a compatible IV solution prior to IV infusion to provide a solution containing 5 mg/mL.2
Rate of Administration
Administer doses of 250 or 500 mg by IV infusion over 60 minutes;2 administer doses of 750 mg by IV infusion over 90 minutes.2
Rapid IV infusion or injection associated with hypotension and must be avoided.2
Dosage
Dosage of oral and IV levofloxacin is identical.1 2 8
Dosage adjustments not needed when switching from IV to oral administration.1 2 8
Because safety of levofloxacin given for >28 days in adults and >14 days in pediatric patients not studied, manufacturers state use prolonged therapy only when potential benefits outweigh risks.1 2 8
Pediatric Patients
Anthrax
Postexposure Prophylaxis Following Exposure in the Context of Biologic Warfare or Bioterrorism
Oral or IVPediatric patients as young as 1 month of age†: AAP suggests 8 mg/kg (up to 250 mg) every 12 hours in those weighing <50 kg or 500 mg once daily in those weighing >50 kg.671
Children ≥6 months of age weighing <50 kg: Manufacturer recommends 8 mg/kg (up to 250 mg) every 12 hours.1 2 8
Children ≥6 months of age weighing >50 kg: Manufacturer recommends 500 mg once daily.1 2 8
Initiate prophylaxis as soon as possible following suspected or confirmed exposure to aerosolized B. anthracis.1 2 8 668 683
Because of possible persistence of B. anthracis spores in lung tissue following an aerosol exposure, CDC, AAP, and others recommend that anti-infective postexposure prophylaxis be continued for 60 days following a confirmed exposure.668 671 672 673 683
Treatment of Uncomplicated Cutaneous Anthrax (Biologic Warfare or Bioterrorism Exposure)†
OralPediatric patients ≥1 month of age†: AAP recommends 8 mg/kg (up to 250 mg) every 12 hours in those weighing <50 kg and 500 mg once daily in those weighing >50 kg.671
Recommended duration is 60 days after illness onset if cutaneous anthrax occurred after exposure to aerosolized B. anthracis spores in the context of biologic warfare or bioterrorism.671
Treatment of Systemic Anthrax (Biologic Warfare or Bioterrorism Exposure)†
IVPediatric patients ≥1 month of age† with systemic anthrax: 8 mg/kg (up to 250 mg) every 12 hours in those weighing <50 kg or 500 mg once daily in those weighing >50 kg.671
Pediatric patients ≥1 month of age† with systemic anthrax if meningitis excluded: 10 mg/kg (up to 250 mg) every 12 hours in those weighing <50 kg or 500 mg once daily in those weighing >50 kg.671
Used in multiple-drug parenteral regimen for initial treatment of systemic anthrax (inhalational, GI, meningitis, or cutaneous anthrax with systemic involvement, lesions on the head or neck, or extensive edema).671 Continue parenteral regimen for ≥2–3 weeks until patient is clinically stable and can be switched to appropriate oral anti-infective.671
If systemic anthrax occurred after exposure to aerosolized B. anthracis spores in the context of biologic warfare or bioterrorism, continue oral follow-up regimen until 60 days after illness onset.671
OralPediatric patients ≥1 month of age† (follow-up after initial multiple-drug parenteral regimen): 8 mg/kg (up to 250 mg) every 12 hours in those weighing <50 kg or 500 mg once daily in those weighing ≥50 kg.671
If systemic anthrax occurred after exposure to aerosolized B. anthracis spores in the context of biologic warfare or bioterrorism, continue oral follow-up regimen until 60 days after illness onset.672 673
Plague
Treatment or Prophylaxis of Plague
Oral or IVChildren ≥6 months of age weighing <50 kg: 8 mg/kg (up to 250 mg) every 12 hours for 10–14 days.1 2 8
Children ≥6 months of age weighing >50 kg: 500 mg once daily for 10–14 days.1 2 8 Higher dosage (i.e., 750 mg once daily) may be used if clinically indicated.1 2 8
Initiate as soon as possible after suspected or known exposure to Y. pestis.1 2 8
Adults
Respiratory Tract Infections
Acute Bacterial Sinusitis
Oral or IV500 mg once every 24 hours for 10–14 days.1 2 8 (See Respiratory Tract Infections under Uses.)
Alternatively, 750 mg once every 24 hours for 5 days.1 2 8
Acute Bacterial Exacerbations of Chronic Bronchitis
Oral or IV500 mg once every 24 hours for 7 days.1 2 8 (See Respiratory Tract Infections under Uses.)
Community-acquired Pneumonia (CAP)
Oral or IVS. aureus, S. pneumoniae (including MDRSP), K. pneumoniae, L. pneumophila, M. catarrhalis: 500 mg once every 24 hours for 7–14 days.1 2 8
S. pneumoniae (except MDRSP), H. influenzae, H. parainfluenzae, M. pneumoniae, or C. pneumoniae: 500 mg once every 24 hours for 7–14 days or, alternatively, 750 mg once every 24 hours for 5 days.1 2 8
If used for empiric treatment of CAP or treatment of CAP caused by Ps. aeruginosa, IDSA and ATS recommend 750 mg once daily.512
IDSA and ATS state that CAP should be treated for a minimum of 5 days and patients should be afebrile for 48–72 hours before discontinuing anti-infective therapy.512
Nosocomial Pneumonia
Oral or IV750 mg once every 24 hours for 7–14 days.1 2 8
Skin and Skin Structure Infections
Uncomplicated Infections
Oral or IV500 mg once every 24 hours for 7–10 days.1 2 8
Complicated Infections
Oral or IV750 mg once every 24 hours for 7–14 days.1 2 8
Urinary Tract Infections (UTIs) and Prostatitis
Uncomplicated UTIs
Oral or IV250 mg once every 24 hours for 3 days.1 2 8 (See Urinary Tract Infections [UTIs] and Prostatitis under Uses.)
Complicated UTIs
Oral or IVE. faecalis, E. cloacae, or Ps. aeruginosa: 250 mg once every 24 hours for 10 days.1 2 8
E. coli, K. pneumoniae, or P. mirabilis: 250 mg once every 24 hours for 10 days or, alternatively, 750 mg once every 24 hours for 5 days.1 2 8
Acute Pyelonephritis
Oral or IVE. coli: 250 mg once every 24 hours or 10 days or, alternatively, 750 mg once every 24 hours for 5 days.1 2 8
Chronic Prostatitis
Oral or IV500 mg once every 24 hours for 28 days.1 2 8
GI Infections†
Campylobacter Infections†
Oral or IVHIV-infected: 750 mg once daily.440
Recommended treatment duration is 7–10 days for gastroenteritis or ≥14 days for bacteremic infections.440 Duration of 2–6 weeks recommended for recurrent infections.440
Salmonella Gastroenteritis†
Oral or IVHIV-infected: 750 mg once daily.440
Recommended treatment duration is 7–14 days if CD4+ T-cells ≥200 cells/mm3 (≥14 days if bacteremic or infection is complicated) or 2–6 weeks if CD4+ T-cells <200 cells/mm3.440
Consider secondary prophylaxis in those with recurrent bacteremia;440 also may consider in those with recurrent gastroenteritis (with or without bacteremia) or with CD4+ T-cells <200 cells/mm3 and severe diarrhea.440 Discontinue secondary prophylaxis if Salmonella infection resolves and there has been a sustained response to antiretroviral therapy with CD4+ T-cells >200 cells/mm3.440
Shigella Infections†
Oral or IVHIV-infected: 750 mg once daily.440
Recommended treatment duration is 7–10 days for gastroenteritis or ≥14 days for bacteremic infections.440 Up to 6 weeks may be required for recurrent infections, especially if CD4+ T-cells <200 cells/mm3.440
Treatment of Travelers’ Diarrhea†
Oral500 mg once daily for 1–3 days.305 679
Prevention of Travelers’ Diarrhea†
OralAnti-infective prophylaxis generally discouraged (see GI Infections under Uses);305 525 if such prophylaxis used, give during period of risk (not exceeding 2–3 weeks) beginning day of travel and continuing for 1 or 2 days after leaving area of risk.305
Helicobacter pylori Infection
Oral500 mg once daily usually used;235 236 237 250 mg once daily also has been used.235
Used as a component of multiple-drug regimen (see GI Infections under Uses).235 236 237
Anthrax
Postexposure Prophylaxis of Anthrax (Biologic Warfare or Bioterrorism Exposure)
Oral or IV500 mg once daily recommended by manufacturers.1 2 8
750 mg once daily recommended by CDC.672 673
Initiate prophylaxis as soon as possible following suspected or confirmed exposure to aerosolized B. anthracis.1 2 8 668 673 683
Because of possible persistence of B. anthracis spores in lung tissue following an aerosol exposure, CDC and others recommend that anti-infective postexposure prophylaxis be continued for 60 days following a confirmed exposure.668 672 673 683
Treatment of Uncomplicated Cutaneous Anthrax (Biologic Warfare or Bioterrorism Exposure)†
OralRecommended duration is 60 days if cutaneous anthrax occurred after exposure to aerosolized B. anthracis spores in the context of biologic warfare or bioterrorism.668 672 673 683 686
Treatment of Systemic Anthrax (Biologic Warfare or Bioterrorism Exposure)†
IVUsed in multiple-drug parenteral regimen for initial treatment of systemic anthrax (inhalational, GI, meningitis, or cutaneous with systemic involvement, lesions on the head or neck, or extensive edema).672 673 Continue parenteral regimen for ≥2–3 weeks until patient is clinically stable and can be switched to appropriate oral anti-infective.672 673
If anthrax occurred after exposure to aerosolized B. anthracis spores in the context of biologic warfare or bioterrorism, continue oral follow-up regimen until 60 days after illness onset.672 673
Chlamydial Infections†
Urogenital Infections†
Oral500 mg once daily for 7 days recommended by CDC for infections caused by C. trachomatis.344
Gonorrhea and Associated Infections†
Epididymitis†
Oral500 mg once daily for 10 days recommended by CDC.344
Use only when epididymitis† most likely caused by sexually transmitted enteric bacteria (e.g., E. coli) and N. gonorrhoeae ruled out.344 (See Gonorrhea and Associated Infections under Uses.)
Mycobacterial Infections†
Active Tuberculosis†
Oral or IV0.5–1 g once daily.218 Must be used in conjunction with other antituberculosis agents.218
ATS, CDC, and IDSA state data insufficient to date to support intermittent levofloxacin regimens for treatment of tuberculosis.218
Disseminated MAC Infections
OralHIV-infected: 500 mg once daily.440
Nongonococcal Urethritis†
Oral
500 mg once daily for 7 days recommended by CDC.344
Pelvic Inflammatory Disease†
Oral
500 mg once daily for 14 days given in conjunction with oral metronidazole (500 mg twice daily for 14 days).344
Use only when cephalosporins not feasible, community prevalence and individual risk of gonorrhea low, and in vitro susceptibility confirmed.344 (See Pelvic Inflammatory Disease under Uses.)
