Gemfibrozil (Monograph)
Brand name: Lopid
Drug class: Fibric Acid Derivatives
VA class: CV350
Chemical name: 5-(2,5-Dimethylphenoxy)-2,2-dimethylpentanoic acid
Molecular formula: C15H22O3
CAS number: 25812-30-0
Introduction
Antilipemic agent; fibric acid derivative.2
Uses for Gemfibrozil
Prevention of Cardiovascular Events
Adjunct to dietary therapy to reduce the risk of developing CHD in patients with type IIb hyperlipoproteinemia without clinical evidence of CHD (primary prevention) who have an inadequate response to dietary management, weight loss, exercise, and drugs known to reduce LDL-cholesterol and increase HDL-cholesterol (e.g., bile acid sequestrants, niacin) and who have low HDL-cholesterol concentrations in addition to elevated LDL-cholesterol and triglycerides.1 67 68 104 105 110 127
Potential benefit unlikely to outweigh potential risks in patients with type IIa hyperlipoproteinemia and elevations of LDL-cholesterol only (because of toxicity, including malignancy, gallbladder disease, abdominal pain leading to appendectomy and other abdominal surgeries, and increased incidence of noncardiovascular and all-cause mortality, associated with the chemically and pharmacologically similar drug clofibrate [no longer commercially available in US]).1
Manufacturer states that gemfibrozil is not indicated for use in the management of patients with low HDL-cholesterol as their only lipid abnormality (isolated low HDL-cholesterol).1
Reduction of recurrent coronary events† [off-label], including death from coronary causes, MI, and stroke in men with clinical evidence of CHD who have low HDL-cholesterol and moderately elevated LDL-cholesterol concentrations.137
AHA/ACC cholesterol management guideline states that lifestyle modification is the foundation of cardiovascular risk reduction.400 If pharmacologic therapy is needed, statins are first-line drugs of choice because of their demonstrated benefits in reducing risk of atherosclerotic cardiovascular disease (ASCVD).400 Nonstatin drugs may be considered as adjunctive therapy in certain high-risk patients, but other drugs (e.g., ezetimibe) are generally recommended.400 Although fibrates have mild LDL-lowering effects, randomized controlled studies do not support their use as add-on therapy to statins.400
If fibrate therapy is necessary in a statin-treated patient, AHA/ACC states that it is safer to use fenofibrate than gemfibrozil because of lower risk of severe myopathy.400
Dyslipidemias
Adjunct to dietary therapy in the management of severe hypertriglyceridemia in patients at risk of developing pancreatitis (typically those with serum triglyceride concentrations >2000 mg/dL and elevated concentrations of VLDL-cholesterol and fasting chylomicrons) who do not respond adequately to dietary management.1
Also may be used in patients with triglyceride concentrations of 1000–2000 mg/dL who have a history of pancreatitis or of recurrent abdominal pain typical of pancreatitis;1 however, efficacy in patients with type IV hyperlipoproteinemia and triglyceride concentrations >1000 mg/dL who exhibit type V patterns subsequent to dietary or alcoholic indiscretion has not been adequately studied.1
Manufacturer states that gemfibrozil is not indicated for use in patients with type I hyperlipoproteinemia who have elevated triglyceride and chylomicron concentrations but normal VLDL-cholesterol concentrations.1
Effective in a very limited number of patients with type III hyperlipoproteinemia† [off-label]17 18 37 38 43 45 49 to decrease elevated triglyceride and cholesterol concentrations associated with this disorder.
Gemfibrozil Dosage and Administration
General
-
Patients should be placed on a standard lipid-lowering diet before initiation of gemfibrozil therapy and should remain on this diet during treatment with the drug.1
Administration
Oral Administration
Administer orally twice daily, 30 minutes before the morning and evening meals.1
Dosage
Adults
Prevention of Cardiovascular Events
Oral
600 mg twice daily.1 16 17 18 21 22 24 25 26 27 30 31 91 104 106
Monitor lipoprotein concentrations periodically.1 Discontinue therapy in patients who fail to achieve an adequate response after 3 months of therapy.1
Dyslipidemias
Oral
600 mg twice daily.1 16 17 18 21 22 24 25 26 27 30 31 91 104 106
Monitor lipoprotein concentrations periodically.1 Discontinue therapy in patients who fail to achieve an adequate response after 3 months of therapy.1
Cautions for Gemfibrozil
Contraindications
-
Hepatic impairment, including primary biliary cirrhosis; severe renal impairment; or preexisting gallbladder disease.1
-
Known hypersensitivity to gemfibrozil or any ingredient in the formulation.1
Warnings/Precautions
Warnings
Cholelithiasis
May increase cholesterol excretion in bile,1 34 61 resulting in cholelithiasis.1 26 34 Cholecystitis and cholelithiasis reported.1 Discontinue therapy if gallbladder studies indicate the presence of gallstones.1
Musculoskeletal Effects
Use may be associated with myositis.1 Myalgia, myopathy, myasthenia, painful extremities, arthralgia, synovitis, and rhabdomyolysis reported.1 Myopathy, rhabdomyolysis, and other complications also reported in patients receiving gemfibrozil concomitantly with certain other antilipemic agents.1
Monitor creatine kinase (CK, creatine phosphokinase, CPK) concentrations in patients reporting adverse musculoskeletal effects.1 108 116 Discontinue therapy if myositis is suspected or diagnosed.1
Effect on Morbidity and Mortality
Effect on cardiovascular mortality not established.1 Because gemfibrozil is chemically, pharmacologically, and clinically similar to other fibric acid derivatives, some adverse effects of clofibrate (no longer commercially available in the US) such as increased incidence of cholelithiasis, cholecystitis requiring surgery, postcholecystectomy complications, malignancy, pancreatitis, appendectomy, gallbladder disease, and increased overall mortality may also apply to gemfibrozil,1 and the usual precautions associated with fibrate therapy should be observed.1
Cataracts
Possible subcapsular bilateral and unilateral cataracts.1
Sensitivity Reactions
Hypersensitivity Reactions
