Brexpiprazole (Monograph)
Brand name: Rexulti
Drug class: Atypical Antipsychotics
- Dopamine Receptor Partial Agonists
ATC class: N05AX16
VA class: CN709
Chemical name: 7-[4-(4-Benzo[b]thien-4-yl-1-piperazinyl)butoxy]-2(1H)-quinolinone
Molecular formula: C25H27N3O2S
CAS number: 913611-97-9
Warning
- Increased Mortality in Geriatric Patients with Dementia-related Psychosis
-
Geriatric patients with dementia-related psychosis treated with antipsychotic agents are at an increased risk of death.
-
Antipsychotic agents, including brexpiprazole, are not approved for the treatment of dementia-related psychosis. (See Increased Mortality in Geriatric Patients with Dementia-related Psychosis under Cautions.)
- Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults
-
Antidepressants increased risk of suicidal thoughts and behaviors compared with placebo in children, adolescents, and young adults (≤24 years of age) receiving antidepressants for major depressive disorder and other indications. (See Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults under Cautions.)
-
Safety and efficacy of brexpiprazole have not been established in pediatric patients.
Introduction
Atypical or second-generation antipsychotic agent.
Uses for Brexpiprazole
Adjunctive Therapy of Major Depressive Disorder
Adjunctive therapy to antidepressants for treatment of major depressive disorder.
Schizophrenia
Treatment of schizophrenia.
American Psychiatric Association (APA) recommends that patients with schizophrenia be treated with an antipsychotic agent and that patients whose symptoms have improved with an antipsychotic agent continue to receive such therapy. APA also suggests that patients whose symptoms have improved with an antipsychotic agent should continue to be treated with the same antipsychotic agent; however, some circumstances (e.g., patient preferences, drug availability, adverse effects) may necessitate a change in antipsychotic agent.
APA and other experts consider antipsychotic agents (i.e., first- and second-generation antipsychotic agents) first-line drugs for management of schizophrenia (including first psychotic episodes). Initial choice of an antipsychotic agent should be individualized and generally be made in the context of shared decision-making, taking into consideration multiple patient- and drug-related factors (e.g., adverse effect profiles, concurrent medical conditions or risk factors, potential for drug interactions, potential pharmacogenomic considerations, patient preferences, prior responses to treatment, available formulations, cost).
Patients who do not respond to or tolerate one antipsychotic agent may be successfully treated with another drug with different receptor binding or adverse effect profile.
Drug therapy should be used as part of a comprehensive, patient-centered treatment plan that includes evidence-based nonpharmacologic and pharmacologic treatments for schizophrenia. Consult APA’s Practice Guideline for the Treatment of Patients with Schizophrenia (at [Web]) for additional information on treatment of schizophrenia.
Brexpiprazole Dosage and Administration
General
-
Monitor for possible worsening of depression and emergence of suicidal thoughts or behaviors, especially at the beginning of therapy or during periods of dosage adjustments. (See Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults under Cautions.)
Administration
Oral Administration
Administer tablets orally once daily without regard to meals. (See Food under Pharmacokinetics.)
Dosage
If used with a CYP2D6 and/or CYP3A4 inhibitor or a CYP3A4 inducer, dosage adjustment may be required. (See Interactions.)
Adults
Adjunctive Therapy of Major Depressive Disorder
Oral
As adjunctive treatment with antidepressants, initially, 0.5 or 1 mg once daily. Increase dosage to 1 mg once daily, then up to the target dosage of 2 mg once daily. Adjust dosage at weekly intervals based on individual patient response and tolerability.
Periodically reassess need for continued therapy and appropriate dosage.
Schizophrenia
Oral
Initially, 1 mg once daily on days 1–4, followed by 2 mg once daily on days 5–7. May increase dosage to 4 mg once daily on day 8 based on individual patient response and tolerability. Recommended target dosage is 2–4 mg once daily.
In patients whose symptoms have improved, continued treatment (i.e., maintenance therapy) with an antipsychotic agent is recommended to reduce the risk of relapse. Some experts generally recommend maintenance antipsychotic therapy for at least 1–2 years after the first psychotic episode and for 2–5 years or longer following recurrent episodes. Indefinite maintenance treatment may be necessary; however, periodically assess the benefits and risks of continued antipsychotic therapy in the context of shared decision-making, taking into consideration each patient's risk of relapse, drug-associated adverse effects, course of disease, and specific goals and needs.
Prescribing Limits
Adults
Adjunctive Therapy of Major Depressive Disorder
Oral
Maximum 3 mg daily.