IV
500 mg once daily;344 used with or without IV metronidazole (500 mg every 8 hours).344
Use only when cephalosporins not feasible, community prevalence and individual risk of gonorrhea are low, and in vitro susceptibility confirmed.344 (See Pelvic Inflammatory Disease under Uses.)
Plague
Treatment or Prophylaxis of Plague
Oral or IV500 mg once daily for 10–14 days.1 2 8 Higher dosage (i.e., 750 mg once daily) may be used if clinically indicated.1 2 8
Initiate as soon as possible after suspected or known exposure to Y. pestis.1 2 8
Special Populations
Hepatic Impairment
Dosage adjustments not required.1 2 8
Renal Impairment
Adjust dosage in adults with Clcr <50 mL/minute.1 2 8 (See Table 1.) Adjustments not needed when used for treatment of uncomplicated UTIs in patients with renal impairment.1 2 8
Dosage recommendations not provided by manufacturer for pediatric patients with renal impairment.1 2 8
|
Usual Daily Dosage for Normal Renal Function (Clcr ≥ 50 mL/min) |
Clcr (mL/min) |
Dosage for Renal Impairment |
|---|---|---|
|
250 mg |
20–49 |
Dosage adjustment not required |
|
250 mg |
10–19 |
Uncomplicated UTIs: Dosage adjustment not required. Other infections: 250 mg once every 48 hours |
|
250 mg |
Hemodialysis or CAPD patients |
Information not available |
|
500 mg |
20–49 |
Initial 500-mg dose, then 250 mg once every 24 hours |
|
500 mg |
10–19 |
Initial 500-mg dose, then 250 mg once every 48 hours |
|
500 mg |
Hemodialysis or CAPD patients |
Initial 500-mg dose, then 250 mg once every 48 hours; supplemental doses not required after dialysis |
|
750 mg |
20–49 |
750 mg once every 48 hours |
|
750 mg |
10–19 |
Initial 750-mg dose, then 500 mg once every 48 hours |
|
750 mg |
Hemodialysis or CAPD patients |
Initial 750-mg dose, then 500 mg once every 48 hours; supplemental doses not required after dialysis |
Geriatric Patients
No dosage adjustments except those related to renal impairment.1 2 8 (See Renal Impairment under Dosage and Administration.)
Cautions for Levofloxacin
Contraindications
Warnings/Precautions
Warnings
Disabling and Potentially Irreversible Serious Adverse Reactions
Systemic fluoroquinolones, including levofloxacin, associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that can occur together in the same patient.1 2 8 140 145 May occur within hours to weeks after a systemic fluoroquinolone is initiated;1 have occurred in all age groups and in patients without preexisting risk factors for such adverse reactions.1 2 8
Immediately discontinue levofloxacin at first signs or symptoms of any serious adverse reactions.1 2 8 140 145
Avoid systemic fluoroquinolones, including levofloxacin, in patients who have experienced any of the serious adverse reactions associated with fluoroquinolones.1 2 8 140 145
Tendinitis and Tendon Rupture
Systemic fluoroquinolones, including levofloxacin, are associated with an increased risk of tendinitis and tendon rupture in all age groups.1 2 8 128 129
Risk of developing fluoroquinolone-associated tendinitis and tendon rupture is increased in older adults (usually those >60 years of age), individuals receiving concomitant corticosteroids, and kidney, heart, or lung transplant recipients.1 2 8 128 129 (See Geriatric Use under Cautions.)
Other factors that may independently increase the risk of tendon rupture include strenuous physical activity, renal failure, and previous tendon disorders such as rheumatoid arthritis.1 2 8 Tendinitis and tendon rupture have been reported in patients receiving fluoroquinolones who did not have any risk factors for such adverse reactions.1 2 8
Fluoroquinolone-associated tendinitis and tendon rupture most frequently involve the Achilles tendon;1 2 8 also reported in rotator cuff (shoulder), hand, biceps, thumb, and other tendon sites.1 2 8
Tendinitis and tendon rupture can occur within hours or days after levofloxacin is initiated or as long as several months after completion of therapy and can occur bilaterally.1 2 8
Immediately discontinue levofloxacin if pain, swelling, inflammation, or rupture of a tendon occurs.1 2 8 128 129 (See Advice to Patients.)
Avoid systemic fluoroquinolones, including levofloxacin, in patients who have a history of tendon disorders or have experienced tendinitis or tendon rupture.1 2 8
Peripheral Neuropathy
Systemic fluoroquinolones, including levofloxacin, are associated with an increased risk of peripheral neuropathy.1 2 8
Sensory or sensorimotor axonal polyneuropathy affecting small and/or large axons resulting in paresthesias, hypoesthesias, dysesthesias, and weakness reported with systemic fluoroquinolones, including levofloxacin.1 2 8 130 Symptoms may occur soon after initiation of the drug and, in some patients, may be irreversible.1 130
Immediately discontinue levofloxacin if symptoms of peripheral neuropathy (e.g., pain, burning, tingling, numbness, and/or weakness) occur or if there are other alterations in sensations (e.g., light touch, pain, temperature, position sense, vibratory sensation).1 2 8 130 (See Advice to Patients.)
Avoid systemic fluoroquinolones, including levofloxacin, in patients who have experienced peripheral neuropathy.1 2 8
CNS Effects
Systemic fluoroquinolones, including levofloxacin, are associated with increased risk of psychiatric adverse effects, including toxic psychosis,1 2 8 hallucinations,1 2 8 paranoia,1 2 8 depression,1 2 8 suicidal thoughts or acts,1 2 8 anxiety,1 2 8 agitation,1 2 8 171 restlessness,1 2 8 nervousness,1 2 8 171 confusion,1 2 8 delirium,1 2 8 171 disorientation,1 2 8 171 disturbances in attention,1 2 8 171 insomnia,1 2 8 nightmares,1 2 8 and memory impairment.1 2 8 171 Attempted or completed suicides reported, especially in patients with a history of depression or underlying risk factor for depression.1 2 8 These adverse effects may occur after first dose.1 2 8
Systemic fluoroquinolones, including levofloxacin, are associated with increased risk of seizures (convulsions), increased intracranial pressure (including pseudotumor cerebri), dizziness, and tremors.1 2 8 Use with caution in patients with known or suspected CNS disorders that predispose to seizures or lower the seizure threshold (e.g., severe cerebral arteriosclerosis, epilepsy) or with other risk factors that predispose to seizures or lower the seizure threshold (e.g., certain drugs, renal impairment).1 2 8
If psychiatric or other CNS effects occur, immediately discontinue levofloxacin and institute appropriate measures.1 2 8 (See Advice to Patients.)
Exacerbation of Myasthenia Gravis
Fluoroquinolones, including levofloxacin, have neuromuscular blocking activity and may exacerbate muscle weakness in myasthenia gravis patients;1 death or need for ventilatory support reported.1 2 8
Avoid use in patients with known history of myasthenia gravis.1 2 8 (See Advice to Patients.)
Sensitivity Reactions
Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity and/or anaphylactic reactions reported in patients receiving fluoroquinolones, including levofloxacin.1 These reactions often occur with first dose.1 2 8
Some hypersensitivity reactions have been accompanied by cardiovascular collapse, hypotension or shock, seizures, loss of consciousness, tingling, angioedema (e.g., edema or swelling of the tongue, larynx, throat, or face), airway obstruction (e.g., bronchospasm, shortness of breath, acute respiratory distress), dyspnea, urticaria, pruritus, and other severe skin reactions.1 2 8
Other serious and sometimes fatal adverse reactions reported with fluoroquinolones, including levofloxacin, that may or may not be related to hypersensitivity reactions include one or more of the following: fever, rash or other severe dermatologic reactions (e.g., toxic epidermal necrolysis, Stevens-Johnson syndrome); vasculitis, arthralgia, myalgia, serum sickness; allergic pneumonitis; interstitial nephritis, acute renal insufficiency or failure; hepatitis, jaundice, acute hepatic necrosis or failure; anemia (including hemolytic and aplastic), thrombocytopenia (including thrombotic thrombocytopenic purpura), leukopenia, agranulocytosis, pancytopenia, and/or other hematologic effects.1 2 8
Immediately discontinue levofloxacin at first appearance of rash, jaundice, or any other sign of hypersensitivity.1 2 8 Institute appropriate therapy as indicated (e.g., epinephrine, corticosteroids, maintenance of an adequate airway and oxygen).1 2 8
Photosensitivity Reactions
Moderate to severe photosensitivity/phototoxicity reactions reported with fluoroquinolones, including levofloxacin1 2 8
Phototoxicity may manifest as exaggerated sunburn reactions (e.g., burning, erythema, exudation, vesicles, blistering, edema) on areas exposed to sun or artificial ultraviolet (UV) light (usually the face, neck, extensor surfaces of forearms, dorsa of hands).1 2 8
Avoid unnecessary or excessive exposure to sunlight or artificial UV light (tanning beds, UVA/UVB treatment) while receiving levofloxacin.1 2 8 If patient needs to be outdoors, they should wear loose-fitting clothing that protects skin from sun exposure and use other sun protection measures (sunscreen).1 2 8
Discontinue levofloxacin if photosensitivity or phototoxicity (sunburn-like reaction, skin eruption) occurs.1 2 8
Other Warnings/Precautions
Hepatotoxicity
Severe hepatotoxicity, including acute hepatitis, has occurred in patients receiving levofloxacin and sometimes resulted in death.1 2 8 Most cases occurred within 6–14 days of initiation of levofloxacin therapy and were not associated with hypersensitivity reactions.1 2 8 The majority of fatalities were in geriatric patients ≥65 years of age.1 2 8 (See Geriatric Use under Cautions.)
Immediately discontinue levofloxacin in any patient who develops symptoms of hepatitis (e.g., loss of appetite, nausea, vomiting, fever, weakness, tiredness, right upper quadrant tenderness, itching, yellowing of the skin or eyes, light colored bowel movements, or dark colored urine).1 2 8
Prolongation of QT Interval
Prolonged QT interval leading to ventricular arrhythmias, including torsades de pointes, reported with some fluoroquinolones, including levofloxacin.1 2 8 37
Avoid use in patients with a history of prolonged QT interval or uncorrected electrolyte disorders (e.g., hypokalemia).1 2 8 Also avoid use in those receiving class IA (e.g., quinidine, procainamide) or class III (e.g., amiodarone, sotalol) antiarrhythmic agents.1 2 8
Risk of prolonged QT interval may be increased in geriatric patients.1 2 8 (See Geriatric Use under Cautions.)