Angioedema, laryngeal edema, urticaria, rash, dermatitis, and pruritus reported.1
Major Toxicities
Hematologic Effects
Mild decreases in hemoglobin,1 2 hematocrit,1 2 38 and leukocyte counts1 2 reported; these counts usually normalize during long-term therapy.1 Severe anemia, leukopenia, thrombocytopenia, and bone marrow hypoplasia have occurred rarely; eosinophilia also reported.1
Monitor blood cell counts periodically during the first 12 months of therapy.1
General Precautions
Hepatic Effects
Possible elevations in serum concentrations of aminotransferase (i.e., AST, ALT),1 2 24 25 47 LDH,1 2 bilirubin,1 and alkaline phosphatase.1 2 15 25 47 Serum aminotransferase concentrations usually return slowly to pretreatment values following discontinuance of gemfibrozil.1 Cholestatic jaundice reported.1
Perform liver function tests periodically.1 Discontinue therapy if abnormalities persist.1
Carcinogenicity
Carcinogenicity (e.g., hepatic tumors, Leydig cell tumors) demonstrated in animals.1
Specific Populations
Pregnancy
Category C.1
Lactation
Not known if gemfibrozil is distributed into milk.1 102 Discontinue nursing or the drug.1
Pediatric Use
Safety and efficacy not established.1
Renal Impairment
Possible exacerbation of renal insufficiency in patients with baseline Scr >2 mg/dL.1 Consider use of alternative antilipemic therapy against the risks and benefits of a lower dose of gemfibrozil.1
Common Adverse Effects
GI disturbances (e.g., dyspepsia, abdominal pain, diarrhea, nausea, vomiting, constipation, acute appendicitis, gallbladder surgery), adverse CNS effects (headache, hypesthesia, paresthesias, dizziness, somnolence, peripheral neuritis, depression), fatigue, eczema, vertigo, taste perversion, blurred vision, decreased libido, impotence.1
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
β-Adrenergic blocking agents |
Possible increase in serum triglyceride and decreases in HDL-cholesterol concentrations30 74 |
|
|
Anticoagulants, oral (e.g., warfarin) |
Use with caution;1 reduce anticoagulant dosage to maintain PT at desired level to prevent bleeding complications; monitor PT frequently until stabilized1 |
|
|
Estrogens |
Potential increase in serum triglyceride concentrations73 |
|
|
HMG-CoA reductase inhibitors (statins) |
Increased risk of adverse musculoskeletal effects (e.g., myopathy, rhabdomyolysis)1 |
|
|
Methyldopa |
Possible decrease in HDL- and LDL-cholesterol concentrations74 |
|
|
Repaglinide |
Increased repaglinide concentrations and half-life, resulting in enhanced and prolonged blood glucose-lowering effects;138 139 potential for severe hypoglycemia138 |
Do not initiate repaglinide in patients receiving gemfibrozil, and vice versa138 139 Monitor blood glucose and reduce repaglinide dosage as required if drugs already used concomitantly138 Patients receiving gemfibrozil concomitantly with repaglinide should not receive itraconazole138 |
|
Thiazide diuretics |
Possible increase in total cholesterol and triglyceride concentrations74 |
Gemfibrozil Pharmacokinetics
Absorption
Bioavailability
Rapidly and completely absorbed from the GI tract.1 2 7 76
Peak plasma concentrations occur within 1–2 hours.1 2 7 9 Plasma concentrations do not appear to correlate with therapeutic response.29 102
Food
Rate and extent of absorption increased when administered 30 minutes before meals.1
Distribution
Extent
Highest tissue concentrations observed in the liver and kidneys in animals.2
Gemfibrozil crosses the placenta;2 not known if it is distributed into milk.1 102
Plasma Protein Binding
About 95%.2
Elimination
Metabolism
Appears to be metabolized in the liver to 4 major metabolites produced via 3 metabolic pathways.2 7 102 A phenol derivative (metabolite I)2 7 is pharmacologically active.102
Elimination Route
Excreted in urine (70%) in the form of metabolites and in feces (approximately 6%).1
Half-life
Stability
Storage
Oral
Tablets
20–25°C.1 Protect from light and humidity.1
Actions and Spectrum
-
Decreases serum concentrations of triglycerides,1 15 16 17 18 19 21 22 23 24 26 27 28 29 30 32 33 37 38 45 48 76 91 104 VLDL-cholesterol,1 15 17 18 19 25 33 37 38 45 48 76 and, to a lesser extent, LDL-cholesterol.1 15 33 37 38 45 76 Increases HDL-cholesterol.1 15 16 19 21 22 24 25 26 31 32 33 36 38 45 88 91 Causes a variable reduction in serum total cholesterol,1 15 16 17 18 19 21 24 25 26 27 28 29 30 31 32 33 37 38 48 68 105 106 because the decrease in serum cholesterol is a net result of a decrease in VLDL-cholesterol,18 19 21 25 26 28 32 33 38 45 an increase in HDL-cholesterol,37 68 and an increase15 21 30 33 37 45 91 or decrease in LDL-cholesterol.21 24 26 32 37 38 45
-
Generally increases LDL-cholesterol in patients with type IV or V hyperlipoproteinemia and decreases LDL-cholesterol in type IIa or IIb disorder.21 25 28 45 91
-
Inhibits lipolysis of fat in adipose tissue1 54 56 75 76 91 and decreases hepatic uptake of plasma free fatty acids1 54 75 76 (i.e., free fatty acid turnover is decreased),51 54 75 thereby reducing hepatic triglyceride production1 54 75 76 (triglyceride turnover rate is decreased).51 75 Also inhibits production1 15 54 75 91 and increases clearance1 75 102 of VLDL carrier apolipoprotein B (VLDL-apo B), leading to a decrease in VLDL production,1 15 45 54 75 enhanced clearance of VLDL,15 and, subsequently, a decrease in serum triglyceride concentrations.2 54 91
Advice to Patients
-
Importance of patients informing clinicians of any unexplained muscle pain, tenderness, or weakness.1
-
Importance of adhering to nondrug therapies and measures, including dietary management, weight control, physical activity, and management of potentially contributory disease (e.g., diabetes mellitus).1 64 67 70 133 136
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as concomitant illnesses.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
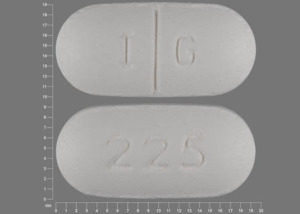
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
600 mg* |
Gemfibrozil Tablets |
|
|
Lopid |
Pfizer |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 26, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Parke-Davis. Lopid (gemfibrozil) tablets prescribing information. New York, NY; 2003 Oct.
