Delafloxacin (Monograph)
Brand name: Baxdela
Drug class: Quinolones
Chemical name: 1-(6-amino-3,5-difluoropyridin-2-yl)-8-chloro-6-fluoro-7-(3-hydroxyazetidin-1-yl)-4-oxoquinoline-3-carboxylic acid
Molecular formula: C18H12ClF3N4O4
CAS number: 1256037-58-7
Warning
- Serious Adverse Reactions
-
Fluoroquinolones have been associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that have occurred together. Discontinue immediately and avoid use of fluoroquinolones, including delafloxacin, in patients who have experienced any of these serious adverse reactions. (See Warnings under Cautions.)
-
Fluoroquinolones may exacerbate muscle weakness in patients with myasthenia gravis. Avoid in patients with known history of myasthenia gravis.
Introduction
Antibacterial; fluoroquinolone.
Uses for Delafloxacin
Skin and Skin Structure Infections
Treatment of acute bacterial skin and skin structure infections (ABSSSI) caused by susceptible Staphylococcus aureus (including methicillin-resistant S. aureus [MRSA; also known as oxacillin-resistant S. aureus or ORSA] and methicillin-susceptible S. aureus), S. haemolyticus, S. lugdunensis, Streptococcus pyogenes (group A β-hemolytic streptococci, GAS), S. agalactiae (group B streptococci, GBS), S. anginosus group (includes S. anginosus, S. intermedius, and S. constellatus), Enterococcus faecalis, Escherichia coli, Enterobacter cloacae, Klebsiella pneumoniae, or Pseudomonas aeruginosa.
Delafloxacin Dosage and Administration
Administration
Administer orally or by slow IV infusion.
Oral Administration
Administer tablets orally without regard to meals. (See Food under Pharmacokinetics.)
Administer orally at least 2 hours before or 6 hours after antacids containing magnesium or aluminum, metal cations (e.g., iron), sucralfate, multivitamins or dietary supplements containing iron or zinc, or buffered didanosine preparations. (See Specific Drugs under Interactions.)
IV Infusion
Must be reconstituted and further diluted prior to IV infusion. Observe strict aseptic technique when preparing IV solutions.
Do not infuse simultaneously through same tubing with other drugs. Do not administer with any solution containing multivalent cations (e.g., calcium, magnesium).
If common IV line used to administer other drugs, flush with 0.9% sodium chloride injection or 5% dextrose injection before and after each delafloxacin infusion.
Vials of lyophilized powder for injection are for single use only.
For solution and drug compatibility information, see Compatibility under Stability.
Reconstitution
Reconstitute vial containing 300 mg of delafloxacin by adding 10.5 mL of 0.9% sodium chloride injection or 5% dextrose injection to provide a solution containing 25 mg/mL.
Shake vial vigorously until contents completely dissolved. Reconstituted solution should appear clear yellow to amber in color.
Dilution
To prepare a 300-mg dose of delafloxacin in a 250-mL infusion bag containing 0.9% sodium chloride injection or 5% dextrose injection, remove 12 mL of the diluent from infusion bag, then inject 12 mL of reconstituted delafloxacin solution into the bag. Concentration of final infusion solution is 1.2 mg/mL.
To prepare a 200-mg dose of delafloxacin in a 250-mL infusion bag containing 0.9% sodium chloride injection or 5% dextrose injection, remove 8 mL of the diluent from infusion bag, then inject 8 mL of reconstituted delafloxacin solution into the bag. Concentration of final infusion solution is 0.8 mg/mL.
Rate of Administration
Administer by IV infusion over 1 hour.
Dosage
Available as delafloxacin meglumine; dosage expressed in terms of delafloxacin.
Adults
Skin and Skin Structure Infections
Oral
450 mg every 12 hours for 5–14 days.
IV
300 mg every 12 hours for 5–14 days.
IV therapy may be switched to oral therapy at discretion of clinician. Total duration of IV and oral therapy is 5–14 days.
Special Populations
Hepatic Impairment
Mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, or C): Dosage adjustments not needed.