Schizophrenia
Oral
Maximum 4 mg daily.
Special Populations
Hepatic Impairment
Adjunctive Therapy of Major Depressive Disorder
Oral
Mild hepatic impairment: Manufacturer makes no specific dosage adjustment recommendations.
Moderate to severe hepatic impairment (Child-Pugh score ≥7): Do not exceed 2 mg once daily.
Schizophrenia
Oral
Mild hepatic impairment: Manufacturer makes no specific dosage adjustment recommendations.
Moderate to severe hepatic impairment (Child-Pugh score ≥7): Do not exceed 3 mg once daily.
Renal Impairment
Adjunctive Therapy of Major Depressive Disorder
Oral
Moderate, severe, or end-stage renal impairment (Clcr <60 mL/minute): Do not exceed 2 mg once daily.
Schizophrenia
Oral
Moderate, severe, or end-stage renal impairment (Clcr <60 mL/minute): Do not exceed 3 mg once daily.
Geriatric Patients
Cautious dosage selection recommended, usually starting at the lower end of the recommended dosage range, reflecting the greater frequency of decreased hepatic, renal, and cardiac function and concomitant illnesses and other drug therapy in this population.
Gender, Race, or Smoking Status
Dosage adjustment not required based on gender, race, or smoking status.
CYP2D6 Poor Metabolizers
Reduce brexpiprazole dosage by 50%. (See Special Populations under Pharmacokinetics.) In CYP2D6 poor metabolizers who are also taking moderate or potent CYP3A4 inhibitors, reduce brexpiprazole dosage to 25% of the usual dosage. (See Interactions.)
Cautions for Brexpiprazole
Contraindications
-
Known hypersensitivity to brexpiprazole or any components in the formulation. Rash, facial swelling, urticaria, and anaphylaxis reported.
Warnings/Precautions
Warnings
Increased Mortality in Geriatric Patients with Dementia-related Psychosis
Increased risk of death with antipsychotic agents in geriatric patients with dementia-related psychosis.
Analyses of 17 placebo-controlled trials in geriatric patients mainly receiving atypical antipsychotic agents revealed an approximate 1.6- to 1.7-fold increase in mortality compared with that in patients receiving placebo.
Most fatalities appeared to result from cardiovascular-related events (e.g., heart failure, sudden death) or infections (mostly pneumonia).
Antipsychotic agents, including brexpiprazole, are not approved for the treatment of dementia-related psychosis. (See Increased Mortality in Geriatric Patients with Dementia-related Psychosis in Boxed Warning and see Cerebrovascular Events in Geriatric Patients with Dementia-related Psychosis under Cautions.)
Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults
Antidepressants increased risk of suicidal thoughts and behaviors compared with placebo in children, adolescents, and young adults (≤24 years of age) receiving antidepressants for major depressive disorder and other indications.
Closely monitor all patients receiving antidepressants for any reason, particularly during initiation of therapy (i.e., the first few months) and during periods of dosage adjustments.
Consider changing or discontinuing therapy in patients whose depression is persistently worse or in those with emerging suicidal thoughts or behaviors.
Other Warnings and Precautions
Cerebrovascular Events in Geriatric Patients with Dementia-related Psychosis
Increased incidence of adverse cerebrovascular events (cerebrovascular accidents and TIAs), including fatalities, observed in geriatric patients with dementia treated with risperidone, aripiprazole, or olanzapine in placebo-controlled studies. The manufacturer states that brexpiprazole is not approved for the treatment of patients with dementia-related psychosis. (See Increased Mortality in Geriatric Patients with Dementia-related Psychosis in Boxed Warning.)
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome (NMS), a potentially fatal syndrome characterized by hyperpyrexia, muscle rigidity, altered mental status, and autonomic instability, reported with antipsychotic agents, including brexpiprazole.
If NMS is suspected, immediately discontinue therapy and provide intensive symptomatic treatment and monitoring.
Tardive Dyskinesia
Tardive dyskinesia, a syndrome consisting of potentially irreversible, involuntary dyskinetic movements, reported with use of antipsychotic agents.
Reserve long-term antipsychotic treatment for patients with chronic illness known to respond to antipsychotic agents, and for whom alternative, effective, but potentially less harmful treatments are not available or appropriate. In patients requiring chronic treatment, use lowest dosage and shortest duration of treatment needed to achieve a satisfactory clinical response; periodically reassess need for continued therapy.