2. Parke-Davis. Lopid (gemfibrozil) compendium of pharmacological and clinical studies. Morris Plains, NJ; 1982 Feb.
3. The United States pharmacopeia, 21st rev, and The national formulary, 16th ed. Rockville, MD: The United States Pharmacopeial Convention, Inc; 1985: 457.
4. Hodges RM. Gemfibrozil—a new lipid lowering agent. Proc R Soc Med. 1976; 69(Suppl 2):1-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864035/ https://pubmed.ncbi.nlm.nih.gov/798192
5. Creger PL, Moersch GW, Neuklis WA. Structure/activity relationship of gemfibrozil (CI-719) and related compounds. Proc R Soc Med. 1976; 69(Suppl 2):3-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864034/ https://pubmed.ncbi.nlm.nih.gov/1019152
6. Rodney G, Uhlendorf P, Maxwell RE. The hypolipidaemic effect of gemfibrozil (CI-719) in laboratory animals. Proc R Soc Med. 1976; 69(Suppl 2):6-10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864017/ https://pubmed.ncbi.nlm.nih.gov/828263
7. Okerholm RA, Keeley FJ, Peterson FE et al. The metabolism of gemfibrozil. Proc R Soc Med. 1976; 69(Suppl 2):11-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864041/ https://pubmed.ncbi.nlm.nih.gov/828261
8. Kurtz SM, Fitzgerald JE, Fisken RA et al. Toxicological studies on gemfibrozil. Proc R Soc Med. 1976; 69(Suppl 2):15-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864019/ https://pubmed.ncbi.nlm.nih.gov/828262
9. Smith TC. Toleration and bioavailability of gemfibrozil in healthy men. Proc R Soc Med. 1976; 69(Suppl 2):24-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864020/ https://pubmed.ncbi.nlm.nih.gov/798193
10. Randinitis EJ, Kinkel AW, Nelson C et al. Gas chromatographic determination of gemfibrozil and its metabolites in plasma and urine. J Chromatogr. 1984; 307:210-5. https://pubmed.ncbi.nlm.nih.gov/6586728
11. Gray RH, de la Iglesia FA. Quantitative microscopy comparison of peroxisome proliferation by the lipid-regulating agent gemfibrozil in several species. Hepatology. 1984; 4:520-30. https://pubmed.ncbi.nlm.nih.gov/6586630
12. de la Iglesia FA, Lewis JE, Buchanan RA et al. Light and electron microscopy of liver in hyperlipoproteinemic patients under long-term gemfibrozil treatment. Atherosclerosis. 1982; 43:19-37. https://pubmed.ncbi.nlm.nih.gov/6807326
13. Maxwell RE, Nawrocki JW, Uhlendorf PD. Some comparative effects of gemfibrozil, clofibrate, benzafibrate, cholestyramine, and compactin on sterol metabolism in rats. Atherosclerosis. 1983; 48:195-203. https://pubmed.ncbi.nlm.nih.gov/6579963
14. Kahonen MT, Ylikahri RH. Effect of clofibrate and gemfibrozil on the activities of mitochondrial carnitine acyltransferases in rat liver. Dose-response relations. Atherosclerosis. 1979; 32:47-56. https://pubmed.ncbi.nlm.nih.gov/465113
15. Kesaniemi YA, Grundy SM. Influence of gemfibrozil and clofibrate on metabolism of cholesterol and plasma triglycerides in man. JAMA. 1984; 251:2241-6. https://pubmed.ncbi.nlm.nih.gov/6368883
16. Kaukola S, Manninen V, Malkonen M et al. Gemfibrozil in the treatment of dyslipidaemias in middle-aged survivors of myocardial infarction. Acta Med Scand. 1981; 209:69-73. https://pubmed.ncbi.nlm.nih.gov/7010929
17. Konttinen A, Kuisma I, Ralli R et al. The effect of gemfibrozil on serum lipids in diabetic patients. Ann Clin Res. 1979; 11:240-5. https://pubmed.ncbi.nlm.nih.gov/398183
18. Hoogwerf BJ, Bantle JP, Kuba K et al. Treatment of type III hyperlipoproteinemia with four different treatment regimens. Atherosclerosis. 1984; 51:251-9. https://pubmed.ncbi.nlm.nih.gov/6588975
19. Nye ER, Sutherland NHF, Temples WA. The treatment of hyperlipoproteinemia with gemfibrozil compared with placebo and clofibrate. N Z Med J. 1980; 92:345-9. https://pubmed.ncbi.nlm.nih.gov/6935550
20. Nash DT. Gemfibrozil in combination with other drugs for severe hyperlipidemia: preliminary study comprising four cases. Postgrad Med. 1983; 73:75-82. https://pubmed.ncbi.nlm.nih.gov/6572892