Renal Impairment
Oral
Mild, moderate, or severe renal impairment (estimated GFR [eGFR] of 15–89 mL/minute per 1.73 m2): Dosage adjustments not needed.
End-stage renal disease (eGFR <15 mL/minute per 1.73 m2): Not recommended.
IV
Mild or moderate renal impairment (eGFR of 30–89 mL/minute per 1.73 m2): Dosage adjustments not needed.
Severe renal impairment (eGFR of 15–29 mL/minute per 1.73 m2): 200 mg every 12 hours.
End-stage renal disease (eGFR <15 mL/minute per 1.73 m2): Not recommended.
Geriatric Patients
No dosage adjustments except those related to renal impairment. (See Renal Impairment under Dosage and Administration.)
Cautions for Delafloxacin
Contraindications
-
Known hypersensitivity to delafloxacin, any component of the preparation, or other fluoroquinolones.
Warnings/Precautions
Warnings
Disabling and Potentially Irreversible Serious Adverse Reactions
Systemic fluoroquinolones are associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that can occur together in the same patient. May occur within hours to weeks after a systemic fluoroquinolone is initiated; have occurred in all age groups and in patients without preexisting risk factors for such adverse reactions.
Immediately discontinue at first signs or symptoms of any serious adverse reactions.
Avoid systemic fluoroquinolones, including delafloxacin, in patients who have experienced any serious adverse reactions associated with fluoroquinolones.
Tendinitis and Tendon Rupture
Systemic fluoroquinolones are associated with an increased risk of tendinitis and tendon rupture in all age groups.
Risk of developing fluoroquinolone-associated tendinitis and tendon rupture is increased in older adults (usually those >60 years of age), individuals receiving concomitant corticosteroids, and kidney, heart, or lung transplant recipients. (See Geriatric Use under Cautions.)
Other factors that may independently increase the risk of tendon rupture include strenuous physical activity, renal failure, and previous tendon disorders such as rheumatoid arthritis. Tendinitis and tendon rupture have been reported in patients receiving fluoroquinolones who did not have any risk factors for such adverse reactions.
Fluoroquinolone-associated tendinitis and tendon rupture most frequently involve the Achilles tendon; also reported in the rotator cuff (shoulder), hand, biceps, thumb, and other tendon sites.
Tendinitis and tendon rupture can occur within hours or days after therapy initiated or as long as several months after completion of therapy; can occur bilaterally.
Immediately discontinue delafloxacin if pain, swelling, inflammation, or rupture of a tendon occurs. (See Advice to Patients.)
Avoid systemic fluoroquinolones, including delafloxacin, in patients who have a history of tendon disorders or have experienced tendinitis or tendon rupture.
Peripheral Neuropathy
Systemic fluoroquinolones are associated with an increased risk of peripheral neuropathy.
Sensory or sensorimotor axonal polyneuropathy affecting small and/or large axons resulting in paresthesias, hypoesthesias, dysesthesias, and weakness reported with fluoroquinolones, including delafloxacin. Symptoms may occur soon after initiation of the drug and, in some patients, may be irreversible.
Immediately discontinue delafloxacin if symptoms of peripheral neuropathy (e.g., pain, burning, tingling, numbness, and/or weakness) occur or if there are other alterations in sensations (e.g., light touch, pain, temperature, position sense, vibratory sensation, and/or motor strength).
Avoid systemic fluoroquinolones, including delafloxacin, in patients who have experienced peripheral neuropathy.
CNS Effects
Systemic fluoroquinolones are associated with an increased risk of adverse psychiatric effects, including toxic psychosis, hallucinations, paranoia, depression, suicidal thoughts or acts, delirium, disorientation, confusion, disturbances in attention, anxiety, agitation, nervousness, insomnia, nightmares, and memory impairment. These adverse effects may occur after first dose.