APA recommends clinically assessing patients receiving antipsychotic agents for abnormal involuntary movements at baseline and at each follow-up visit and assessing such patients using a structured instrument (e.g., the Abnormal Involuntary Movement Scale [AIMS], Dyskinesia Identification System: Condensed User Scale [DISCUS]) at least every 6 months in patients considered at high risk for tardive dyskinesia (e.g., patients ≥55 years of age; women; individuals with a mood disorder, substance use disorder, intellectual disability, or CNS injury; individuals with high cumulative exposure to antipsychotic medications, particularly high-potency dopamine type 2 [D2] receptor antagonists; and patients who experience acute dystonic reactions, clinically significant parkinsonism, or akathisia) or at least every 12 months in other patients as well as if new onset or exacerbation of preexisting movements is observed at any follow-up visit. In some jurisdictions, the frequency of monitoring for involuntary movements in individuals receiving antipsychotic therapy may be subject to local regulations.
Consider discontinuance of brexpiprazole if signs and symptoms of tardive dyskinesia appear. However, some patients may require treatment despite presence of the syndrome.
APA recommends that patients who have moderate to severe or disabling tardive dyskinesia associated with antipsychotic therapy be treated with a vesicular monoamine transporter 2 (VMAT2) inhibitor (e.g., deutetrabenazine, valbenazine, tetrabenazine); may also consider VMAT2 inhibitor therapy in patients with mild tardive dyskinesia based on factors such as patient preference, associated impairment, and effect on psychosocial functioning.
Metabolic Changes
Atypical antipsychotic agents, including brexpiprazole, have caused metabolic changes, including hyperglycemia and diabetes mellitus, dyslipidemia, and weight gain. While all atypical antipsychotics produce some metabolic changes, each drug has its own specific risk profile. (See Hyperglycemia and Diabetes Mellitus, see Dyslipidemia, and also see Weight Gain under Cautions.)
Hyperglycemia and Diabetes Mellitus
Hyperglycemia, sometimes severe and associated with ketoacidosis, hyperosmolar coma, or death, reported in patients receiving atypical antipsychotic agents. Hyperglycemia reported in patients treated with brexpiprazole. In short-term clinical trials, clinically important differences between brexpiprazole and placebo in the proportion of patients experiencing an increase in fasting glucose concentrations from baseline to end point not observed. In longer-term clinical studies, 9–10% of patients with normal or borderline fasting glucose concentrations treated with brexpiprazole experienced shifts to high fasting glucose concentrations.
Periodically monitor patients with an established diagnosis of diabetes mellitus for worsening of glucose control and perform fasting blood glucose testing at baseline and periodically in patients with risk factors for diabetes (e.g., obesity, family history of diabetes). If manifestations of hyperglycemia occur in any brexpiprazole-treated patient, perform fasting blood glucose testing.
Some patients who developed hyperglycemia while receiving an atypical antipsychotic have required continuance of antidiabetic treatment despite discontinuance of the atypical antipsychotic; in other patients, hyperglycemia resolved with discontinuance of the antipsychotic.
Dyslipidemia
Atypical antipsychotics cause adverse alterations in lipid parameters. In short-term clinical studies, a higher incidence of hypertriglyceridemia was reported with brexpiprazole than with placebo while changes in fasting total cholesterol, LDL-cholesterol, and HDL-cholesterol were similar between brexpiprazole-treated patients and those receiving placebo. In uncontrolled, longer-term depression and schizophrenia studies, shifts to high or very high triglyceride concentrations reported in 13–17 or 0.2–0.4%, respectively, of brexpiprazole-treated patients with normal baseline triglyceride concentrations and shifts from normal to low HDL-cholesterol concentrations reported in 14% of patients in the depression studies.
Weight Gain
Weight gain observed with atypical antipsychotic therapy. Brexpiprazole generally appears to be associated with moderate weight gain; mean weight gain of 1–1.6 kg reported during short-term studies. Weight gain was ≥7% of baseline body weight in 20–30% of brexpiprazole-treated patients during longer-term studies. Manufacturer recommends monitoring of weight at baseline and frequently thereafter during therapy.
Pathological Gambling and Other Compulsive Behaviors
Postmarketing case reports suggest that patients receiving brexpiprazole may experience intense urges, particularly for gambling, and the inability to control these urges. Other compulsive urges reported include sexual urges, shopping, eating or binge eating, and other impulsive or compulsive behaviors. In some, but not all, cases, these uncontrollable urges stopped following brexpiprazole dosage reduction or drug discontinuance.