Risk of Aortic Aneurysm and Dissection
Rupture or dissection of aortic aneurysms reported in patients receiving systemic fluoroquinolones.172 Epidemiologic studies indicate an increased risk of aortic aneurysm and dissection within 2 months following use of systemic fluoroquinolones, particularly in geriatric patients.1 2 8 Cause for this increased risk not identified.1 2 8 172
Unless there are no other treatment options, do not use systemic fluoroquinolones, including levofloxacin, in patients who have an aortic aneurysm or are at increased risk for an aortic aneurysm.1 2 8 172 This includes geriatric patients and patients with peripheral atherosclerotic vascular disease, hypertension, or certain genetic conditions (e.g., Marfan syndrome, Ehlers-Danlos syndrome).172
If patient reports adverse effects suggestive of aortic aneurysm or dissection, immediately discontinue the fluoroquinolone.172 (See Advice to Patients.)
Hypoglycemia or Hyperglycemia
Systemic fluoroquinolones, including levofloxacin, are associated with alterations in blood glucose concentrations, including symptomatic hypoglycemia and hyperglycemia.1 2 8 171 Blood glucose disturbances during fluoroquinolone therapy usually have occurred in patients with diabetes mellitus receiving an oral antidiabetic agent (e.g., glyburide) or insulin.1 2 8 171
Severe cases of hypoglycemia resulting in coma or death reported with some systemic fluoroquinolones.1 2 8 171 Although most reported cases of hypoglycemic coma involved patients with risk factors for hypoglycemia (e.g., older age, diabetes mellitus, renal insufficiency, concomitant use of antidiabetic agents [especially sulfonylureas]), some involved patients receiving a fluoroquinolone who were not diabetic and not receiving an oral antidiabetic agent or insulin.171
Carefully monitor blood glucose concentrations when levofloxacin used in diabetic patients.1 2 8 82
If a hypoglycemic reaction occurs, discontinue the fluoroquinolone and initiate appropriate therapy immediately.1 2 8 (See Advice to Patients.)
Musculoskeletal Effects
Increased incidence of musculoskeletal disorders (arthralgia, arthritis, tendinopathy, gait abnormality) reported in pediatric patients receiving levofloxacin.1 2 8 Use in pediatric patients only for inhalational anthrax (postexposure) or treatment or prophylaxis of plague and only in those 6 months of age or older.1 2 8 (See Pediatric Use under Cautions.)
Fluoroquinolones, including levofloxacin, cause arthropathy and osteochondrosis in immature animals of various species.1 2 8 118 119 120 121 122 125 126 Persistent lesions in cartilage reported in levofloxacin studies in immature dogs.1
C. difficile-associated Diarrhea and Colitis
Treatment with anti-infectives alters normal colon flora and may permit overgrowth of Clostridioides difficile (formerly known as Clostridium difficile).1 2 8 302 303 304 C. difficile infection (CDI) and C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) reported with nearly all anti-infectives, including levofloxacin, and may range in severity from mild diarrhea to fatal colitis.1 2 8 102 106 107 302 303 304 C. difficile produces toxins A and B which contribute to development of CDAD;1 2 8 302 hypertoxin-producing strains of C. difficile are associated with increased morbidity and mortality since they may be refractory to anti-infectives and colectomy may be required.1 2 8
Consider CDAD if diarrhea develops during or after therapy and manage accordingly.1 2 8 302 303 304 Obtain careful medical history since CDAD may occur as late as 2 months or longer after anti-infective therapy is discontinued.1 2 8 302 303 304
If CDAD is suspected or confirmed, discontinue anti-infectives not directed against C. difficile as soon as possible.302 Initiate appropriate anti-infective therapy directed against C. difficile (e.g., vancomycin, fidaxomicin, metronidazole), supportive therapy (e.g., fluid and electrolyte management, protein supplementation), and surgical evaluation as clinically indicated.1 2 8 302 303 304
Selection and Use of Anti-infectives
Use for treatment of acute bacterial sinusitis, acute bacterial exacerbations of chronic bronchitis, or uncomplicated UTIs only when no other treatment options available.1 2 8 140 145 Because levofloxacin, like other systemic fluoroquinolones, has been associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that can occur together in the same patient, risks of serious adverse reactions outweigh benefits for patients with these infections.140 145
To reduce development of drug-resistant bacteria and maintain effectiveness of levofloxacin and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.1 2 8
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing.1 2 8 In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.1 2 8
Information on test methods and quality control standards for in vitro susceptibility testing of antibacterial agents and specific interpretive criteria for such testing recognized by FDA is available at [Web].1 2 8
Specific Populations
Pregnancy
No adequate and well-controlled studies in pregnant women;1 2 8 animal studies (rats and rabbits) did not reveal evidence of fetal harm.1 2 8
Use during pregnancy only if potential benefits justify potential risks to fetus.1 2 8
Lactation
Distributed into milk following oral or IV administration.80
Discontinue nursing or the drug.1 2 8
Pediatric Use
Safety and efficacy not established for any indication in infants <6 months of age.1 2 8
Labeled by FDA for inhalational anthrax (postexposure) or for treatment or prophylaxis of plague in adolescents and children ≥6 months of age.1 2 8 Safety and efficacy not established for any other indication in this age group.1 2 8
Increased incidence of musculoskeletal disorders reported in pediatric patients receiving levofloxacin.1 2 8 Causes arthropathy and osteochondrosis in juvenile animals.1 2 8 (See Musculoskeletal Effects under Cautions.)
AAP states use of a systemic fluoroquinolone may be justified in children <18 years of age in certain specific circumstances when there are no safe and effective alternatives and the drug is known to be effective.110 292
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.1 2 8
Risk of severe tendon disorders, including tendon rupture, is increased in older adults (usually those >60 years of age).1 2 8 128 129 This risk is further increased in those receiving concomitant corticosteroids.1 2 8 128 129 (See Tendinitis and Tendon Rupture under Cautions.) Use caution in geriatric adults, especially those receiving concomitant corticosteroids.1
Serious and sometimes fatal hepatotoxicity reported with levofloxacin;1 2 8 majority of fatalities have occurred in geriatric patients ≥65 years of age.1 2 8 (See Hepatotoxicity under Cautions.)
Risk of prolonged QT interval leading to ventricular arrhythmias may be increased in geriatric patients, especially those receiving concurrent therapy with other drugs that can prolong QT interval (e.g., class IA or III antiarrhythmic agents) or with risk factors for torsades de pointes (e.g., known QT prolongation, uncorrected hypokalemia).1 2 8 (See Prolongation of QT Interval under Cautions.)
Risk of aortic aneurysm and dissection may be increased in geriatric patients.1 2 8 (See Risk of Aortic Aneurysm and Dissection under Cautions.)
Consider age-related decreases in renal function when selecting dosage.1 2 8 (See Renal Impairment under Dosage and Administration.)
Hepatic Impairment
Pharmacokinetics not studied in patients with hepatic impairment, but pharmacokinetic alterations unlikely.1 2 8
Renal Impairment
Substantially decreased clearance and increased half-life.1 2 8 Use with caution and adjust dosage.1 2 8 (See Renal Impairment under Dosage and Administration.)
Perform appropriate renal function tests prior to and during therapy.1 2 8
Common Adverse Effects
GI effects (nausea, diarrhea, constipation), headache, insomnia, dizziness.1 2 8
Drug Interactions
Drugs That Prolong QT Interval
Potential pharmacologic interaction (additive effect on QT interval prolongation).1 2 8 Avoid use in patients receiving class IA (e.g., quinidine, procainamide) or class III (e.g., amiodarone, sotalol) antiarrhythmic agents.1 2 8 (See Prolongation of QT Interval under Cautions.)