Systemic fluoroquinolones are associated with increased risk of convulsions (seizures), increased intracranial pressure (including pseudotumor cerebri), dizziness, and tremors. Use delafloxacin in patients with known or suspected CNS disorders (e.g., severe cerebral arteriosclerosis, epilepsy) or other risk factors that predispose to seizures or lower seizure threshold only if potential benefits outweigh risks.
If psychiatric or other CNS effects occur, immediately discontinue delafloxacin and institute appropriate measures. (See Advice to Patients.)
Exacerbation of Myasthenia Gravis
Fluoroquinolones have neuromuscular blocking activity and may exacerbate muscle weakness in myasthenia gravis patients; death or need for ventilatory support reported.
Avoid use in patients with known history of myasthenia gravis. (See Advice to Patients.)
Sensitivity Reactions
Hypersensitivity
Serious and occasionally fatal hypersensitivity and/or anaphylactic reactions reported in patients receiving fluoroquinolones. These reactions may occur with first or subsequent doses.
Some hypersensitivity reactions reported with fluoroquinolones have been accompanied by cardiovascular collapse, loss of consciousness, tingling, edema (pharyngeal or facial), dyspnea, urticaria, or pruritus.
Hypersensitivity and urticaria reported in patients receiving delafloxacin.
Immediately discontinue delafloxacin at first appearance of rash or any other sign of hypersensitivity. (See Advice to Patients.)
Photosensitivity
No evidence of phototoxic potential.
Other Warnings and Precautions
Risk of Aortic Aneurysm and Dissection
Rupture or dissection of aortic aneurysms reported in patients receiving systemic fluoroquinolones. Epidemiologic studies indicate an increased risk of aortic aneurysm and dissection within 2 months following use of systemic fluoroquinolones, particularly in elderly patients. Cause for this increased risk not identified.
Unless there are no other treatment options, do not use systemic fluoroquinolones, including delafloxacin, in patients who have an aortic aneurysm or are at increased risk for an aortic aneurysm. This includes elderly patients and patients with peripheral atherosclerotic vascular disease, hypertension, or certain genetic conditions (e.g., Marfan syndrome, Ehlers-Danlos syndrome).
If patient reports adverse effects suggestive of aortic aneurysm or dissection, immediately discontinue the fluoroquinolone. (See Advice to Patients.)
Hypoglycemia or Hyperglycemia
Systemic fluoroquinolones are associated with alterations in blood glucose concentrations, including symptomatic hypoglycemia and hyperglycemia. Blood glucose disturbances during fluoroquinolone therapy usually have occurred in patients with diabetes mellitus receiving an oral antidiabetic agent (e.g., glyburide) or insulin.
Severe cases of hypoglycemia resulting in coma or death reported with some systemic fluoroquinolones. Although most reported cases of hypoglycemic coma involved patients with risk factors for hypoglycemia (e.g., older age, diabetes mellitus, renal insufficiency, concomitant use of antidiabetic agents [especially sulfonylureas]), some involved patients receiving a fluoroquinolone who were not diabetic and not receiving an oral antidiabetic agent or insulin.
Carefully monitor blood glucose concentrations when systemic fluoroquinolones, including delafloxacin, used in diabetic patients receiving antidiabetic agents.
If hypoglycemic reaction occurs, discontinue the fluoroquinolone and immediately initiate appropriate therapy. (See Advice to Patients.)
C. difficile-associated Diarrhea and Colitis
Treatment with anti-infectives alters normal colon flora and may permit overgrowth of Clostridioides difficile (formerly known as Clostridium difficile). C. difficile infection (CDI) and C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) reported with nearly all anti-infectives, including delafloxacin, and may range in severity from mild diarrhea to fatal colitis. C. difficile produces toxins A and B which contribute to development of CDAD; hypertoxin-producing strains of C. difficile are associated with increased morbidity and mortality since they may be refractory to anti-infectives and colectomy may be required.
Consider CDAD if diarrhea develops during or after therapy and manage accordingly. Obtain careful medical history since CDAD may occur as late as ≥2 months after anti-infective therapy is discontinued.