Compulsive behaviors may result in harm to the patient or others if not recognized. Because patients may not recognize such behaviors as abnormal, specifically ask patients whether they have developed any new or intense gambling urges, compulsive sexual urges, compulsive shopping, binge or compulsive eating, or other urges while receiving the drug.
If a brexpiprazole-treated patient develops new or increased impulsive or compulsive behaviors, consider reducing the dosage or discontinuing the drug. (See Advice to Patients.)
Leukopenia, Neutropenia, and Agranulocytosis
Leukopenia and neutropenia reported during therapy with antipsychotic agents. Agranulocytosis (including fatal cases) reported with other antipsychotic agents.
Possible risk factors for leukopenia and neutropenia include preexisting low WBC count or ANC or a history of drug-induced leukopenia or neutropenia. Monitor CBC frequently during the first few months of therapy in patients with such risk factors. Discontinue brexpiprazole at the first sign of a decline in WBC count in the absence of other causative factors.
Carefully monitor patients with neutropenia for signs and symptoms of infection (e.g., fever) and treat promptly if they occur. Discontinue brexpiprazole if severe neutropenia (ANC <1000/mm3) occurs; monitor WBC until recovery occurs.
Orthostatic Hypotension and Syncope
Risk of orthostatic hypotension and syncope with atypical antipsychotics, particularly during initial dosage titration and when dosage is increased, because of brexpiprazole's α1-adrenergic blocking activity.
Dizziness (2%), orthostatic hypotension (0.4%), and syncope (0.1%) reported in brexpiprazole-treated patients in short-term schizophrenia studies; dizziness (2%) and orthostatic hypotension (0.1%) reported in brexpiprazole-treated patients in short-term depression trials.
Monitor orthostatic vital signs in patients susceptible to hypotension (e.g., geriatric patients, patients with dehydration or hypovolemia, patients receiving concomitant antihypertensive therapy), patients with known cardiovascular disease (e.g., history of MI, ischemic heart disease, heart failure, or conduction abnormalities), and patients with cerebrovascular disease.
Brexpiprazole has not been evaluated in patients with a recent history of MI or unstable cardiovascular disease; such patients were excluded from premarketing clinical trials.
Falls
May cause somnolence, postural hypotension, and motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries.
In patients with diseases or conditions or receiving other drugs that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic therapy and repeat such testing periodically during long-term therapy.
Seizures
Brexpiprazole may cause seizures. Higher risk of seizures in patients with a history of seizures or with conditions that lower the seizure threshold; conditions that lower seizure threshold may be more prevalent in older patients.
Body Temperature Dysregulation
Atypical antipsychotic agents may disrupt body's ability to reduce core body temperature.
Use with caution in patients who may experience conditions that contribute to an elevation in core body temperature (e.g., strenuous exercise, extreme heat, dehydration, concomitant use of agents with anticholinergic activity).
Dysphagia
Esophageal dysmotility and aspiration associated with the use of antipsychotic agents. Use with caution in patients at risk for aspiration pneumonia.
Cognitive and Motor Impairment
Judgment, thinking, or motor skills may be impaired. Somnolence (including sedation and hypersomnia) reported in 4–5% of brexpiprazole-treated patients in short-term depression and schizophrenia trials. (See Advice to Patients.)
Specific Populations
Pregnancy
No adequate and well-controlled studies to date in pregnant women. No teratogenicity observed in animal studies, but increased perinatal deaths observed in pups at supratherapeutic dosages.
Risk for extrapyramidal and/or withdrawal symptoms (e.g., agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, feeding disorder) in neonates exposed to antipsychotic agents during the third trimester; monitor neonates exhibiting such symptoms. Symptoms were self-limiting in some neonates but varied in severity; some infants required intensive support and prolonged hospitalization.
National Pregnancy Registry for Atypical Antipsychotics: 866-961-2388 and [Web].
Lactation
Distributes into milk in rats; not known whether distributes into human milk. Effects on nursing infants and on milk production also not known.
Weigh benefits of brexpiprazole therapy to the woman and benefits of breast-feeding against potential risks of infant drug exposure.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Antidepressants may increase the risk of suicidal thoughts and behaviors in children, adolescents, and young adults. (See Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults under Cautions.)
Geriatric Use
Clinical efficacy trials of brexpiprazole did not include any patients ≥65 years of age to determine whether they respond differently than younger adults. Pharmacokinetics of the drug in geriatric patients (70–85 years of age) with depression were similar to those observed in younger adults. Manufacturer recommends cautious dosage selection in geriatric patients (see Geriatric Patients under Dosage and Administration).