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum- or magnesium-containing) |
Decreased absorption of oral levofloxacin;1 8 5 7 data not available regarding IV levofloxacin2 |
Administer oral levofloxacin at least 2 hours before or 2 hours after such antacids1 8 |
|
Antiarrhythmic agents |
Potential additive effects on QT interval prolongation1 2 8 Procainamide: Increased half-life and decreased clearance of procainamide84 |
Avoid levofloxacin in patients receiving class IA (e.g., quinidine, procainamide) or class III (e.g., amiodarone, sotalol) antiarrhythmic agents1 2 8 |
|
Anticoagulants, oral (warfarin) |
Monitor PT, INR, or other suitable coagulation tests and monitor for bleeding1 2 8 |
|
|
Antidiabetic agents (e.g., insulin, glyburide) |
Alterations in blood glucose (hyperglycemia and hypoglycemia) reported1 2 8 |
Closely monitor blood glucose;1 2 8 if hypoglycemic reaction occurs, immediately discontinue levofloxacin and initiate appropriate therapy1 2 8 |
|
Cimetidine |
Not considered clinically important;1 2 8 levofloxacin dosage adjustments not warranted1 2 8 |
|
|
Corticosteroids |
Increased risk of tendinitis or tendon rupture, especially in patients >60 years of age1 2 8 |
|
|
Cyclosporine or tacrolimus |
Possible increased AUC of cyclosporine or tacrolimus92 |
Manufacturer of levofloxacin states dosage adjustments not needed for either drug when levofloxacin used with cyclosporine;1 2 8 some clinicians suggest monitoring plasma concentrations of cyclosporine or tacrolimus92 |
|
Didanosine |
Possible decreased absorption of oral levofloxacin;1 8 data not available regarding IV levofloxacin2 |
Administer oral levofloxacin at least 2 hours before or 2 hours after buffered didanosine (pediatric oral solution admixed with antacid)1 8 |
|
Digoxin |
No evidence of clinically important effect on pharmacokinetics of digoxin or levofloxacin1 2 8 83 |
|
|
Iron preparations |
Decreased absorption of oral levofloxacin;1 8 data not available regarding IV levofloxacin2 |
Administer oral levofloxacin at least 2 hours before or after ferrous sulfate and dietary supplements containing iron1 8 |
|
Multivitamins and mineral supplements |
Decreased absorption of oral levofloxacin;1 94 8 data not available regarding IV levofloxacin2 |
Administer oral levofloxacin at least 2 hours before or 2 hours after supplements containing zinc, calcium, magnesium, or iron1 8 94 |
|
NSAIAs |
Possible increased risk of CNS stimulation, seizures;1 2 8 91 animal studies suggest risk may be less than that associated with some other fluoroquinolones91 |
|
|
Probenecid |
Not considered clinically important;1 2 8 levofloxacin dosage adjustments not required1 2 8 |
|
|
Psychotherapeutic agents |
Fluoxetine or imipramine: Potential additive effect on QT interval prolongation85 |
|
|
Tests for opiates |
Possibility of false-positive results for opiates in patients receiving some quinolones, including levofloxacin, when commercially available urine screening immunoassay kits are used1 2 8 |
Positive opiate urine screening test results may need to be confirmed using more specific methods1 2 8 |
|
Sucralfate |
Decreased absorption of oral levofloxacin;1 8 data not available regarding IV levofloxacin2 |
Administer oral levofloxacin at least 2 hours before or 2 hours after sucralfate1 8 86 |
|
Theophylline |
No evidence of clinically important pharmacokinetic interaction with levofloxacin;1 2 8 increased theophylline concentrations and increased risk of theophylline-related adverse effects reported with some other quinolones1 2 8 |
Closely monitor theophylline concentrations and make appropriate dosage adjustments;1 2 8 consider that adverse theophylline effects (e.g., seizures) may occur with or without elevated theophylline concentrations1 2 8 |
Levofloxacin Pharmacokinetics
Absorption
Bioavailability
Single 500- or 750-mg dose as tablets: Absolute bioavailability approximately 99%.1 8
Rapidly absorbed from GI tract.1 8 Peak plasma concentrations usually attained 1–2 hours after an oral dose;1 8 steady-state plasma concentrations attained within 48 hours with once-daily regimens.1 8
Tablets and oral solution are bioequivalent.8
Plasma concentrations and AUC after oral administration of tablets are similar to those after IV administration.1 2 8
Food
Tablets: Food slightly prolongs time to peak plasma concentration and slightly decreases peak concentrations (approximately 14%);1 86 not considered clinically important.1
Oral solution: Food decreases peak concentrations by approximately 25%.1 8
Distribution
Extent
Widely distributed into body tissues and fluids, including skin, blister fluid, and lungs.1 2 8
Distributed into CSF.5 64 65 Following IV administration of 400 or 500 mg twice daily, CSF concentrations have been reported to be up to 47% of concurrent plasma concentrations.64 65
Distributed into milk following oral or IV administration.80
Plasma Protein Binding
24–38% bound to serum proteins, principally albumin.1 2 8
Elimination
Metabolism
Undergoes limited metabolism to inactive metabolites.1 2 8
Elimination Route
Eliminated principally as unchanged drug in urine by glomerular filtration and active tubular secretion.1 2 8 Approximately 87% of an oral dose eliminated in urine and <4% eliminated in feces.1 2 8
Not removed by hemodialysis or continuous ambulatory peritoneal dialysis (CAPD).1 2 8
Half-life
Terminal elimination half-life approximately 6–8 hours after oral or IV administration.1 2 8
Special Populations
Pediatric patients ≥6 months of age: Increased clearance and decreased plasma concentrations relative to those in adults.1 2 8
Geriatric individuals with normal renal function: Pharmacokinetics similar to that in younger adults.1 2 8
Patients with hepatic impairment: Pharmacokinetics not studied, but alterations unlikely.1 2 8
Patients with impaired renal function: Decreased clearance and prolonged half-life1 2 8 (27 hours in those with Clcr 20–49 mL/minute and 35 hours in those with Clcr <20 mL/minute).1 8
Stability
Storage
Oral
Solution
25°C (may be exposed to 15–30°C).8
Tablets
15–30°C in well-closed containers.1
Parenteral
For Injection, for IV Infusion
Single-dose vials: 15–30°C; protect from light.2 After dilution to a concentration of 5 mg/mL with compatible IV solution, stable for up to 72 hours at ≤25°C or up to 14 days at 5°C in flexible IV containers.2
Diluted solutions containing 5 mg/mL may be frozen in glass or plastic IV containers for ≤6 months at -20°C;2 after thawing at room temperature or in a refrigerator, do not refreeze.2
Contains no preservatives; discard any unused portions.2
Injection, for IV Infusion
Single-dose flexible containers: 20–25°C; do not freeze.2 Protect from light and excessive heat.2
Contains no preservatives;2 discard any unused portions.2
Compatibility
Parenteral
Solution Compatibility2 HID
|
Compatible |
|---|
|
Dextrose 5% in Ringer’s injection, lactated |
|
Dextrose 5% in sodium chloride 0.9% |
|
Dextrose 5% in water |
|
Plasma-Lyte 56 and dextrose 5% |
|
Sodium chloride 0.9% |
|
Sodium lactate 1/6 M |
|
Variable |
|
Mannitol 20% |
|
Sodium bicarbonate 5% |
Drug Compatibility
|
Compatible |
|---|
|
Linezolid |
|
Incompatible |
|
Micafungin sodium |
|
Compatible |
|---|
|
Amikacin sulfate |
|
Aminophylline |
|
Ampicillin sodium |
|
Anidulafungin |
|
Bivalirudin |
|
Caffeine citrate |
|
Cangrelor tetrasodium |
|
Caspofungin acetate |
|
Cefotaxime sodium |
|
Ceftaroline fosamil |
|
Ceftolozane sulfate-tazobactam sodium |
|
Clindamycin phosphate |
|
Cloxacillin sodium |
|
Daptomycin |
|
Dexamethasone sodium phosphate |
|
Dexmedetomidine HCl |
|
Dobutamine HCl |
|
Dopamine HCl |
|
Doripenem |
|
Epinephrine HCl |
|
Fenoldopam mesylate |
|
Fentanyl citrate |
|
Gentamicin sulfate |
|
Hetastarch in lactated electrolyte injection |
|
Hydromorphone HCL |
|
Isavuconazonium sulfate |
|
Isoproterenol HCl |
|
Lidocaine HCl |
|
Linezolid |
|
Lorazepam |
|
Magnesium sulfate |
|
Meropenem-vaborbactam |
|
Metoclopramide HCl |
|
Morphine sulfate |
|
Oxacillin sodium |
|
Pancuronium bromide |
|
Penicillin G sodium |
|
Phenobarbital sodium |
|
Phenylephrine HCl |
|
Posaconazole |
|
Potassium chloride |
|
Sodium bicarbonate |
|
Tedizolid phosphate |
|
Vancomycin HCl |
|
Incompatible |
|
Acyclovir sodium |
|
Alprostadil |
|
Azithromycin |
|
Furosemide |
|
Heparin sodium |
|
Indomethacin sodium trihydrate |
|
Letermovir |
|
Nitroglycerin |
|
Plazomicin |
|
Sodium nitroprusside |
|
Telavancin HCl |
|
Variable |
|
Insulin, regular |
Actions and Spectrum
-
Like other fluoroquinolones, levofloxacin inhibits bacterial DNA gyrase and topoisomerase IV.1 2 4 8 39
-
Spectrum of activity includes gram-positive aerobic bacteria, some gram-negative aerobic bacteria, some anaerobic bacteria, and some other organisms (e.g., Chlamydia, Mycoplasma, Mycobacterium).1 2 3 8 13 14 15 16 17 40 41 42
-
More active in vitro against gram-positive bacteria, (including S. pneumoniae) and anaerobes than some other fluoroquinolones (e.g., ciprofloxacin, ofloxacin),3 13 14 15 16 17 but less active in vitro than ciprofloxacin against Pseudomonas aeruginosa.3 14 17
-
Gram-positive aerobes: Active in vitro and in clinical infections against S. aureus (oxacillin-susceptible [methicillin-susceptible] strains only), S. epidermidis (oxacillin-susceptible strains only), S. saprophyticus, S. pneumoniae (including penicillin-resistant strains), S. pyogenes (group A β-hemolytic streptococci, GAS), and Enterococcus faecalis (many strains only moderately susceptible).1 2 3 8 Also active in vitro against S. haemolyticus, S. agalactiae (group B streptococci, GBS), groups C, G, and F streptococci, S. milleri, and viridans streptococci.1 2 3 8 Active against Bacillus anthracis in vitro and in a primate infection model.1 2 8 93
-
Gram-negative aerobes: Active in vitro and in clinical infections against H. influenzae, H. parainfluenzae, K. pneumoniae, M. catarrhalis, E. cloacae, E. coli, P. mirabilis, S. marcescens, Ps. aeruginosa (some may develop resistance during therapy), and Legionella pneumophila.1 2 8 3 Also active in vitro against Acinetobacter, Bordetella pertussis, Citrobacter, E. aerogenes, E. sakazakii, K. oxytoca, Morganella morganii, Pantoea agglomerans, P. vulgaris, Providencia, and Ps. fluorescens.1 2 8 Active against Y. pestis in vitro and in a primate infection model.1 2 8 Has in vitro activity against H. pylori,241 but resistance occurs and prevalence of levofloxacin-resistant strains may be high in some geographic areas.235 239 240
-
Anaerobes and other organisms: Active in vitro and in clinical infections against C. pneumoniae 1 2 8 and M. pneumoniae.1 2 3 8 Also active in vitro against Clostridium perfringens,1 2 3 8 Mycobacterium tuberculosis,40 41 111 and M. fortuitum.42
-
N. gonorrhoeae with decreased susceptibility to levofloxacin and other fluoroquinolones (quinolone-resistant N. gonorrhoeae; QRNG) are widely disseminated worldwide, including in the US.53 109 114 132 344
-
Resistance to fluoroquinolones can occur as the result of mutations in defined regions of DNA gyrase or topoisomerase IV (i.e., quinolone-resistance determining regions [QRDRs]) or altered efflux.1 2 8
-
Some cross-resistance occurs between levofloxacin and other fluoroquinolones.1 2 8
Advice to Patients
-
Advise patients to read manufacturer’s patient information (medication guide) prior to initiating levofloxacin therapy and each time prescription refilled.1 2 8
-
Advise patients that antibacterials (including levofloxacin) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).1 2 8
-
Importance of completing full course of therapy, even if feeling better after a few days.1 2 8
-
Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with levofloxacin or other antibacterials in the future.1 2 8
-
Advise patients that the oral solution should be taken 1 hour before or 2 hours after meals;8 tablets may be taken without regard to meals1
-
Levofloxacin should be taken at the same time each day and with liberal amounts of fluids to prevent highly concentrated urine and formation of crystals in urine.1 8
-
Importance of taking oral levofloxacin at least 2 hours before or 2 hours after aluminum- or magnesium-containing antacids, metal cations (e.g., iron), sucralfate, multivitamins containing iron or zinc, or buffered didanosine (pediatric oral solution prepared as an admixture with antacid).1 8
-
Inform patients that systemic fluoroquinolones, including levofloxacin, have been associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that may occur together in same patient.1 2 8 140 145 Advise patients to immediately discontinue levofloxacin and contact a clinician if they experience any signs or symptoms of serious adverse effects (e.g., unusual joint or tendon pain, muscle weakness, a “pins and needles” tingling or pricking sensation, numbness of the arms or legs, confusion, hallucinations) while taking the drug.1 140 145 Advise patients to talk with a clinician if they have any questions or concerns.1 140 145
-
Inform patients that systemic fluoroquinolones, including levofloxacin, are associated with an increased risk of tendinitis and tendon rupture in all age groups and this risk is increased in adults >60 years of age, individuals receiving corticosteroids, and kidney, heart, or lung transplant recipients.1 2 8 Symptoms may be irreversible.1 2 8 Importance of resting and refraining from exercise at the first sign of tendinitis or tendon rupture (e.g., pain, swelling, or inflammation of a tendon or weakness or inability to use a joint) and importance of immediately discontinuing the drug and contacting a clinician.1 2 8 (See Tendinitis and Tendon Rupture under Cautions.)