If CDAD suspected or confirmed, discontinue anti-infectives not directed against C. difficile as soon as possible. Manage using appropriate anti-infective therapy directed against C. difficile (e.g., vancomycin, fidaxomicin, metronidazole), supportive therapy (e.g., fluid and electrolyte management, protein supplementation), and surgical evaluation as clinically indicated.
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of delafloxacin and other antibacterials, use only for treatment of infections proven or strongly suspected to be caused by susceptible bacteria.
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing. In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.
Information on test methods and quality control standards for in vitro susceptibility testing of antibacterial agents and specific interpretive criteria for such testing recognized by FDA is available at [Web].
Specific Populations
Pregnancy
Available data regarding use in pregnant women insufficient to inform any drug-associated risk for miscarriages or major birth defects.
When administered orally to pregnant rats, no malformations or fetal deaths observed at delafloxacin concentrations 7 times estimated clinical exposure. Maternal toxicity and reduced fetal body weight observed at highest dosage (1.6 g/kg daily); fetal ossification delays observed at all doses. Following IV administration to rats in late pregnancy through lactation, no adverse effects on offspring observed at clinically relevant concentrations.
Lactation
Distributed into milk in lactating rats; not known if distributes into human milk, affects breast-fed infant, or affects milk production.
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for delafloxacin; also consider potential adverse effects on breast-fed infant from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy not established in children or adolescents <18 years of age; use in pediatric patients not recommended.
Quinolones cause arthropathy in juvenile animals.
Manufacturer states clinical trials evaluating delafloxacin for treatment of bacterial skin and skin structure infections did not include patients <18 years of age because risks versus benefits do not support use of the drug for such infections in this age group.
AAP states use of a systemic fluoroquinolone may be justified in children <18 years of age in certain specific circumstances when there are no safe and effective alternatives and the drug is known to be effective.
Geriatric Use
About 15% of patients receiving delafloxacin in clinical studies were ≥65 years of age. Clinical response rate at 48–72 hours was about 76% in patients ≥65 years of age compared with about 82% in those <65 years of age.
Risk of severe tendon disorders, including tendon rupture, is increased in older adults (usually those >60 years of age). This risk is further increased in those receiving concomitant corticosteroids. (See Tendinitis and Tendon Rupture under Cautions.) Use caution in geriatric adults, especially those receiving concomitant corticosteroids.
Risk of aortic aneurysm and dissection may be increased in geriatric patients. (See Risk of Aortic Aneurysm and Dissection under Cautions.)
Hepatic Impairment
No clinically important differences in pharmacokinetics in adults with mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, or C); dosage adjustments not needed in such patients.
Renal Impairment
Severe renal impairment (eGFR of 15–29 mL/minute per 1.73 m2): Accumulation of the IV delafloxacin vehicle, sulfobutylether-β-cyclodextrin (SBECD), occurs. Reduce dosage (see Renal Impairment under Dosage and Administration) and closely monitor Scr and eGFR in patients receiving IV delafloxacin. Consider switching to oral delafloxacin if Scr increases during IV delafloxacin treatment. If eGFR decreases to <15 mL/minute per 1.73 m2, discontinue delafloxacin.
End-stage renal disease (eGFR <15 mL/minute per 1.73 m2): Accumulation of IV delafloxacin vehicle (SBECD) occurs. Use of delafloxacin (oral or IV) not recommended.
Common Adverse Effects
GI effects (nausea, diarrhea, vomiting), headache, elevated aminotransferase concentrations.
Drug Interactions
Does not inhibit CYP1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A4/5 in vitro at clinically relevant concentrations; shows no potential for induction of CYP1A2, 2B6, 2C19, or 2C8. Mild induction of CYP2C9 and 3A4 in vitro.
Drugs Affecting or Affected by Membrane Transporters
Substrate of P-glycoprotein (P-gp) transport and breast cancer resistance protein (BCRP) in vitro; clinical importance of concomitant use with P-gp inhibitors and/or BCRP inhibitors not known.