Geriatric patients with dementia-related psychosis treated with either conventional or atypical antipsychotic agents are at an increased risk of death; increased incidence of cerebrovascular events also observed with certain atypical antipsychotic agents. Brexpiprazole is not approved for the treatment of patients with dementia-related psychosis. (See Boxed Warning and also see Cerebrovascular Events in Geriatric Patients with Dementia-related Psychosis under Cautions.)
Hepatic Impairment
Patients with moderate to severe hepatic impairment generally have higher brexpiprazole exposure than patients with normal hepatic function, which may increase the risk of adverse effects. Manufacturer recommends a reduction in the maximum recommended dosage in patients with moderate or severe hepatic impairment (Child-Pugh score ≥7). (See Hepatic Impairment under Dosage and Administration and also see Special Populations under Pharmacokinetics.)
Renal Impairment
Patients with moderate to severe renal impairment or end-stage renal disease generally have higher brexpiprazole exposure than patients with normal renal function, which may increase the risk of adverse effects. Manufacturer recommends a reduction in the maximum recommended dosage in patients with moderate or severe renal impairment (Clcr <60 mL/minute) or end-stage renal disease. (See Renal Impairment under Dosage and Administration and also see Special Populations under Pharmacokinetics.)
CYP2D6 Poor Metabolizers
Dosage adjustment is recommended in patients known to be poor metabolizers of CYP2D6. (See CYP2D6 Poor Metabolizers under Dosage and Administration and also see Special Populations under Pharmacokinetics.)
Common Adverse Effects
Major depressive disorder (adjunctive therapy with antidepressants): Akathisia, headache, weight gain, extrapyramidal symptoms (excluding akathisia), somnolence, nasopharyngitis, tremor, anxiety, increased appetite, dizziness, fatigue, restlessness, constipation, decreased blood cortisol concentration. Akathisia and restlessness were dose related.
Schizophrenia: Akathisia, extrapyramidal symptoms (excluding akathisia), weight gain, diarrhea, dyspepsia, tremor, increased CK concentrations, sedation.
Drug Interactions
Principally metabolized by CYP3A4 and CYP2D6.
In vitro, not a potent inhibitor or inducer of CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A4/5.
In vitro, neither a clinically relevant substrate nor inhibitor of the efflux transporters P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP), organic anion transport proteins (OATP) 1B1 and 1B3, organic anion transporter 3 (OAT3), organic cation transporter 2 (OCT2), and multidrug and toxic compound extrusion (MATE) 1 and MATE2K.
Drugs Affecting Hepatic Microsomal Enzymes
CYP3A4 and/or CYP2D6 inhibitors: Potential pharmacokinetic interaction (inhibition of brexpiprazole clearance resulting in increased systemic exposure). Reduce usual brexpiprazole dosage by 50% if used concomitantly with a potent inhibitor of CYP3A4 or CYP2D6; may resume previous brexpiprazole dosage upon discontinuance of the CYP3A4 or CYP2D6 inhibitor. Dosage adjustment not necessary when potent CYP2D6 inhibitors are used in the adjunctive treatment of major depressive disorder. In known CYP2D6 poor metabolizers, reduce usual brexpiprazole dosage by 75% if used concurrently with moderate or potent CYP3A4 inhibitors. Also reduce usual brexpiprazole dosage by 75% when given in combination with both moderate or potent CYP2D6 inhibitors and moderate or potent CYP3A4 inhibitors. May resume previous brexpiprazole dosage upon discontinuance of the CYP3A4 and/or CYP2D6 inhibitors.
Potent CYP3A4 inducers: Potential pharmacokinetic interaction (increased brexpiprazole clearance resulting in decreased systemic exposure). Double brexpiprazole dosage over 1–2 weeks during concurrent therapy. May resume usual brexpiprazole dosage over 1–2 weeks upon discontinuance of the CYP3A4 inducer.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP3A4, CYP2B6, or CYP2D6: Dosage adjustment of the CYP substrate not necessary during concurrent use.
Drugs Affecting Gastric pH
Clinically important pharmacokinetic interaction unlikely; dosage adjustment of brexpiprazole not necessary.