-
Inform patients that peripheral neuropathies have been reported with systemic fluoroquinolones, including levofloxacin, and that symptoms may occur soon after initiation of the drug and may be irreversible.1 2 8 Importance of immediately discontinuing levofloxacin and contacting a clinician if symptoms of peripheral neuropathy (e.g., pain, burning, tingling, numbness, and/or weakness) occur.1 2 8
-
Inform patients that systemic fluoroquinolones, including levofloxacin, have been associated with CNS effects (e.g., convulsions, dizziness, lightheadedness, increased intracranial pressure).1 2 8 Importance of informing clinician of any history of convulsions before initiating therapy with the drug.1 2 8 Importance of contacting a clinician if persistent headache with or without blurred vision occurs.1 2 8
-
Advise patients that levofloxacin may cause dizziness and lightheadedness;1 2 8 caution patients not to engage in activities requiring mental alertness and motor coordination (e.g., driving a vehicle, operating machinery) until effects of the drug on the individual are known.1 2 8
-
Advise patients that systemic fluoroquinolones, including levofloxacin, may worsen myasthenia gravis symptoms;1 2 8 importance of informing clinician of any history of myasthenia gravis.1 2 8 Importance of immediately contacting a clinician if any symptoms of muscle weakness, including respiratory difficulties, occur.1 2 8
-
Inform patients that levofloxacin may be associated with hypersensitivity reactions (including anaphylactic reactions), even after first dose.1 2 8 Importance of immediately discontinuing levofloxacin and contacting a clinician at first sign of rash or any symptom of hypersensitivity (e.g., hives, other skin reaction, rapid heartbeat, difficulty swallowing or breathing, throat tightness, hoarseness, swelling of lips, tongue, or face).1 2 8
-
Inform patients that photosensitivity/phototoxicity reactions reported following exposure to sun or UV light in patients receiving fluoroquinolones.1 2 8 Importance of avoiding or minimizing exposure to sunlight or artificial UV light (e.g., tanning beds, UVA/UVB treatment) and using protective measures (e.g., wearing loose-fitting clothes, sunscreen) if outdoors during levofloxacin therapy.1 2 8 Importance of discontinuing levofloxacin and contacting a clinician if a sunburn-like reaction or skin eruption occurs.1 2 8
-
Inform patients that severe hepatotoxicity (including acute hepatitis and fatal events) reported in patients receiving levofloxacin.1 2 8 Importance of immediately discontinuing levofloxacin and informing a clinician if any signs or symptoms of liver injury (e.g., loss of appetite, nausea, vomiting, fever, weakness, tiredness, right upper quadrant tenderness, itching, yellowing of the skin and eyes, light colored bowel movements, dark colored urine) occur.1 2 8
-
Importance of informing clinician of personal or family history of QT interval prolongation or proarrhythmic conditions (e.g., recent hypokalemia, bradycardia, recent myocardial ischemia) and of concurrent therapy with any drugs that may affect QT interval (e.g., class IA [quinidine, procainamide] or class III [e.g., amiodarone, sotalol] antiarrhythmic agents).1 2 8 Importance of contacting a clinician if symptoms of prolonged QT interval (e.g., prolonged heart palpitations, loss of consciousness) occur.1 2 8
-
Inform patients that systemic fluoroquinolones may increase risk of aortic aneurysm and dissection;172 importance of informing clinician of any history of aneurysms, blockages or hardening of the arteries, high blood pressure, or genetic conditions such as Marfan syndrome or Ehlers-Danlos syndrome.172 Advise patients to seek immediate medical treatment if they experience sudden, severe, and constant pain in the stomach, chest, or back.1 2 8 172
-
Inform patients that hypoglycemia reported when systemic fluoroquinolones were used in some patients receiving antidiabetic agents.171 Advise patients with diabetes mellitus receiving insulin or oral antidiabetic agents to discontinue levofloxacin and contacting a clinician if they experience hypoglycemia or symptoms of hypoglycemia.1 2 8
-
Advise patients that diarrhea is a common problem caused by anti-infectives and usually ends when the drug is discontinued.1 2 8 Importance of contacting a clinician if watery and bloody stools (with or without stomach cramps and fever) occur during or as late as 2 months or longer after the last dose.1 2 8
-
If considering levofloxacin for a pediatric patient (see Pediatric Use under Cautions), importance of parent informing clinician if the child has a history of joint-related problems.1 2 8 Importance of parent contacting a clinician if the child develops any joint-related problems during or following levofloxacin therapy.1 2 8
-
Advise patients receiving levofloxacin for inhalational anthrax (postexposure) or for treatment or prophylaxis of plague that human efficacy studies have not been performed for ethical and feasibility reasons; use in these conditions based on animal efficacy studies.1 2 8
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs (e.g., drugs that may affect QT interval, antidiabetic agents, warfarin), as well as any concomitant illnesses.1 2 8
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 2 8
-
Importance of advising patients of other important precautionary information.1 2 8 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
125 mg/5 mL* |
levoFLOXacin Solution |
|
|
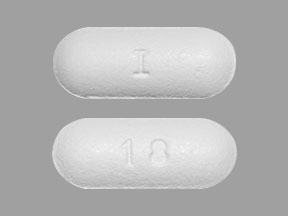
Tablets, film-coated |
250 mg (of anhydrous levofloxacin)* |
Levaquin |
Janssen |
|
|
levoFLOXacin Tablets |
||||
|
500 mg (of anhydrous levofloxacin)* |
Levaquin |
Janssen |
||
|
levoFLOXacin Tablets |
||||
|
750 mg (of anhydrous levofloxacin)* |
Levaquin |
Janssen |
||
|
levoFLOXacin Tablets |
||||
|
Parenteral |
For injection, concentrate, for IV infusion |
equivalent to levofloxacin 25 mg/mL (500 mg)* |
levoFLOXacin Concentrate, for IV Infusion |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for IV infusion |
equivalent to levofloxacin 5 mg/mL (250, 500, or 750 mg) in 5% Dextrose* |
levoFLOXacin in Dextrose Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Janssen Pharmaceuticals Inc. Levaquin (levofloxacin) tablets, film coated prescribing information. Titusville, NJ; 2019 May.
2. Baxter Healthcare Corporation. Levofloxacin injection, solution prescribing information. Deerfield, IL; 2019 Mar.
3. Davis R, Bryson HM. Levofloxacin: a review of its antibacterial activity, pharmacokinetics and therapeutic efficacy. Drugs. 1994; 47:677-700. https://pubmed.ncbi.nlm.nih.gov/7516863
4. Zhanel GC, Ennis K, Vercaigne L et al. A critical review of the fluoroquinolones: focus on respiratory tract infections. Drugs. 2002. 62:13-59.
5. Fish DN, Chow AT. The clinical pharmacokinetics of levofloxacin. Clin Pharmacokinet. 1997; 32:101-19. https://pubmed.ncbi.nlm.nih.gov/9068926
6. Williams NA, Bornstein M, Johnson K. Stability of levofloxacin in intravenous solutions in polyvinyl chloride bags. Am J Health-Syst Pharm. 1996; 53:2309-13. https://pubmed.ncbi.nlm.nih.gov/8893070
7. Shiba K, Sakai O, Shimada J et al. Effects of antacids, ferrous sulfate, and ranitidine on absorption of DR-3355 in humans. Antimicrob Agents Chemother. 1992; 36:2270-4. https://pubmed.ncbi.nlm.nih.gov/1444308 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245488/
8. Hi-Tech Pharmacal Co., Inc. Levofloxacin oral solution prescribing information. Amityville, NY; 2019 Mar.
9. Christ W, Lehnert T, Ulbrich B. Specific toxicologic aspects of the quinolones. Rev Infect Dis. 1988; 10(Suppl 1):S141-6. https://pubmed.ncbi.nlm.nih.gov/3279489
10. Reviewer’s comments (personal observations) on ciprofloxacin 8:12.18.
12. Une T, Fujimoto T, Sato K et al. In vitro activity of DR-3355, an optically active ofloxacin. Antimicrob Agents Chemother. 1988; 32:1336-40. https://pubmed.ncbi.nlm.nih.gov/3195996 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC175863/
13. Plouffe JF and the Franklin County Pneumonia Study Group. Levofloxacin in vitro activity against bacteremic isolates of Streptococcus pneumoniae. Diagn Microbiol Infect Dis. 1996; 25:43-5. https://pubmed.ncbi.nlm.nih.gov/8831044
14. Goa KL, Bryson HM, Markham A. Sparfloxacin: a review of its antibacterial activity, pharmacokinetic properties, clinical efficacy and tolerability in lower respiratory tract infections. Drugs. 1997; 53:700-25. https://pubmed.ncbi.nlm.nih.gov/9098667
15. Hecht DW, Wexler HM. In vitro susceptibility of anaerobes to quinolones in the United States. Clin Infect Dis. 1996; 23(Suppl 1):S2-8.
16. Eliopoulos GM. In vitro activity of fluoroquinolones against gram-positive bacteria. Drugs. 1995; 49(Suppl 2):48-57. https://pubmed.ncbi.nlm.nih.gov/8549407
17. Hooper DC. Quinolones. In: Mandell GL, Bennett JE, Dolin R eds. Mandell, Douglas and Bennett’s principles and practice of infectious diseases. 4th ed. New York: Churchill Livingstone; 1995:366-7.
18. Adeglass J, DeAbate AC, McElvaine P et al. Comparison of the effectiveness of levofloxacin and amoxicillin-clavulanate for the treatment of acute sinusitis in adults. Otolaryngol Head Neck Surg. 1999; 120:320-7. https://pubmed.ncbi.nlm.nih.gov/10064632
19. DeAbate CA, Russell M, McElvaine P et al. Safety and efficacy of oral levofloxacin versus cefuroxime axetil in acute bacterial exacerbation of chronic bronchitis. Respir Care. 1997; 42:206-13.