21. Pickering JE. Clinical results with gemfibrozil. Am J Cardiol. 1983; 52:39-40B.
22. Torstila I, Kaukola S, Manninen V et al. Plasma prekallikrein, kallikrein inhibitors, kininogen and lipids during gemfibrozil treatment in type II dyslipidaemia. Acta Med Scand Suppl. 1982; 668:123-9. https://pubmed.ncbi.nlm.nih.gov/6188330
23. Manninen V. Clinical results with gemfibrozil and background to the Helsinki Heart Study. Am J Cardiol. 1983; 52:35-8B.
24. Manninen V, Malkonen M, Eisalo A et al. Gemfibrozil in the treatment of dyslipidaemia: a 5-year follow-up study. Acta Med Scand (Suppl). 1982: 668:82-7. (IDIS 168759)
25. Samuel P. Effects of gemfibrozil on serum lipids. Am J Med. 1983; 74(Suppl 5A):23-7. https://pubmed.ncbi.nlm.nih.gov/6573843
26. Fenderson RW, Deutsch S, Menachemi E et al. Effect of gemfibrozil on serum lipids in man. Angiology. 1982; 33:581-93. https://pubmed.ncbi.nlm.nih.gov/6751166
27. Nash DT. Hyperlipoproteinemia, atherosclerosis and gemfibrozil. Angiology. 1982; 33:594-602. https://pubmed.ncbi.nlm.nih.gov/6957155
28. Lewis JE. Long-term use of gemfibrozil (Lopid) in the treatment of dyslipidemia. Angiology. 1982; 33:603-12. https://pubmed.ncbi.nlm.nih.gov/6957156
29. Jain AK, Ryan JR, LaCorte WSJ et al. Clinical evaluation of gemfibrozil, a new antilipemic agent. Clin Pharmacol Ther. 1981; 29:254-5.
30. Vega GL, Grundy SM. Gemfibrozil therapy in primary hypertriglyceridemia associated with coronary heart disease: effects on metabolism of low-density lipoproteins. JAMA. 1985; 253:2398-403. https://pubmed.ncbi.nlm.nih.gov/3856692
31. Borresen AL, Berg K, Dahlen G et al. The effect of gemfibrozil on human serum apolipoproteins and on serum reserve cholesterol binding capacity (SRCBC). Artery. 1981; 9:77. https://pubmed.ncbi.nlm.nih.gov/7018466
32. Dahlen D, Gillnas T, Borresen AL et al. Effect of gemfibrozil on serum lipid levels. Artery. 1980; 7:224-31. https://pubmed.ncbi.nlm.nih.gov/7008748
33. Schwandt P, Weisweiler P, Neureuther G. Serum lipoprotein lipids after gemfibrozil treatment. Artery. 1979; 5:117-24. https://pubmed.ncbi.nlm.nih.gov/231950
34. Hall MJ, Nelson LM, Russell RI et al. Gemfibrozil—the effect of biliary cholesterol saturation of a new lipid-lowering agent and its comparison with clofibrate. Atherosclerosis. 1981; 39:511-6. https://pubmed.ncbi.nlm.nih.gov/6942844
35. Baird IM, Lewis B, Hill JM. Preliminary observations on the effect of gemfibrozil on the excretion of faecal bile acids. Proc R Soc Med. 1976; 69(Suppl 2):112-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864021/ https://pubmed.ncbi.nlm.nih.gov/1019150
36. Glueck C. Influence of gemfibrozil on high-density lipoproteins. Am J Cardiol. 1983; 52:31-4B.
37. Olsson AG, Rossner S, Walldius G et al. Effect of gemfibrozil on lipoprotein concentrations in different types of hyperlipoproteinaemia. Proc R Soc Med. 1976; 69(Suppl 2):28-31. https://pubmed.ncbi.nlm.nih.gov/190607
38. Vessby B, Lithell J, Boberg J et al. Gemfibrozil as a lipid lowering compound in hyperlipoproteinaemia. A placebo-controlled cross-over trial. Proc R Soc Med. 1976; 69(Suppl 2):32-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864027/ https://pubmed.ncbi.nlm.nih.gov/798194
39. Tuomilehto J, Salonen J, Kuusisto P et al. A clofibrate controlled trial of gemfibrozil in the treatment of hyperlipidaemias. Proc R Soc Med. 1976; 69(Suppl 2):38-40.