Protein-bound Drugs
In vitro studies suggest that protein binding of brexpiprazole not affected by concurrent administration of other highly protein-bound drugs; clinically important drug interactions because of protein displacement unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids |
Clinically important pharmacokinetic interaction unlikely with drugs that increase gastric pH |
Dosage adjustment of brexpiprazole not necessary |
|
Anticholinergic agents |
Possible disruption of body temperature regulation |
Use with caution |
|
Antifungals, azoles (e.g., fluconazole, itraconazole, ketoconazole) |
CYP3A4 inhibitors: Possible increased brexpiprazole exposure Ketoconazole (potent CYP3A4 inhibitor) increased brexpiprazole peak concentrations and AUC by approximately 1.2-fold and twofold, respectively |
Potent CYP3A4 inhibitors: Reduce brexpiprazole dosage to 50% of usual dosage (or 25% of usual dosage in patients who are CYP2D6 poor metabolizers) In combination with moderate or potent CYP2D6 inhibitors: Reduce brexpiprazole dosage to 25% of usual dosage Increase back to original brexpiprazole dosage when the CYP2D6 and/or CYP3A4 inhibitors are discontinued |
|
Bupropion |
No clinically important effect on pharmacokinetics of bupropion (CYP2B6 substrate) |
Dosage adjustment of bupropion not necessary |
|
Clarithromycin |
Possible increased brexpiprazole exposure with clarithromycin (potent CYP3A4 inhibitor) |
Reduce brexpiprazole dosage to 50% of usual dosage (or 25% of usual dosage in patients who are CYP2D6 poor metabolizers) In combination with moderate or potent CYP2D6 inhibitors: Reduce brexpiprazole dosage to 25% of usual dosage Increase back to original brexpiprazole dosage when the CYP2D6 and/or CYP3A4 inhibitors are discontinued |
|
Dextromethorphan |
No clinically important effect on pharmacokinetics of dextromethorphan (CYP2D6 substrate) |
Dosage adjustment of dextromethorphan not necessary |
|
Diazepam |
Clinically important interaction due to protein binding displacement of brexpiprazole unlikely |
|
|
Duloxetine |
Possible increased brexpiprazole exposure with duloxetine (moderate CYP2D6 inhibitor) |
In combination with moderate or potent CYP3A4 inhibitors: Reduce brexpiprazole dosage to 25% of usual dosage Increase back to original brexpiprazole dosage when the CYP2D6 and/or CYP3A4 inhibitors are discontinued |
|
Fexofenadine |
No clinically important effect on fexofenadine pharmacokinetics |
|
|
Fluoxetine |
Possible increased brexpiprazole exposure with fluoxetine (potent CYP2D6 inhibitor) |
Reduce brexpiprazole dosage to 50% of usual dosage; dosage adjustment not necessary when used as adjunctive therapy for major depressive disorder In combination with moderate or potent CYP3A4 inhibitors: Reduce brexpiprazole dosage to 25% of usual dosage Increase back to original brexpiprazole dosage when the CYP2D6 and/or CYP3A4 inhibitors are discontinued |
|
Histamine H2-receptor antagonists |
Clinically important pharmacokinetic interaction unlikely with drugs that increase gastric pH |
Dosage adjustment of brexpiprazole not necessary |
|
Hypotensive agents |
Possible additive hypotensive effects; may result in orthostatic hypotension and syncope |
Monitor orthostatic vital signs |
|
Lovastatin |
No clinically important effect on lovastatin pharmacokinetics |
Dosage adjustment of lovastatin not necessary |
|
Paroxetine |
Possible increased brexpiprazole exposure with paroxetine (potent CYP2D6 inhibitor) |
Reduce brexpiprazole dosage to 50% of usual dosage; dosage adjustment not necessary when used as adjunctive therapy for major depressive disorder In combination with moderate or potent CYP3A4 inhibitors: Reduce brexpiprazole dosage to 25% of usual dosage Increase back to original brexpiprazole dosage when the CYP2D6 and/or CYP3A4 inhibitors are discontinued |
|
Proton-pump inhibitors (e.g., omeprazole) |
Clinically important pharmacokinetic interaction unlikely with drugs that increase gastric pH Omeprazole: No clinically important effect on brexpiprazole pharmacokinetics |
Dosage adjustment of brexpiprazole not necessary |
|
Quinidine |
Quinidine (potent CYP2D6 inhibitor) increased peak concentration and AUC of brexpiprazole by approximately 1.1- and 1.9-fold, respectively |
Reduce brexpiprazole dosage to 50% of usual dosage; dosage adjustment not necessary when used as adjunctive therapy for major depressive disorder In combination with moderate or potent CYP3A4 inhibitors: Reduce brexpiprazole dosage to 25% of usual dosage Increase back to original brexpiprazole dosage when the CYP2D6 and/or CYP3A4 inhibitors are discontinued |
|
Rifampin |
Rifampin (potent CYP3A4 inducer) decreased peak concentration and AUC of brexpiprazole by 40 and 73%, respectively |
Double usual brexpiprazole dosage over 1–2 weeks during concomitant use, then adjust dosage based on clinical response Reduce brexpiprazole dosage back to original dosage over 1–2 weeks when rifampin is discontinued |
|
Rosuvastatin |
No clinically important effect on rosuvastatin pharmacokinetics |
|
|
Smoking |
Pharmacokinetic interaction unlikely |
Dosage adjustment of brexpiprazole in smokers not necessary |
|
St. John's wort (Hypericum perforatum) |
St. John's wort (potent CYP3A4 inducer) potentially can decrease peak concentration and AUC of brexpiprazole |
Double usual brexpiprazole dosage over 1–2 weeks during concomitant use, then adjust dosage based on clinical response Reduce brexpiprazole dosage back to previous dosage over 1–2 weeks when St. John's wort is discontinued |
|
Ticlopidine |
No clinically important effect on brexpiprazole pharmacokinetics |
|
|
Warfarin |
Clinically important interaction due to protein binding displacement of brexpiprazole unlikely |
Brexpiprazole Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations achieved within 4 hours following single-dose, oral administration. Exhibits dose-proportional pharmacokinetics.