Does not inhibit multidrug-resistance gene (MDR) 1, BCRP, organic anion transporter (OAT) 1, OAT3, organic anion transporting polypeptide (OATP) 1B1, OATP1B3, bile salt export pump (BSEP), or organic cation transporter (OCT) 1 or OCT2 at clinically relevant concentrations.
Not a substrate of OAT1, OAT3, OCT1, OCT2, OATP1B1, or OATP1B3.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum- or magnesium-containing) |
Possible decreased oral absorption and decreased systemic concentrations of delafloxacin; effect on IV delafloxacin unknown |
Administer oral delafloxacin at least 2 hours before or 6 hours after antacids containing aluminum or magnesium |
|
Antibacterials |
Aztreonam, ceftazidime, colistin (commercially available in US as colistimethate sodium), co-trimoxazole, daptomycin, linezolid, meropenem, tigecycline, or vancomycin: No in vitro evidence of synergistic or antagonistic antibacterial effects |
|
|
Didanosine |
Possible decreased oral absorption and decreased systemic concentrations of delafloxacin if used concomitantly with buffered didanosine (pediatric powder for oral solution); effect on IV delafloxacin unknown |
Administer oral delafloxacin at least 2 hours before or 6 hours after buffered didanosine |
|
Iron preparations |
Possible decreased oral absorption and decreased systemic concentrations of delafloxacin; effect on IV delafloxacin unknown |
Administer oral delafloxacin at least 2 hours before or 6 hours after iron preparations |
|
Midazolam |
No substantial effect on peak plasma concentrations or AUC of midazolam or its metabolite (1-hydroxymidazolam) |
|
|
Multivitamins and dietary supplements |
Possible decreased oral absorption and decreased systemic concentrations of delafloxacin; effect on IV delafloxacin unknown |
Administer oral delafloxacin at least 2 hours before or 6 hours after multivitamins or dietary supplements containing iron or zinc |
|
Sucralfate |
Possible decreased oral absorption and decreased systemic concentrations of delafloxacin; effect on IV delafloxacin unknown |
Administer oral delafloxacin at least 2 hours before or 6 hours after sucralfate |
Delafloxacin Pharmacokinetics
Absorption
Bioavailability
Oral: Absolute bioavailability is 58.8%. Peak plasma concentrations attained 0.75 hours after single dose and 1 hour after a dose at steady state.
IV: Peak plasma concentrations attained at end of 1-hour infusion after single dose and at steady state.
Steady state achieved within approximately 3 days after oral or IV delafloxacin with accumulation of approximately 36 or 10%, respectively.
AUC after single 450-mg oral dose is comparable to AUC after single 300-mg IV dose. Peak plasma concentrations are approximately 55% lower following oral administration; not considered clinically important.
Food
No substantial effect on oral bioavailability.
Distribution
Extent
Volume of distribution at steady state is 30–48 L, which approximates total body water.
Distributed into breast milk in rats; not known if distributed into human breast milk.
Plasma Protein Binding
84%, principally albumin.
Special Populations
Plasma protein binding not substantially affected in patients with renal impairment.
Elimination
Metabolism
Metabolized primarily via glucuronidation by UGT1A1, 1A3, and 2B15; about 1% of a dose undergoes oxidative metabolism.
Elimination Route
Oral: 50% of a dose eliminated in urine as unchanged delafloxacin and glucuronide metabolites; 48% in feces as unchanged drug.
IV: 65% of a dose eliminated in urine as unchanged delafloxacin and glucuronide metabolites; 28% in feces as unchanged drug.
Half-life
Oral: 4.2–8.5 hours.
IV: 3.7 hours.
Special Populations
Mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, or C): Peak plasma concentrations and AUC not substantially affected.
Mild renal impairment (eGFR of 51–80 mL/minute per 1.73 m2): Oral exposures comparable to those in healthy individuals; IV exposures increased 1.3-fold.
Moderate renal impairment (eGFR of 31–50 mL/minute per 1.73 m2): Oral exposures increased 1.5-fold. IV exposures increased 1.6-fold; exposures of IV vehicle (SBECD) increased 2-fold.