40. Beaumont JL, Dachet C. Binding of plasma lipoproteins of chlorophenoxyisobutyric, tibric and nicotinic acids and their esters. Proc R Soc Med. 1976; 69(Suppl 2):41-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864029/ https://pubmed.ncbi.nlm.nih.gov/1019153
41. Eisalo A, Manninen V. Gemfibrozil and clofibrate in the treatment of hyperlipidaemias: a comparative trial. Proc R Soc Med. 1976; 69(Suppl 2):47-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864013/ https://pubmed.ncbi.nlm.nih.gov/798197
42. Eisalo A, Manninen V, Malkonen M et al. Hypolipidaemic action of gemfibrozil in adult nephrotics. Proc R Soc Med. 1976; 69(Suppl 2):47-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864013/ https://pubmed.ncbi.nlm.nih.gov/798197
43. Eisalo A, Manninen V. A long-term trial of gemfibrozil in the treatment of hyperlipidaemias. Proc R Soc Med. 1976; 69(Suppl 2):49-52. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864023/ https://pubmed.ncbi.nlm.nih.gov/798198
44. Huunan-Seppala A, Manninen V, Burton R et al. Extrinsic factors affecting the response to gemfibrozil. Proc R Soc Med. 1976; 69(Suppl 2):53-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864032/ https://pubmed.ncbi.nlm.nih.gov/1019154
45. Nikkila EA, Ylikahri R, Huttunen JK. Gemfibrozil: effect on serum lipids, lipoproteins, post-heparin plasma lipase activities and glucose tolerance in primary hypertriglyceridaemia. Proc R Soc Med. 1976; 69(Suppl 2):58-63. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864025/ https://pubmed.ncbi.nlm.nih.gov/190608
46. de Salcedo I, Gorringe JAL, Luiz Salva J et al. Gemfibrozil in a group of diabetics. Proc R Soc Med. 1976; 69(Suppl 2):64-70.
47. Lageder H, Irsigler K. Evaluation of increasing doses of gemfibrozil in hyperlipoproteinaemia. Proc R Soc Med. 1976; 69(Suppl 2):71-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864014/ https://pubmed.ncbi.nlm.nih.gov/798199
48. Janus ED, Costa D, Ononogbu IC et al. The evaluation of lipoprotein changes during gemfibrozil treatment. Proc R Soc Med. 1976; 69(Suppl 2):76-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864026/ https://pubmed.ncbi.nlm.nih.gov/1019156
49. Honorato J, Masso RM, Purroy A. The use of gemfibrozil in the treatment of primary hyperlipoproteinaemia. Preliminary report. Proc R Soc Med. 1976; 69(Suppl 2):78-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864036/ https://pubmed.ncbi.nlm.nih.gov/798200
50. de la Iglesia FA, Pinn SM, Lucas J et al. Quantitative stereology of peroxisomes in hepatocytes from hyperlipoproteinemic patients receiving gemfibrozil. Micron. 1981; 12:97-8.
51. Bremner WF, Third JLHC, Clark B et al. CI-719 in hyperlipoproteinaemia: interim data. Proc R Soc Med. 1976; 69(Suppl 2):83-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864018/ https://pubmed.ncbi.nlm.nih.gov/798201
52. Howard AN, Ghosh P. Gemfibrozil treatment: a comparison with clofibrate. Proc R Soc Med. 1976; 69(Suppl 2):88-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864044/ https://pubmed.ncbi.nlm.nih.gov/190609
53. Wilkening J, Schwandt P. Summary of present data from a clinical trial of CI-719. Proc R Soc Med. 1976; 69(Suppl 2):90-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864022/ https://pubmed.ncbi.nlm.nih.gov/1019158
54. Kissebah AH, Adams PA, Wynn V. Lipokinetic studies with gemfibrozil (CI-719). Proc R Soc Med. 1976; 69(Suppl 2):94-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864040/ https://pubmed.ncbi.nlm.nih.gov/190610
55. Elkeles RS, Ashwell M, Priest R et al. The effect of CI-719 on lipolysis in rat adipose tissue. Proc R Soc Med. 1976; 69(Suppl 2):98-100. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864028/ https://pubmed.ncbi.nlm.nih.gov/1019159
56. C.dtdon LA. Effect of gemfibrozil in vitro on fat-mobilizing lipolysis in human adipose tissue. Proc R Soc Med. 1976; 69(Suppl 2):101-3.
57. Kallai-Sanfacon MA, Cayen MN, Dubuc J et al. Effect of AY-25, 712 and other lipid-lowering agents on liver catalase and liver carnitine acetyltransferase in rats (41658). Proc Soc Exp Biol Med. 1983; 173:367-71. https://pubmed.ncbi.nlm.nih.gov/6867010
58. O’Brien JR, Etherington MD, Shuttleworth RD et al. A pilot study of the effect of gemfibrozil on some haematological parameters. Thrombosis Res. 1982; 26:275-9.
59. Rasi VPO, Torstila I. Effect of gemfibrozil upon platelet function and blood coagulation. preliminary report. Proc R Soc Med. 1976; 69(Suppl 2):109-11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864038/ https://pubmed.ncbi.nlm.nih.gov/1019149
60. Wynn V, chairman. Gemfibrozil: a new lipid lowering agent: open forum. Proc R Soc Med. 1976; 69(Suppl 2):115-20.
61. Leiss O, von Bergmann K, Gnasso A et al. Effect of gemfibrozil on biliary lipid metabolism in normolipemic subjects. Metabolism. 1985; 34:74-82. https://pubmed.ncbi.nlm.nih.gov/3855325
62. Fitzgerald JE, Sanyer JL, Schardein JL et al. Carcinogen bioassay and mutagenicity studies with the hypolipidemic agent gemfibrozil. J Natl Cancer Inst. 1981; 67:1105-14. https://pubmed.ncbi.nlm.nih.gov/7029098
63. Nash DT. Gemfibrozil—a new lipid lowering agent. J Med. 1980; 11:107-16. https://pubmed.ncbi.nlm.nih.gov/6931871
64. National Institutes of Health Office of Medical Applications of Research. Consensus conference: treatment of hypertriglyceridemia. JAMA. 1984; 251:1196-1200. https://pubmed.ncbi.nlm.nih.gov/6582287
65. Levy RI. Current status of the cholesterol controversy. Am J Med. 1983; 74(Suppl 5A):1-4. https://pubmed.ncbi.nlm.nih.gov/6342382
66. Kuo PT. Hyperlipoproteinemia and atherosclerosis: dietary intervention. Am J Med. 1983; 74(Suppl 5A):15-8. https://pubmed.ncbi.nlm.nih.gov/6846377
67. Hunninghake DB. Pharmacologic therapy for the hyperlipidemic patient. Am J Med. 1983; 74(Suppl 5A):19-22. https://pubmed.ncbi.nlm.nih.gov/6846378
68. Anon. Gemfibrozil for hyperlipidemia. Med Lett Drugs Ther. 1982; 24:59-60. https://pubmed.ncbi.nlm.nih.gov/6953310
69. Probstfield JL, Gotto AM Jr. Disorders of lipids and lipoproteins. In: Stein JH, ed. Internal medicine. Boston: Little Brown and Company; 1983:1888-93.