Absolute oral bioavailability of tablets is 95%.
Steady-state concentrations achieved within 10–12 days.
Food
Administration with a high-fat meal does not substantially affect peak plasma concentration or AUC.
Special Populations
In patients with mild, moderate or severe renal impairment, brexpiprazole exposure was approximately 7, 71, or 72% higher, respectively, than in patients with normal renal function.
Hemodialysis not expected to affect plasma concentrations of brexpiprazole because drug is highly bound to plasma proteins.
In patients with mild, moderate, or severe hepatic impairment, brexpiprazole exposures were 26, 73, or 4% higher, respectively, than in patients with normal hepatic function.
In geriatric patients (70–85 years of age) with depression, brexpiprazole pharmacokinetics were similar to those observed in younger adults.
Higher plasma concentrations observed in CYP2D6 poor metabolizers compared with CYP2D6 extensive metabolizers.
Distribution
Extent
Large volume of distribution following IV administration indicates extravascular distribution.
Brexpiprazole distributes into milk in rats; not known whether distributes into human milk.
Plasma Protein Binding
Brexpiprazole: Highly bound (>99%) to albumin and α1-acid glycoprotein. Not affected by renal or hepatic impairment.
DM-3411 (principal metabolite): >90%.
Elimination
Metabolism
Extensively metabolized mainly by CYP3A4 and CYP2D6.
Principal metabolite (DM-3411) not likely to contribute to therapeutic effects of brexpiprazole.
Elimination Route
Following administration of a single radiolabeled dose, approximately 46% recovered in feces and 25% in urine. Approximately 14% and <1% excreted unchanged in feces and urine, respectively.
Half-life
Brexpiprazole: 91 hours.
DM-3411 (principal metabolite): 86 hours.
Stability
Storage
Oral
Tablets
20–25°C (may be exposed to 15–30°C).
Brexpiprazole Mechanism of Action
-
Exact mechanism of action in major depressive disorder and schizophrenia unknown; efficacy may be mediated through a combination of partial agonist activity at dopamine type 2 (D2) and serotonin type 1 (5-hydroxytryptamine [5-HT1A]) receptors and antagonist activity at serotonin type 2 (5-HT2A) receptors.
-
Demonstrates partial agonist activity at D2 and D3 receptors and 5-HT1A receptors and antagonist activity at 5-HT2A, 5-HT2B, and 5-HT7 receptors and α1A-, α1B-, α1D-, and α2C-adrenergic receptors.
-
Compared with aripiprazole, brexpiprazole appears to have lower intrinsic activity at D2 receptors and higher activity at 5-HT1A and 5-HT1B receptors and demonstrates stronger antagonism at 5-HT2A receptors.
-
Exhibits moderate affinity for histamine (H1) receptors, which are associated with sedation, and very low affinity for muscarinic (M1) receptors.
Advice to Patients
-
Importance of advising patients and/or caregivers to read the patient information (medication guide).
-
Importance of advising patients that brexpiprazole tablets may be taken with or without food. Importance of following dosage escalation instructions.
-
Importance of advising patients and caregivers that geriatric patients with dementia-related psychosis treated with antipsychotic agents are at an increased risk of death. Inform patients and caregivers that brexpiprazole is not approved for treating geriatric patients with dementia-related psychosis.