20. Habib MP, Gentry LO, Rodriguez-Gomez G et al. A multicenter, randomized study comparing the efficacy and safety of oral levofloxacin vs cefaclor in the treatment of acute bacterial exacerbations of chronic bronchitis. Proceedings of ICAAC New Orleans 1996. Abstract L002.
21. File TM Jr, Segreti J, Dunbar L et al. A multicenter, randomized study comparing the efficacy and safety of intravenous and/or oral levofloxacin vs ceftriaxone and/or cefuroxime axetil in the treatment of adults with community-acquired pneumonia. Antimicrob Agents Chemother. 1997; 41:1965-72. https://pubmed.ncbi.nlm.nih.gov/9303395 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164046/
23. Nicodemo AC, Robledo JA, Jasovich A et al. A multicenter, double-blind, randomized study comparing the efficacy and safety of oral levofloxacin versus ciprofloxacin in the treatment of uncomplicated skin and skin structure infections. Int J Clin Pract. 1998; 52:69-74. https://pubmed.ncbi.nlm.nih.gov/9624783
24. Richard GA, Klimberg IN, Fowler CL et al. Levofloxacin versus ciprofloxacin versus lomefloxacin in acute pyelonephritis. Urology. 1998; 52:51-5. https://pubmed.ncbi.nlm.nih.gov/9671870
25. Richard GA, Childs S, Fowler C et al. A comparison of levofloxacin (LVFX) and ciprofloxacin (cipro) for the treatment of complicated urinary tract infections (cUTI). Clin Infect Dis. 1996; 23:914.
27. Nichols R, Smith J, Gentry LO et al. Multicenter, open-label, active-controlled, randomized comparison of levofloxacin (LVFX) QD vs. ciprofloxacin (CIP) BID in 469 adults with mild-to-moderate skin and skin structure infections. Clin Infect Dis. 1996; 23:913.
32. Heffelfinger JD, Dowell SF, Jorgensen JH et al. Management of community-acquired pneumonia in the era of pneumococcal resistance: a report from the drug-resistance streptococcus pneumoniae therapeutic working group. Arch Intern Med. 2000; 160:1399-1408. https://pubmed.ncbi.nlm.nih.gov/10826451
37. Morganroth J, DiMarco JP, Anzueto A et al. A randomized trial comparing the cardiac rhythm safety of moxifloxacin vs levofloxacin in elderly patients hospitalized with community-acquired pneumonia. Chest. 2005; 128:3398-406. https://pubmed.ncbi.nlm.nih.gov/16304291
38. Bishai W. Current issues on resistance, treatment guidelines, and the appropriate use of fluoroquinolones for respiratory tract infections. Clin Ther. 2002; 24:838-50. https://pubmed.ncbi.nlm.nih.gov/12117077
39. Bearden DT, Danziger LH. Mechanism of action of and resistance to quinolones. Pharmacotherapy. 2001; 21:224S-32S. https://pubmed.ncbi.nlm.nih.gov/11642689
40. Tomioka H, Sato K, Akaki T et al. Comparative in vitro antimicrobial activities of the newly synthesized quinolone HSR-903, sitafloxacin (DU-6859s), gatifloxacin (AM-1155), and levofloxacin against Mycobacterium tuberculosis and Mycobacterium avium complex. Antimicrob Agents Chemother. 1999; 43:3001-4. https://pubmed.ncbi.nlm.nih.gov/10582897 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC89602/
41. Alvirez-Freites EJ, Carter JL, Cynamon MH. In vitro and in vivo activities of gatifloxacin against Mycobacterium tuberculosis. 2002; 46:1022-5.
42. Yang SC, Hsueh PR, Lai HC et al. High prevalence of antimicrobial resistance in rapidly growing mycobacteria in Taiwan. Antimicrob Agents Chemother. 2003; 47:1958-62. https://pubmed.ncbi.nlm.nih.gov/12760874 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC155839/
44. Zhanel GG, Palatnick L, Nichol KA et al. Antimicrobial resistance in respiratory tract Streptococcus pneumoniae isolates: results of the Canadian respiratory organism susceptibility study, 1997 to 2002. Antimicrob Agents Chemother. 2003; 47:1867-74. https://pubmed.ncbi.nlm.nih.gov/12760860 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC155828/
45. Kays MB, Smith DW, Wack ME et al. Levofloxacin treatment failure in a patient with fluoroquinolone-resistant Streptococcus pneumoniae pneumonia. Pharmacotherapy. 2002; 22:395-9. https://pubmed.ncbi.nlm.nih.gov/11898897
46. Graham DR, Talan DA, Nichols RL et al. Once-daily, high-dose levofloxacin versus ticarcillin-clavulanate alone or followed by amoxicillin-clavulanate for complicated skin and skin-structure infections: a randomized, open-label trial. Clin Infect Dis. 2002; 35:381-9. https://pubmed.ncbi.nlm.nih.gov/12145720
50. Frean JA, Arntzen L, Capper T et al. In vitro activities of 14 antibiotics against 100 human isolates of Yersinia pestis from a Southern African plague focus. Antimicrob Agents Chemother. 1996; 40:2646-7. https://pubmed.ncbi.nlm.nih.gov/8913481 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC163592/
53. Centers for Disease Control and Prevention. Increases in fluoroquinolone-resistant Neisseria gonorrhoeae among men who have sex with men—United States, 2003, and revised recommendations for gonorrhea treatment, 2004. MMWR Morb Mortal Wkly Rep. 2004; 53:3235-8.
58. Graham DR, Talan DA, Nichols RL et al. Once-daily, high-dose levofloxacin versus ticarcillin-clavulanate alone or followed by amoxicillin-clavulanate for complicated skin and skin-structure infections: a randomized, open-label trial. Clin Infect Dis. 2002; 35:381-9. https://pubmed.ncbi.nlm.nih.gov/12145720
64. Scotton PG, Pea F, Giobbia M et al. Cerebrospinal fluid penetration of levofloxacin in patients with spontaneous acute bacterial meningitis. Clin Infect Dis. 2001; 33:e109-11. https://pubmed.ncbi.nlm.nih.gov/11577376
65. Pea F, Pavan F, Nascimben E et al. Levofloxacin disposition in cerebrospinal fluid in patients with external ventriculostomy. Antimicrob Agents Chemother. 2003; 47:3104-8. https://pubmed.ncbi.nlm.nih.gov/14506016 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC201115/
66. Scotton PG, Tonon E, Giobbia M et al. Rhodococcus equi nosocomial meningitis cured by levofloxacin and shunt removal. Clin Infect Dis. 2000; 30:223-4. https://pubmed.ncbi.nlm.nih.gov/10619769
67. Nau R, Schmidt T, Kaye K et al. Quinolone antibiotics in therapy of experimental pneumococcal meningitis in rabbits. Antimicrob Agents Chemother. 1995; 39:593-7. https://pubmed.ncbi.nlm.nih.gov/7793857 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC162589/
68. Kuhn F, Cottagnoud M, Acosta F et al. Cefotaxime acts synergistically with levofloxacin in experimental meningitis due to penicillin-resistant pneumococci and prevents selection of levofloxacin-resistant mutants in vitro. Antimicrob Agents Chemother. 2003; 47:2487-91. https://pubmed.ncbi.nlm.nih.gov/12878509 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC166100/
69. Cottagnoud P, Cottagnoud M, Acosta F et al. Meropenem prevents levofloxacin-induced resistance in penicillin-resistant pneumococci and acts synergistically with levofloxacin in experimental meningitis. Eur J Clin Microbiol Infect Dis. 2003; 22:656-62. https://pubmed.ncbi.nlm.nih.gov/14557920
70. Granich RM, Oh P, Lewis B et al. Multidrug resistance among persons with tuberculosis in California, 1994-2003. JAMA. 2005; 293:2732-9. https://pubmed.ncbi.nlm.nih.gov/15941802
71. World Health Organization. Extensively drug-resistant tuberculosis (XDR-TB): recommendations for prevention and control. Wkly Epidemiol Rec. 2006; 45:430-2.
72. Gandhi NR, Moll A, Sturm AW et al. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006; 368:1575-80. https://pubmed.ncbi.nlm.nih.gov/17084757
73. Johnson JL, Hadad DJ, Boom WH et al. Early and extended early bactericidal activity of levofloxacin, gatifloxacin and moxifloxacin in pulmonary tuberculosis. Int J Tuberc Lung Dis. 2006; 10:605-12. https://pubmed.ncbi.nlm.nih.gov/16776446
74. Aubry A, Veziris N, Cambau E et al. Novel gyrase mutations in quinolone-resistant and -hypersusceptible clinical isolates of Mycobacterium tuberculosis: functional analysis of mutant enzymes. Antimicrob Agents Chemother. 2006; 50:104-12. https://pubmed.ncbi.nlm.nih.gov/16377674 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1346799/
75. Huang TS, Kunin CM, Lee SS et al. Trends in fluoroquinolone resistance of Mycobacterium tuberculosis complex in a Taiwanese medical centre: 1995-2003. J Antimicrob Chemother. 2005; 56:1058-62. https://pubmed.ncbi.nlm.nih.gov/16204341
76. Yew WW, Chan CK, Leung CC et al. Comparative roles of levofloxacin and ofloxacin in the treatment of multidrug-resistant tuberculosis. Chest. 2003; 124:1476-81. https://pubmed.ncbi.nlm.nih.gov/14555582
77. Marra F, Marra CA, Moadebi S et al. Levofloxacin treatment of active tuberculosis and the risk of adverse events. Chest. 2005; 128:1406-13. https://pubmed.ncbi.nlm.nih.gov/16162736
78. Ziganshina LE, Vizel AA, Squire SB. Fluoroquinolones for treating tuberculosis. Cocrane Database Syst Rev. 2005; Jul 20:CD004795.
79. El-Sadr WM, Perlman DC, Matts JP et al. Evaluation of an intensive intermittent-induction regimen and duration of short-course treatment for human immunodeficiency virus-related pulmonary tuberculosis. Clin Infect Dis. 1998; 26:1148-58.
80. Cahill JB, Bailey EM, Chien S et al. Levofloxacin secretion in breast milk: a case report. Pharmacotherapy; 2005; 25:116-8.