Severe renal impairment (eGFR of 15–29 mL/minute per 1.73 m2): Oral exposures increased 1.5-fold. IV exposures increased 1.8-fold; exposures of IV vehicle (SBECD) increased 5-fold.
End-stage renal disease (eGFR <15 mL/minute per 1.73 m2) on hemodialysis: When administered IV 1 hour before and 1 hour after hemodialysis, delafloxacin exposures increased 2.1- and 2.6-fold, respectively, and IV vehicle (SBECD) exposures increased 7.5- and 27-fold, respectively. Approximately 19 and 56% of delafloxacin and SBECD, respectively, recovered in dialysate after 4 hours of hemodialysis.
Pharmacokinetics not substantially affected by age, gender, race, weight, or body mass index.
Stability
Storage
Oral
Tablets
20–25°C (may be exposed to 15–30°C).
Parenteral
Powder for Injection, for IV Infusion
20–25°C (may be exposed to 15–30°C).
Reconstituted or reconstituted and further diluted solutions may be stored under refrigeration or at controlled room temperature for up to 24 hours.
Compatibility
Parenteral
Solution Compatibility1 HID
|
Compatible |
|---|
|
Dextrose 5% |
|
Sodium chloride 0.9% |
|
Incompatible |
|
Dextrose 5% in Ringer's injection |
|
Dextrose 5% in Ringer's injection, lactated |
|
Ringer's injection |
|
Ringer's injection, lactated |
Actions and Spectrum
-
Like other fluoroquinolones, inhibits bacterial topoisomerase IV and DNA gyrase (i.e., topoisomerase II) enzymes. Demonstrates similar affinity for both topoisomerase IV and DNA gyrase.
-
Exhibits concentration-dependent bactericidal activity.
-
Gram-positive aerobes: Active in vitro and in clinical infections against S. aureus (including methicillin-resistant S. aureus [MRSA; also known as oxacillin-resistant S. aureus or ORSA] and methicillin-susceptible S. aureus), S. haemolyticus, S. lugdunensis, S. pyogenes (group A β-hemolytic streptococci, GAS), S. agalactiae (group B streptococci, GBS), S. anginosus group (including S. anginosus, S. intermedius, and S. constellatus), and E. faecalis. Active in vitro against some staphylococci (including MRSA), streptococci, and enterococci resistant to some other fluoroquinolones.
-
Gram-negative aerobes: Active in vitro and in clinical infections against E. coli, E. cloacae, K. pneumoniae, and Ps. aeruginosa.
-
Resistance can occur due to mutations in target regions of topoisomerase IV and/or DNA gyrase (i.e., quinolone-resistance determining regions [QRDRs]) or through altered efflux. In vitro, resistance develops by multiple step mutations in QRDRs of gram-positive and gram-negative bacteria (e.g., double mutations in gyrA and parC).
-
Cross-resistance between delafloxacin and other fluoroquinolones reported; however, some gram-positive and gram-negative bacteria resistant to other fluoroquinolones may be susceptible to delafloxacin.
Advice to Patients
-
Advise patients to read manufacturer’s patient information (medication guide).
-
Advise patients that antibacterials (including delafloxacin) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).
-
Advise patients that delafloxacin tablets may be taken without regard to food.
-
Importance of taking delafloxacin tablets at least 2 hours before or 6 hours after magnesium- or aluminum- containing antacids, sucralfate, multivitamins or dietary supplements containing iron or zinc, or buffered didanosine (pediatric powder for oral solution).
-
Importance of completing full course of therapy, even if feeling better after a few days. Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with delafloxacin or other antibacterials in the future.
-
If a dose of delafloxacin is missed and remembered within 8 hours after the scheduled time, take the dose as soon as possible and take the next dose at the regularly scheduled time. If a dose is missed and remembered >8 hours after the scheduled time, skip the dose and take the next dose at the regularly scheduled time.