-
Risk of suicidal thoughts and behaviors; importance of patients, family, and caregivers being alert to and immediately reporting emergence of suicidality, especially during the first few months of therapy or during periods of dosage adjustment. (See Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults under Cautions.)
-
Importance of informing patients and caregivers about the risk of NMS; importance of immediately contacting clinician or seeking emergency medical attention if signs and symptoms of this rare but potentially life-threatening syndrome develop (e.g., high fever, muscle stiffness, sweating, fast or irregular heart beat, change in BP, confusion, kidney damage).
-
Importance of advising patients about the signs and symptoms of tardive dyskinesia. Importance of contacting a healthcare professional if abnormal muscle movements occur.
-
Importance of informing patients and caregivers about the risk of metabolic changes (e.g., hyperglycemia and diabetes mellitus, dyslipidemia, weight gain) and the need for specific monitoring for such changes. Importance of patients and caregivers being aware of the symptoms of hyperglycemia (e.g., increased thirst, increased urination, increased appetite, weakness). Importance of informing patients who are diagnosed with diabetes or those with risk factors for diabetes (e.g., obesity, family history of diabetes) that they should have their blood glucose monitored at the beginning of and periodically during brexpiprazole therapy; patients who develop symptoms of hyperglycemia during therapy should have their blood glucose assessed.
-
Risk of pathological gambling and other compulsive behaviors. Advise patients and caregivers of the possibility that they may experience compulsive urges to shop, intense urges to gamble, compulsive sexual urges, binge eating and/or other compulsive urges and the inability to control these urges during brexpiprazole therapy. In some cases, but not all, the urges reportedly stopped when the dosage was reduced or the drug was discontinued.
-
Risk of leukopenia, neutropenia, and agranulocytosis. Importance of advising patients with a preexisting low WBC count or history of drug-induced leukopenia/neutropenia that their CBC count should be monitored during brexpiprazole therapy.
-
Risk of orthostatic hypotension and syncope, especially when initiating or reinitiating treatment or increasing the dosage.
-
Importance of avoiding overheating and dehydration.
-
Risk of somnolence and impairment of judgment, thinking, or motor skills. Importance of advising patients to exercise caution when performing activities requiring mental alertness (e.g., driving, operating hazardous machinery) until they gain experience with the drug’s effects.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs or herbal supplements (see Interactions), as well as any concomitant illnesses (e.g., cardiovascular disease, diabetes mellitus, seizures).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Importance of clinicians informing patients about the benefits and risks of taking antipsychotics during pregnancy, and encouraging enrollment in the pregnancy registry (see Pregnancy under Cautions). Importance of advising patients not to stop taking brexpiprazole if they become pregnant without consulting their clinician; abruptly stopping antipsychotic agents may cause complications. Importance of informing patients about the benefits and risks of breast-feeding during brexpiprazole therapy.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
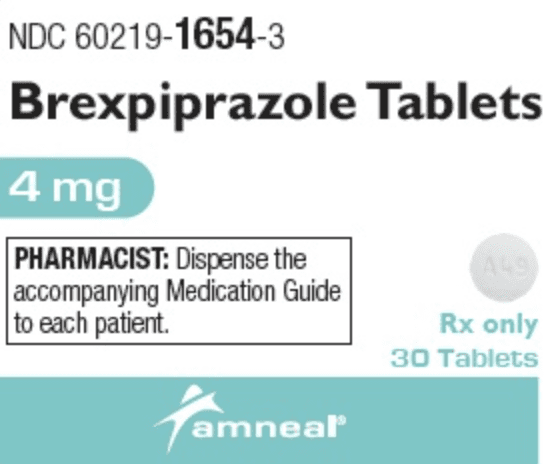
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
0.25 mg |
Rexulti |
Otsuka (also promoted by Lundbeck) |
|
0.5 mg |
Rexulti |
Otsuka (also promoted by Lundbeck) |
||
|
1 mg |
Rexulti |
Otsuka (also promoted by Lundbeck) |
||
|
2 mg |
Rexulti |
Otsuka (also promoted by Lundbeck) |
||
|
3 mg |
Rexulti |
Otsuka (also promoted by Lundbeck) |
||
|
4 mg |
Rexulti |
Otsuka (also promoted by Lundbeck) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 18, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about brexpiprazole
- Check interactions
- Compare alternatives
- Reviews (540)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: atypical antipsychotics
- Breastfeeding
- En español