70. National Institutes of Health Office of Medical Applications of Research. Consensus Conference: lowering blood cholesterol to prevent heart disease. JAMA. 1985; 253:2080-6. https://pubmed.ncbi.nlm.nih.gov/3974099
71. Gordon T, Castelli WP, Hjortland MC et al. High density lipoprotein as a protective factor against coronary heart disease: the Framingham study. Am J Med. 1977; 62:707-14. https://pubmed.ncbi.nlm.nih.gov/193398
72. Glueck CJ. Relationship of lipid disorders to coronary heart disease. Am J Med. 1983; 74(Suppl 5A):10-4. https://pubmed.ncbi.nlm.nih.gov/6846376
73. American Heart Association Committee to Design a Dietary Treatment of Hyperlipoproteinemia. Recommendations for treatment of hyperlipidemia in adults: a joint statement of the Nutrition Committee and the Council on Arteriosclerosis. Circulation. 1984; 69:1065-90A. https://pubmed.ncbi.nlm.nih.gov/6713610
74. Weinberger MH. Antihypertensive therapy and lipids: evidence, mechanisms, and implications. Arch Intern Med. 1985; 145:1102-5. https://pubmed.ncbi.nlm.nih.gov/2860883
75. Kissebah AH, Alfarsi S, Adams PW et al. Transport kinetics of plasma free fatty acids, very low density lipoprotein triglycerides and apoprotein in patients with endogenous hypertriglyceridemia: effects of 2,2-dimethyl,5(2,5-xylyloxy)valic acid therapy. Atherosclerosis. 1976; 24:199-218. https://pubmed.ncbi.nlm.nih.gov/182185
76. Brown MS, Goldstein JL. Drugs used in the treatment of hyperlipoproteinemias. In: Gilman AG, Goodman LS, Rall TW et al, eds. Goodman and Gilman’s the pharmacological basis of therapeutics. 7th ed. New York: The Macmillan Company; 1985:827-45.
77. National Heart, Lung, and Blood Institute Lipid Metabolism—Atherogenesis Branch. The lipid research clinics coronary primary prevention trial results: part I. Reduction in incidence of coronary heart disease. JAMA. 1984; 251:351-64. https://pubmed.ncbi.nlm.nih.gov/6361299
78. National Heart, Lung, and Blood Institute Lipid Metabolism—Atherogenesis Branch. The lipid research clinics coronary primary prevention trial results: part II. The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA. 1984; 251:365-74. https://pubmed.ncbi.nlm.nih.gov/6361300
79. Hansten PD. Drug interactions. 5th ed. Philadelphia: Lea & Febiger; 1985:76.
80. Manninen V, Malkonen M. Effect of gemfibrozil on the blood levels of the high density lipoprotein subfractions HDL2 and HDL3. Res Clin Forums. 1982; 4:77-83.
81. W.H.O. cooperative trial on primary prevention of ischaemic heart disease using clofibrate to lower serum cholesterol: mortality follow-up. Report from the Committee of Principal Investigators. Lancet. 1980; 2:379-85.
82. A co-operative trial in the primary prevention of ischaemic heart disease using clofibrate. Report from the Committee of Principal Investigators. Br Heart J. 1978; 40:1069-118. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC483536/ https://pubmed.ncbi.nlm.nih.gov/361054
83. WHO cooperative trial on primary prevention of ischaemic heart disease with clofibrate to lower serum cholesterol: final mortality follow-up. Report from the Committee of Principal Investigators. Lancet. 1984; 2:600-4. https://pubmed.ncbi.nlm.nih.gov/6147641
84. The Coronary Drug Project Research Group. Clofibrate and niacin in coronary heart disease. JAMA. 1975; 231:360-81. https://pubmed.ncbi.nlm.nih.gov/1088963
85. The Coronary Drug Project Research Group. Gallbladder disease as a side effect of drugs influencing lipid metabolism: experience in the Coronary Drug Project. N Engl J Med. 1977; 296:1185-90. https://pubmed.ncbi.nlm.nih.gov/323705
86. Oliver MF. Cholesterol, coronaries, clofibrate and death. N Engl J Med. 1978; 299:1360-2. https://pubmed.ncbi.nlm.nih.gov/362204
87. Green KG. Interpretation of clofibrate trial. Lancet. 1984; 2:1095-6. https://pubmed.ncbi.nlm.nih.gov/6150164
88. Glueck CJ. Nonpharmacologic and pharmacologic alteration of high-density lipoprotein cholesterol: therapeutic approaches to prevention of atherosclerosis. Am Heart J. 1985; 110:1107-15. https://pubmed.ncbi.nlm.nih.gov/2865887
89. American Medical Association Council on Scientific Affairs. Dietary and pharmacologic therapy for the lipid risk factors. JAMA. 1983; 250:1873-9. https://pubmed.ncbi.nlm.nih.gov/6620484
90. Anon. Lipid-lowering drugs. Med Lett Drugs Ther. 1985; 27:74-6. https://pubmed.ncbi.nlm.nih.gov/3860714
91. Saku K, Gartside PS, Hynd BA et al. Mechanism of action of gemfibrozil on lipoprotein metabolism. J Clin Invest. 1985; 75:1702-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC425514/ https://pubmed.ncbi.nlm.nih.gov/3923042
92. Grundy SM. Consensus statement: role of therapy with “statins” in patients with hypertriglyceridemia. Am J Cardiol. 1998; 81:1-6B. https://pubmed.ncbi.nlm.nih.gov/9462596
93. Mahley RW. Atherogenic lipoproteins and coronary artery disease: concepts derived from recent advances in cellular and molecular biology. Circulation. 1985; 72:943-8. https://pubmed.ncbi.nlm.nih.gov/4042302