81. Flatz L, Cottagnoud M, Kuhn F et al. Ceftriaxone acts synergistically with levofloxacin in experimental meningitis and reduces levofloxacin-induced resistance in penicillin-resistant pneumococci. J Antimicrob Chemother. 2004; 53:305-10. https://pubmed.ncbi.nlm.nih.gov/14729741
82. Friedrich LV, Dougherty R. Fatal hypoglycemia associated with levofloxacin. Pharmacotherapy; 2004; 24:1807-12.
83. Chien SC, Rogge MC, Williams RR et al. Absence of a pharmacokinetic interaction between digoxin and levofloxacin. J Clin Pharm Ther. 2002; 27:7-12. https://pubmed.ncbi.nlm.nih.gov/11846857
84. Bauer LA, Black DJ, Lill JS et al. Levofloxacin and ciprofloxacin decrease procainamide and N-acetylprocainamide renal clearances. Antimicrob Agents Chemother. 2005; 49:1649-51. https://pubmed.ncbi.nlm.nih.gov/15793163 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1068590/
85. Nykamp DL, Blackmon CL, Schmidt PE et al. QTc prolongation associated with combination therapy of levofloxacin, imipramine, and fluoxetine. Ann Pharmacother. 2005; 39:543-6. https://pubmed.ncbi.nlm.nih.gov/15687478
86. Lee LJ, Hafkin B, Lee ID et al. Effects of food and sucralfate on a single oral dose of 500 milligrams of levofloxacin in healthy subjects. Antimicrob Agents Chemother. 1997; 41:2196-200. https://pubmed.ncbi.nlm.nih.gov/9333047 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164092/
87. Amsden GW, Whitaker AM, Johnson PW. Lack of bioequivalence of levofloxacin when coadministered with a mineral-fortified breakfast of juice and cereal. J Clin Pharmacol. 2003; 43:990-5. https://pubmed.ncbi.nlm.nih.gov/12971031
88. Wallace AW, Victory JM, Amsden GW. Lack of bioequivalence when levofloxacin and calcium-fortified orange juice are coadministered to healthy volunteers. J Clin Pharmacol. 2003; 43:539-44. https://pubmed.ncbi.nlm.nih.gov/12751275
89. Wright DH, Pietz SL, Konstantinides FN et al. Decreased in vitro fluoroquinolone concentrations after admixture with an enteral feeding formulation. J Parenter Enteral Nutr. 2000; 24:42-8.
90. Poole M, Anon J, Paglia M et al. A trial of high-dose, short-course levofloxacin for the treatment of acute bacterial sinusitis. Otolaryngol Head Neck Surg. 2006; 134:10-7. https://pubmed.ncbi.nlm.nih.gov/16399173
91. Hori S, Kizu J, Kawamura M. Effects of anti-inflammatory drugs on convulsant activity of quinolones: a comparative study of drug interactions between quinolones and anti-inflammatory drugs. J Infect Chemother. 2003; 9:314-20. https://pubmed.ncbi.nlm.nih.gov/14691652
92. Federico S, Carrano R, Capone D et al. Pharmacokinetic interaction between levofloxacin and ciclosporin or tacrolimus in kidney transplant recipients: ciclosporin, tacrolimus and levofloxacin in renal transplantation. Clin Pharmacokinet. 2006; 45:169-75. https://pubmed.ncbi.nlm.nih.gov/16485913
93. Kao LM, Bush K, Barnewall R et al. Pharmacokinetic considerations and efficacy of levofloxacin in an inhalational anthrax (postexposure) rhesus monkey model. Antimicrob Agents Chemother. 2006; 50:3535-42. https://pubmed.ncbi.nlm.nih.gov/17065619 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1635218/
94. Pai MP, Allen SE, Amsden GW. Altered steady state pharmacokinetics of levofloxacin in adult cystic fibrosis patients receiving calcium carbonate. J Cyst Fibros. 2006; 5:153-7. https://pubmed.ncbi.nlm.nih.gov/16481224
95. Anzueto A, Niederman MS, Pearle J et al. Community-acquired pneumonia recovery in the elderly (CAPRIE): efficacy and safety of moxifloxacin therapy versus that of levofloxacin therapy. Clin Infect Dis. 2006; 42:73-81. https://pubmed.ncbi.nlm.nih.gov/16323095
101. McDonald LC, Killgore GE, Thompson A et al. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med. 2005; 353:2433-41. https://pubmed.ncbi.nlm.nih.gov/16322603
102. Loo VG, Poirier L, Miller MA et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med. 2005; 353:2442-9. https://pubmed.ncbi.nlm.nih.gov/16322602
103. McDonald LC, Owings M, Jernigan DB. Clostridium difficile infection in patients discharged from US short-stay hospitals, 1996-2003. Emerg Infect Dis. 2006; 12:409-15. https://pubmed.ncbi.nlm.nih.gov/16704777 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3291455/
104. Bartlett JG, Peri TM. The new Clostridium difficile–what does it mean? N Engl J Med. 2005; 353:2503-5.
105. Centers for Disease Control and Prevention. Severe Clostridium difficile-associated disease in populations previously at low risk–four states, 2005. MMWR Morb Mortal Wkly Rep. 2005; 54:1201-5.
106. Kazakova SV, Ware K, Baughman B et al. A hospital outbreak of diarrhea due to an emerging epidemic strains of Clostridium difficile. Arch Intern Med. 2006; 166:2518-24. https://pubmed.ncbi.nlm.nih.gov/17159019
107. Dhalla IA, Mamdani MM, Simor AE et al. Are broad-spectrum fluoroquinolones more likely to cause Clostridium difficile-associated disease? Antimicrob Agents Chemother. 2006; 50:3216-9.
109. Knapp JS, Ohye R, Neal SW et al. Emerging in vitro resistance to quinolones in penicillinase-producing Neisseria gonorrhoeae strains in Hawaii. Antimicrob Agents Chemother. 1994; 38:2200-3. https://pubmed.ncbi.nlm.nih.gov/7811047 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC284712/
110. Bradley JS, Jackson MA, Committee on Infectious Diseases et al. The use of systemic and topical fluoroquinolones. Pediatrics. 2011; 128:e1034-45.
111. Ruiz-Serrano MJ, Alcala L, Martinez L et al. In vitro activities of six fluoroquinolones against 250 clinical isolates of Mycobacterium tuberculosis susceptible or resistant to first-line antituberculosis drugs. Antimicrob Agents Chemother. 2000; 44:2567-8.
112. Kam KM, Yip CW, Cheung TL et al. Stepwise decrease in moxifloxacin susceptibility amongst clinical isolates of multidrug-resistant Mycobacterium tuberculosis: correlation with ofloxacin susceptibility. Microb Drug Resist. 2006; 12:7-11. https://pubmed.ncbi.nlm.nih.gov/16584301
113. Shandil RK, Jayaram R, Kaur P et al. Moxifloxacin, ofloxacin, sparfloxacin, and ciprofloxacin against Mycobacterium tuberculosis: evaluation of in vitro and pharmacodynamic indices that best predict in vivo efficacy. Antimicrob Agents Chemother. 2007; 51:576-82. https://pubmed.ncbi.nlm.nih.gov/17145798
114. . Update to CDC’s sexually transmitted diseases treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb Mortal Wkly Rep. 2007; 56:332-6. https://pubmed.ncbi.nlm.nih.gov/17431378
116. Douglas JM Jr. Dear colleague letter: Fluoroquinolones are no longer recommended for the treatment of gonorrhea in the United States. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, Department of Health & Human Services; 2007 April 12.
117. Ball P. Long-term use of quinolones and their safety. Rev Infect Dis. 1989; 11(Suppl 5):S1365-9. https://pubmed.ncbi.nlm.nih.gov/2672258
118. Davis GJ, McKenzie ME. Toxicologic evaluation of ofloxacin. Am J Med. 1989; 87(Suppl 6C):43S-46S. https://pubmed.ncbi.nlm.nih.gov/2690619
119. Mayer DG. Overview of toxicological studies. Drugs. 1987; 34(Suppl 1):150-3. https://pubmed.ncbi.nlm.nih.gov/3325258
120. Kato M, Onodera T. Morphological investigation of cavity formation in articular cartilage induced by ofloxacin in rats. Fund Appl Toxicol. 1988; 11:110-9.
121. Hooper DC, Wolfson JS. Fluoroquinolone antimicrobial agents. N Engl J Med. 1991; 324:384-94. https://pubmed.ncbi.nlm.nih.gov/1987461
122. Paton JH, Reeves DS. Fluoroquinolone antibiotics: microbiology, pharmacokinetics and clinical uses. Drugs. 1988; 36:193-228. https://pubmed.ncbi.nlm.nih.gov/3053126
123. Maggiolo F, Caprioli S, Suter F. Risk/benefit analysis of quinolone use in children: the effect on diarthrodial joints. J Antimicrob Chemother. 1990; 26:469-71. https://pubmed.ncbi.nlm.nih.gov/2254219
124. Pfister K, Mazur D, Vormann J et al. Diminished ciprofloxacin-induced chondrotoxicity by supplementation with magnesium and vitamin E in immature rats. Antimicrob Agents Chemother. 2007; 51:1022-7. https://pubmed.ncbi.nlm.nih.gov/17210779 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1803142/
125. Stahlmann R. Safety profile of the quinolones. J Antimicrob Chemother. 1990; 26(Suppl D):31-44. https://pubmed.ncbi.nlm.nih.gov/2286589
126. Christ W, Lehnert T, Ulbrich B. Specific toxicologic aspects of the quinolones. Rev Infect Dis. 1988; 10(Suppl 1):S141-6. https://pubmed.ncbi.nlm.nih.gov/3279489
128. US Food and Drug Administration. FDA news. FDA requests boxed warnings on fluoroquinolone antimicrobial drugs. 2008 Jul 8. From FDA website. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116919.htm
129. US Food and Drug Administration. Information for healthcare professionals: Fluoroquinolone antimicrobial drugs. 2008 Jul 8. From FDA website. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm126085.htm
130. US Food and Drug Administration. FDA drug safety communication: FDA requires label changes to warn of risk for possibly permanent nerve damage from antibacterial fluoroquinolone drugs taken by mouth or by injection. 2013 Aug 15. From FDA website. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM365078.pdf
132. Knapp JS, Washington JA, Doyle LJ et al. Persistence of Neisseria gonorrhoeae strains with decreased susceptibility to ciprofloxacin and ofloxacin in Cleveland, Ohio, from 1992 through 1993. Antimicrob Agents Chemother. 1994; 38:2194-6. https://pubmed.ncbi.nlm.nih.gov/7811045 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC284710/
140. US Food and Drug Administration. FDA drug safety communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections; warns about disabling side effects that can occur together. Silver Spring, MD; 2016 May 12. From FDA website. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM500591.pdf
143. Gupta K, Hooton TM, Naber KG et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011; 52:e103-20. Updates may be available at IDSA website at www.idsociety.org. https://pubmed.ncbi.nlm.nih.gov/21292654
145. US Food and Drug Administration. FDA drug safety communication: FDA updates warnings for oral and injectable fluoroquinolone antibiotics due to disabling side effects. Silver Spring, MD; 2016 Jul 26. From FDA website. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM513019.pdf
171. US Food and Drug Administration. FDA drug safety communication: FDA reinforces safety information about serious low blood sugar levels and mental health side effects with fluoroquinolone antibiotics; requires label changes. Silver Spring, MD; 2018 Jul 10. From FDA website. https://www.fda.gov/media/114192/download
172. US Food and Drug Administration. FDA drug safety communication: FDA warns about increased risk of ruptures or tears in the aorta blood vessel with fluoroquinolone antibiotics in certain patients. Silver Spring, MD; 2018 Dec 12. From FDA website. https://www.fda.gov/media/119532/download
197. Anon. Drugs for bacterial infections. Treat Guidel Med Lett. 2010; 8:43-52. https://pubmed.ncbi.nlm.nih.gov/20489679