-
Inform patients that systemic fluoroquinolones have been associated with disabling and potentially irreversible serious adverse reactions (e.g., tendinitis and tendon rupture, peripheral neuropathy, CNS effects) that may occur together in the same patient. Advise patients to immediately discontinue delafloxacin and contact a clinician if they experience any signs or symptoms of serious adverse effects (e.g., unusual joint or tendon pain, muscle weakness, a “pins and needles” tingling or pricking sensation, numbness of the arms or legs, confusion, hallucinations) while taking the drug. Advise patients to talk with a clinician if they have any questions or concerns.
-
Inform patients that systemic fluoroquinolones are associated with an increased risk of tendinitis and tendon rupture in all age groups and that this risk is increased in adults >60 years of age, individuals receiving corticosteroids, and kidney, heart, or lung transplant recipients. Symptoms may be irreversible. Importance of resting and refraining from exercise at the first sign of tendinitis or tendon rupture (e.g., pain, swelling, or inflammation of a tendon or weakness or inability to use a joint) and importance of immediately discontinuing the drug and contacting a clinician. (See Tendinitis and Tendon Rupture under Cautions.)
-
Inform patients that peripheral neuropathies have been reported in patients receiving systemic fluoroquinolones and that symptoms may occur soon after initiation of the drug and may be irreversible. Importance of immediately discontinuing delafloxacin and contacting a clinician if symptoms of peripheral neuropathy (e.g., pain, burning, tingling, numbness, and/or weakness) occur.
-
Inform patients that systemic fluoroquinolones have been associated with CNS effects (e.g., convulsions, dizziness, lightheadedness, increased intracranial pressure). Importance of informing clinician of any history of convulsions before initiating therapy with the drug. Importance of contacting a clinician if persistent headache with or without blurred vision occurs.
-
Because fluoroquinolones may cause dizziness and lightheadedness, caution patients not to engage in activities requiring mental alertness and motor coordination (e.g., driving a vehicle, operating machinery) until effects of delafloxacin on the individual are known.
-
Advise patients that systemic fluoroquinolones may worsen myasthenia gravis symptoms; importance of informing clinician of any history of myasthenia gravis. Importance of immediately contacting a clinician if any symptoms of muscle weakness, including respiratory difficulties, occur.
-
Inform patients that delafloxacin may be associated with hypersensitivity reactions (including anaphylactic reactions), even after the first dose. Importance of immediately discontinuing delafloxacin and contacting a clinician at first sign of rash, hives or other skin reaction, rapid heartbeat, difficulty swallowing or breathing, any swelling suggesting angioedema (e.g., swelling of lips, tongue, or face; throat tightness; hoarseness), jaundice, or any other sign of hypersensitivity.
-
Inform patients that systemic fluoroquinolones may increase risk of aortic aneurysm and dissection; importance of informing clinician of any history of aneurysms, blockages or hardening of the arteries, high blood pressure, or genetic conditions such as Marfan syndrome or Ehlers-Danlos syndrome. Advise patients to seek immediate medical treatment if they experience sudden, severe, and constant pain in the stomach, chest, or back.
-
Inform patients that hypoglycemia reported when systemic fluoroquinolones used in some patients receiving antidiabetic agents. Advise patients with diabetes mellitus receiving oral antidiabetic agents or insulin to discontinue fluoroquinolone treatment and contact a clinician if they experience hypoglycemia or symptoms of hypoglycemia.
-
Advise patients that diarrhea is a common problem caused by anti-infectives and usually ends when the drug is discontinued. Importance of contacting a clinician if watery and bloody stools (with or without stomach cramps and fever) occur during or as late as 2 months or longer after the last dose.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
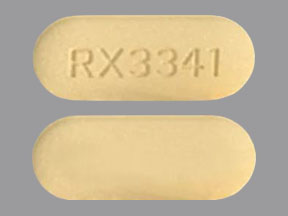
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
450 mg (of delafloxacin) |
Baxdela |
Melinta |
|
Parenteral |
For injection, for IV infusion |
300 mg (of delafloxacin) |
Baxdela |
Melinta |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions September 2, 2019. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about delafloxacin
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
- En español