94. Reviewers’ comments (personal observations); 1985 Dec.
95. Cheung MC, Albers JJ, Wahl PW et al. High density lipoproteins during hypolipidemic therapy: a comparative study of four drugs. Atherosclerosis. 1980; 35:215-28. https://pubmed.ncbi.nlm.nih.gov/7362696
96. Hazzard WR, Wahl PW, Gagne C et al. Plasma and lipoprotein lipid responses to four hypolipid drugs. Lipids. 1984; 19:73-9. https://pubmed.ncbi.nlm.nih.gov/6708754
97. Pierides AM, Alvarez-Ude F, Kerr DN. Clofibrate-induced muscle damage in patients with chronic renal failure. Lancet. 1975; 2:1279-82. https://pubmed.ncbi.nlm.nih.gov/54800
98. Bridgman JF, Rosen SM, Thorp JM. Complications during clofibrate treatment on nephrotic-syndrome hyperlipoproteinaemia. Lancet. 1972; 2:506-9. https://pubmed.ncbi.nlm.nih.gov/4115569
99. Levy RI, Brensike JF, Epstein SE et al. The influence of changes in lipid values induced by cholestyramine and diet on progression of coronary artery disease: results of the NHLBI Type II Coronary Intervention Study. Circulation. 1984; 69:325-37. https://pubmed.ncbi.nlm.nih.gov/6360415
100. Gosselin RE, Smith RP, Hodge HC. Clinical toxicology of commercial products. 5th ed. Baltimore: Williams & Wilkins; 1984:I-10.
101. Brensike JF, Levy RI, Kelsey SF et al. Effects of therapy with cholestyramine on progression of coronary arteriosclerosis: results of the NHLBI Type II Coronary Intervention Study. Circulation. 1984; 69:313-24. https://pubmed.ncbi.nlm.nih.gov/6360414
102. Rhodes DF (Parke-Davis, Morris Plains, NJ): Personal communication; 1986 Jan 21.
103. Hoeg JM, Gregg RE, Brewer HB. An approach to the management of hyperlipoproteinemia. JAMA. 1986; 255:512-21. https://pubmed.ncbi.nlm.nih.gov/3510334
104. Frick MH, Elo O, Haapa K et al. Helsinki Heart Study: primary prevention trial with gemfibrozil in middle-aged men with dyslipidemia: safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987; 317:1237-45. https://pubmed.ncbi.nlm.nih.gov/3313041
105. Rifkind BM. Gemfibrozil, lipids, and coronary risk. N Engl J Med. 1987; 317:1279-81. https://pubmed.ncbi.nlm.nih.gov/3313042
106. The Expert Panel (coordinated by the National Heart, Lung, and Blood Institute). Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Arch Intern Med. 1988; 148:36-69. https://pubmed.ncbi.nlm.nih.gov/3422148
107. Gordon DJ, Knoke J, Probstfield JL et al. High-density lipoprotein cholesterol and coronary heart disease in hypercholesterolemic men: the Lipid Research Clinics Coronary Primary Prevention Trial. Circulation. 1986; 74:1217-25. https://pubmed.ncbi.nlm.nih.gov/3536151
108. Tobert JA. Rhabdomyolysis in patients receiving lovastatin after cardiac transplantation. N Engl J Med. 1988; 318:48. https://pubmed.ncbi.nlm.nih.gov/3257291
109. Fisher DA, Elias PM, LeBoit PL. Exacerbation of psoriasis by the hypolipidemic agent, gemfibrozil. Arch Dermatol. 1988; 124:854-5. https://pubmed.ncbi.nlm.nih.gov/3163912
110. Manninen V, Elo O, Frick MH et al. Lipid alterations and decline in the incidence of coronary heart disease in the Helsinki Heart Study. JAMA. 1988; 260:641-51. https://pubmed.ncbi.nlm.nih.gov/3164788
111. Manninen V, Frick MH, Heinonen OP et al. Lipid level alterations in the Helsinki Heart Study. JAMA. 1989; 261:554-5. https://pubmed.ncbi.nlm.nih.gov/2909790
112. American Heart Association. AHA conference report on cholesterol. Circulation. 1989; 80:715-48. https://pubmed.ncbi.nlm.nih.gov/2670320
113. Miller NE. Associations of high-density lipoprotein subclasses and apolipoproteins with ischemic heart disease and coronary atherosclerosis. Am Heart J. 1987; 113:589-97. https://pubmed.ncbi.nlm.nih.gov/3544775
114. Pocock SJ, Shaper AG, Phillips AN et al. High density lipoprotein cholesterol is not a major risk factor for ischaemic heart disease in British men. BMJ. 1986; 292:515-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1339503/ https://pubmed.ncbi.nlm.nih.gov/3081149
115. Langer T, Levy RI. Acute muscular syndrome associated with administration of clofibrate. N Engl J Med. 1968; 279:856-8. https://pubmed.ncbi.nlm.nih.gov/5677720
116. East C, Alivizatos PA, Grundy SM et al. Rhabdomyolysis in patients receiving lovastatin after cardiac transplantation. N Engl J Med. 1988; 318:47-8. https://pubmed.ncbi.nlm.nih.gov/3275892
117. Sekowski I, Samuel P. Clofibrate-induced acute muscular syndrome. Am J Cardiol. 1972; 30:572-4. https://pubmed.ncbi.nlm.nih.gov/5073673