218. Nahid P, Dorman SE, Alipanah N et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Clin Infect Dis. 2016; :.
231. World Health Organization. Treatment of tuberculosis guidelines. 4th ed. World Health Organization; 2010. From WHO website. http://apps.who.int/iris/bitstream/10665/44165/1/9789241547833_eng.pdf
235. Chey WD, Leontiadis GI, Howden CW et al. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am J Gastroenterol. 2017; 112:212-239. https://pubmed.ncbi.nlm.nih.gov/28071659
236. Sebghatollahi V, Soheilipour M, Khodadoostan M et al. Levofloxacin-containing versus Clarithromycin-containing Therapy for Helicobacter pylori Eradication: A Prospective Randomized Controlled Clinical Trial. Adv Biomed Res. 2018; 7:55. https://pubmed.ncbi.nlm.nih.gov/29657940
237. Hsu PI, Tsai FW, Kao SS et al. Ten-Day Quadruple Therapy Comprising Proton Pump Inhibitor, Bismuth, Tetracycline, and Levofloxacin is More Effective than Standard Levofloxacin Triple Therapy in the Second-Line Treatment of Helicobacter pylori Infection: A Randomized Controlled Trial. Am J Gastroenterol. 2017; 112:1374-1381. https://pubmed.ncbi.nlm.nih.gov/28719592
239. Zerbetto De Palma G, Mendiondo N, Wonaga A et al. Occurrence of Mutations in the Antimicrobial Target Genes Related to Levofloxacin, Clarithromycin, and Amoxicillin Resistance in Helicobacter pylori Isolates from Buenos Aires City. Microb Drug Resist. 2017; 23:351-358. https://pubmed.ncbi.nlm.nih.gov/27391421
240. Shao Y, Lu R, Yang Y et al. Antibiotic resistance of Helicobacter pylori to 16 antibiotics in clinical patients. J Clin Lab Anal. 2018; 32:e22339. https://pubmed.ncbi.nlm.nih.gov/28984385
241. Cheng A, Sheng WH, Liou JM et al. Comparative in vitro antimicrobial susceptibility and synergistic activity of antimicrobial combinations against Helicobacter pylori isolates in Taiwan. J Microbiol Immunol Infect. 2015; 48:72-9. https://pubmed.ncbi.nlm.nih.gov/23036269
276. World Health Organization. WHO treatment guidelines for drug-resistant tuberculosis: 2016 update. From WHO website. http://www.who.int
292. American Academy of Pediatrics. Red Book: 2018–2021 Report of the Committee on Infectious Diseases. 31st ed. Itasca, IL: American Academy of Pediatrics; 2018.
293. Jackson MA, Schutze GE, Committee on Infectious Diseases. The Use of Systemic and Topical Fluoroquinolones. Pediatrics. 2016; 138 https://pubmed.ncbi.nlm.nih.gov/27940800
302. McDonald LC, Gerding DN, Johnson S et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018; 66:987-994. https://pubmed.ncbi.nlm.nih.gov/29562266
303. Fekety R for the American College of Gastroenterology Practice Parameters Committee. Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis. Am J Gastroenterol. 1997; 92:739-50. https://pubmed.ncbi.nlm.nih.gov/9149180
304. American Society of Health-System Pharmacists Commission on Therapeutics. ASHP therapeutic position statement on the preferential use of metronidazole for the treatment of Clostridium difficile-associated disease. Am J Health-Syst Pharm. 1998; 55:1407-11. https://pubmed.ncbi.nlm.nih.gov/9659970
305. Anon. Advice for travelers. Med Lett Drugs Ther. 2015; 57:52-8. https://pubmed.ncbi.nlm.nih.gov/25853663
315. Kalil AC, Metersky ML, Klompas M et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016; 63:e61-e111. https://pubmed.ncbi.nlm.nih.gov/27418577
344. Workowski KA, Bolan GA. Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR Recomm Rep. 2015; 64(RR-03):1-137. https://pubmed.ncbi.nlm.nih.gov/26042815
418. Tunkel AR, Hartman BJ, Kaplan SL et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004; 39:1267-84. Updates may be available at IDSA website at www.idsociety.org. https://pubmed.ncbi.nlm.nih.gov/15494903
440. Panel on Opportunistic Infection in HIV-infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America (Accessed May 13, 2019). Updates may be available at HHS AIDS Information (AIDSinfo) website. http://www.aidsinfo.nih.gov
450. Baddour LM, Wilson WR, Bayer AS et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation. 2015; 132:1435-86. https://pubmed.ncbi.nlm.nih.gov/26373316
512. Mandell LA, Wunderink RG, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007; 44 Suppl 2:S27-72. Updates may be available at IDSA website at www.idsociety.org. https://pubmed.ncbi.nlm.nih.gov/17278083
525. Centers for Disease Control and Prevention. CDC health information for international travel, 2018. Atlanta, GA: US Department of Health and Human Services. Updates may be available at CDC website. https://wwwnc.cdc.gov/travel/page/yellowbook-home
543. Stevens DL, Bisno AL, Chambers HF et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin Infect Dis. 2014; 59:147-59. Updates may be available at IDSA website at www.idsociety.org. https://pubmed.ncbi.nlm.nih.gov/24947530
544. Lipsky BA, Berendt AR, Cornia PB et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012; 54:e132-73. Updates may be available at IDSA website at www.idsociety.org.
599. Centers for Disease Control and Prevention. Additional options for preventive treatment for persons exposed to inhalational anthrax. MMWR Morb Mortal Wkly Rep. 2001; 50:1142.
668. Inglesby TV, O’Toole T, Henderson DA et al for the Working Group on Civilian Biodefense. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA. 2002; 287:2236-52. https://pubmed.ncbi.nlm.nih.gov/11980524
671. Bradley JS, Peacock G, Krug SE et al. Pediatric anthrax clinical management. Pediatrics. 2014; 133:e1411-36. https://pubmed.ncbi.nlm.nih.gov/24777226
672. Meaney-Delman D, Zotti ME, Creanga AA et al. Special considerations for prophylaxis for and treatment of anthrax in pregnant and postpartum women. Emerg Infect Dis. 2014; 20:e1-6. https://pubmed.ncbi.nlm.nih.gov/24457117
673. Hendricks KA, Wright ME, Shadomy SV et al. Centers for disease control and prevention expert panel meetings on prevention and treatment of anthrax in adults. Emerg Infect Dis. 2014; 20 https://pubmed.ncbi.nlm.nih.gov/24447897
675. Griffith DE, Aksamit T, Brown-Elliott BA et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367-416. https://pubmed.ncbi.nlm.nih.gov/17277290
677. Caeiro JP, Dupont HL. Management of travelers’ diarrhoea. Drugs. 1998; 56:73-81. https://pubmed.ncbi.nlm.nih.gov/9664200
679. Adachi JA, Ostrosky-Zeichner L, DuPont HL et al. Empirical antimicrobial therapy for travelers’ diarrhea. Clin Infect Dis. 2000; 31:1079-83. https://pubmed.ncbi.nlm.nih.gov/11049792
681. Centers for Disease Control and Prevention. Diagnosis and management of foodborne illnesses: a primer for physicians. MMWR Recomm Rep. 2001; 50(RR-2):1-69.
683. US Army Medical Research Institute of Infectious Disease. USAMRIID’s medical management of biologic casualties handbook. 8th ed. USAMRIID: Fort Detrick, MD; 20141 Sep.
686. Centers for Disease Control and Prevention. Update: investigation of bioterrorism-related anthrax and interim guidelines for exposure management and antimicrobial therapy, October 2001. MMWR Morb Mortal Wkly Rep. 2001; 50:909-19. https://pubmed.ncbi.nlm.nih.gov/11699843
688. Inglesby TV, Dennis DT, Henderson DA et al for the Working Group on Civilian Biodefense. Plague as a biological weapon: medical and public health management. JAMA. 2000; 283:2281-90. https://pubmed.ncbi.nlm.nih.gov/10807389
710. Jernigan JA, Stephens DS, Ashford DA and the Anthrax Bioterrorism Investigation Team. Bioterrorism–related inhalation anthrax: the first 10 cases reported in the United States. Emerg Infect Dis. 2001; 7:933-44. https://pubmed.ncbi.nlm.nih.gov/11747719 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2631903/
767. Brookmeyer R, Johnson E, Bollinger R. Modeling the optimum duration of antibiotic prophylaxis in an anthrax outbreak. Proc Natl Acad Sci. 2003; 100:10129-32. https://pubmed.ncbi.nlm.nih.gov/12890865 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC187789/
857. Kirkcaldy RD, Harvey A, Papp JR et al. Neisseria gonorrhoeae Antimicrobial Susceptibility Surveillance - The Gonococcal Isolate Surveillance Project, 27 Sites, United States, 2014. MMWR Surveill Summ. 2016; 65:1-19. https://pubmed.ncbi.nlm.nih.gov/27414503
HID. ASHP’s interactive handbook on injectable drugs. McEvoy, GK, ed. Bethesda, MD: American Society of Health-System Pharmacists, Inc; Updated June 1, 2019. From HID website. http://www.interactivehandbook.com/
Related/similar drugs
Frequently asked questions
- What are the best antibiotics for pneumonia?
- What is the best antibiotic to treat a sinus infection?
- What antibiotics are used to treat UTI?
- Can Levaquin cause tendonitis?
More about levofloxacin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (746)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
Patient resources
Professional resources
- Levofloxacin prescribing information
- Levofloxacin Injection Concentrate (FDA)
- Levofloxacin Oral Solution (FDA)
- Levofloxacin Tablets (FDA)