118. Goldstein MR. Myopathy and rhabdomyolysis with lovastatin taken with gemfibrozil. JAMA. 1990; 264:2991. https://pubmed.ncbi.nlm.nih.gov/2243420
119. Van Lente F, Cornell W. Myopathy and rhabdomyolysis with lovastatin taken with gemfibrozil. JAMA. 1990; 264:2991-2. https://pubmed.ncbi.nlm.nih.gov/2243420
120. Pierce LR, Wysowski DK, Gross TP. Myopathy and rhabdomyolysis associated with lovastatin-gemfibrozil combination therapy. JAMA. 1990; 264:71-5. https://pubmed.ncbi.nlm.nih.gov/2355431
121. Marais GE, Larson KK. Rhabdomyolysis and acute renal failure induced by combination lovastatin and gemfibrozil therapy. Ann Intern Med. 1990; 112:228-30. https://pubmed.ncbi.nlm.nih.gov/2297197
122. Mäntari M, Romo M, Manninen V et al. Reduction in Q wave myocardial infarctions with gemfibrozil in the Helsinki heart study. Am Heart J. 1990; 119:991-5. https://pubmed.ncbi.nlm.nih.gov/2330888
123. Pizarro S, Bargay J, D’Agosto P. Gemfibrozil-induced impotence. Lancet. 1990; 336:1135.
124. Ahmad S. Gemfibrozil interaction with warfarin sodium (Coumadin). Chest. 1990; 98:1041-2. https://pubmed.ncbi.nlm.nih.gov/2209118
125. Bain SC, Lemon M, Jones AF. Gemfibrozil-induced impotence. Lancet. 1990; 336:1389. https://pubmed.ncbi.nlm.nih.gov/1978207
126. Lopid (gemfibrozil tablets) prescribing information. In: Physician’s desk reference. 47th ed. Montvale, NJ: Medical Economics Company Inc; 1993 (Suppl A):A144.
127. The Expert Panel. Second Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II). Circulation. 1994; 89:1329-1445.
128. Lopid (gemfibrozil) prescibing information. In: Pysicians’ desk reference. 52nd ed. Montvale, NJ: Medical Economics Company Inc; 1998(Suppl A):A242.
129. Gibbons RJ, Chatterjee K, Daley J et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients with Chronic Stable Angina). J Am Coll Cardiol. 1999; 33:2092-197. https://pubmed.ncbi.nlm.nih.gov/10362225
130. Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Survival Study (4S). Lancet. 1994; 344:1383-9. https://pubmed.ncbi.nlm.nih.gov/7968073
131. Sacks FN, Pfeffer MA, Maye LA et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996; 335:1001-9. https://pubmed.ncbi.nlm.nih.gov/8801446
132. The Long-term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998; 339:1349-57. https://pubmed.ncbi.nlm.nih.gov/9841303
133. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of high Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001; 285:2486-97. https://pubmed.ncbi.nlm.nih.gov/11368702
134. Anon. Bayer voluntarily withdraws Baycol. FDA Talk Paper. Rockville, MD: Food and Drug Administration; 2001 Aug 8.
135. Mac Carthy EP. Dear Doctor letter regarding market withdrawal of Baycol (cerivastatin). West Haven, CT: Bayer Corporation; 2001 Aug 8.
136. National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults: Adult Treatment Panel III Report. From AHA web site. http://www.nhlbi.nih.gov/guidelines/cholesterol/atp3_rpt.htm
137. Rubins HB, Robins SJ, Collins D et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. New Engl J Med. 1999; 341:410-8. https://pubmed.ncbi.nlm.nih.gov/10438259
138. Novo Nordisk Pharmaceuticals, Inc. Prandin (repaglinide) tablets prescribing information. Princeton, NJ; 2003 Aug.
139. Niemi M, Backman JT, Neuvonen M et al. Effects of gemfibrozil, itraconazole, and their combination on the pharmacokinetics and pharmacodynamics of repaglinide: potentially hazardous interaction between gemfibrozil and repaglinide. Diabetologia. 2003; 46:347-51. https://pubmed.ncbi.nlm.nih.gov/12687332
352. Eckel RH, Jakicic JM, Ard JD et al. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2960-84. https://pubmed.ncbi.nlm.nih.gov/24239922
353. ACCORD Study Group, Ginsberg HN, Elam MB et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010; 362:1563-74. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2879499/ https://pubmed.ncbi.nlm.nih.gov/20228404
356. Miller M, Stone NJ, Ballantyne C et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011; 123:2292-333. https://pubmed.ncbi.nlm.nih.gov/21502576
400. Grundy SM, Stone NJ, Bailey AL et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019; 139:e1082-e1143. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC7403606/ https://pubmed.ncbi.nlm.nih.gov/30586774
Related/similar drugs
Frequently asked questions
More about gemfibrozil
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (27)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: fibric acid derivatives
- Breastfeeding
- En español