Atorvastatin Calcium (Monograph)
Brand names: Atorvaliq, Lipitor
Drug class: HMG-CoA Reductase Inhibitors
Introduction
Antilipemic agent; hydroxymethylglutaryl-CoA (HMG-CoA) reductase inhibitor (i.e., statin).1 18 79
Uses for Atorvastatin Calcium
Reduction in Risk of Cardiovascular Events
Adjunct to diet and lifestyle modifications400 in adults without clinical evidence of coronary heart disease (CHD) who have multiple risk factors (e.g., age, smoking, hypertension, low HDL-cholesterol concentrations, family history of early CHD) to reduce the risk of MI, stroke, or angina and the risk of undergoing revascularization procedures.1 73 74 79
Adjunct to diet and lifestyle modifications400 in patients without clinical evidence of CHD who have type 2 diabetes mellitus and multiple risk factors to reduce the risk of MI or stroke.1 79
Adjunct to diet and lifestyle modifications400 in patients with clinical evidence of CHD to reduce the risk of nonfatal MI, fatal and nonfatal stroke, angina, or hospitalization for congestive heart failure (CHF), and the risk of undergoing revascularization procedures.1 35 53 54 58 61 66 68 71 79 81
May use in fixed combination with amlodipine when treatment with both atorvastatin (for prevention of cardiovascular events) and amlodipine (for hypertension and/or coronary artery disease) is appropriate.65
Extensive evidence demonstrates that statins can substantially reduce LDL-cholesterol concentrations and associated risk of atherosclerotic cardiovascular disease (ASCVD); may be used for secondary or primary prevention in high-risk patients.336 337 338 400
AHA/ACC cholesterol management guideline states that lifestyle modification is the foundation of ASCVD risk reduction.400 Patients with established ASCVD or high risk of ASCVD should also be treated with a statin.400
Because relative ASCVD risk reduction is correlated with degree of LDL-cholesterol lowering, use maximum tolerated intensity of a statin to achieve greatest benefit.400 High-intensity statin therapy (defined as reducing LDL-cholesterol concentrations by ≥50%) is recommended; if high-intensity statin therapy not possible (e.g., because of a contraindication or intolerable adverse effect), may consider moderate-intensity statin therapy (defined as reducing LDL-cholesterol concentrations by 30–49%).400 AHA/ACC considers atorvastatin 40–80 mg daily to be a high-intensity statin and atorvastatin 10–20 mg daily to be a moderate-intensity statin.400
The addition of a nonstatin drug (e.g., ezetimibe, PCSK9 inhibitor) to statin therapy may be considered in certain high-risk patients who require further reduction in LDL-cholesterol concentrations, particularly if there is evidence from randomized controlled studies suggesting that the addition of the nonstatin drug further reduces ASCVD events.400 403
When considering whether to initiate statin therapy for primary prevention, AHA/ACC recommends an individualized approach and shared decision making between patient and clinician.400 According to the guidelines, statin therapy may be considered in certain high-risk groups such as adults 20–75 years of age with LDL cholesterol ≥190 mg/dL, adults 40–75 years of age with diabetes mellitus, adults 40–75 years of age without diabetes mellitus but with LDL-cholesterol levels ≥70 mg/dL and an estimated 10-year ASCVD risk ≥7.5%, and adults 40–75 years of age with chronic kidney disease (CKD) (not treated with dialysis or transplantation) and LDL-cholesterol concentrations of 70–189 mg/dL who have a 10-year ASCVD risk ≥7.5%.400 401
Dyslipidemias
Adjunct to diet in adults with primary hyperlipidemia, including heterozygous familial hypercholesterolemia (HeFH) to reduce LDL-cholesterol.1 79 May use in combination with ezetimibe for additive antilipemic effects.64
Adjunct to diet to decrease elevated LDL-cholesterol in the management of HeFH in males and postmenarchal females 10–17 years of age.1 79
Adjunct to diet for the treatment of adults with primary dysbetalipoproteinemia.1 79
Adjunct to diet in the treatment of adults with hypertriglyceridemia.1 79
Reduction of elevated serum total and LDL-cholesterol concentrations in adult and pediatric patients ≥10 years of age with homozygous familial hypercholesterolemia (HoFH) as an adjunct to other lipid-lowering therapies (e.g., plasma LDL-apheresis) or when such therapies are not available.1 79 May use in combination with ezetimibe for additive antilipemic effects.64
May use in fixed combination with amlodipine when treatment with both atorvastatin (for dyslipidemias) and amlodipine (for hypertension and/or coronary artery disease) is appropriate.65
Atorvastatin Calcium Dosage and Administration
General
Pretreatment Screening
-
Obtain baseline hepatic panel in appropriate patients with chronic stable liver disease (including non-alcoholic fatty liver disease).400
-
Obtain baseline fasting lipid panel.400
Patient Monitoring
-
Perform fasting lipid panel periodically 4–12 weeks after statin initiation or dose adjustment; monitoring should continue every 3–12 months thereafter as clinically indicated.1 65 79 400
-
Periodically reinforce adherence to lifestyle modifications.400 Antilipemic therapy is an adjunct to, not a substitute for, lifestyle modification therapies that reduce the risk of ASCVD.400
-
Perform repeat liver function tests (e.g., AST, ALT, total bilirubin, alkaline phosphatase) when clinically indicated (i.e., symptoms suggesting hepatotoxicity); routine monitoring in the absence of symptoms is not recommended.1 65 79 400
-
Monitor hepatic panel in appropriate patients with chronic stable liver disease (including non-alcoholic fatty liver disease).400
-
Obtain creatine kinase (CK) levels in patients with severe statin-associated muscle weakness; routine monitoring in the absence of symptoms is not recommended.400
Administration
Oral Administration
Administer orally at the same time each day (at any time of day) without regard to meals.1 7 65 79
Atorvastatin oral suspension:Administer oral suspension on an empty stomach (1 hour before or 2 hours after a meal).79 Shake the bottle well before measuring the dose.79 Measure oral suspension using a calibrated oral syringe or other oral dosing device scored using metric units of measurements (i.e., mL).79
Atorvastatin oral tablets: Administer with or without food.1
Atorvastatin and amlodipine fixed-combination tablets: Administer with or without food.65 Do not break tablets.65
If a dose is missed, administer missed dose as soon as possible.1 65 79 If the dose was missed by more than 12 hours, do not administer the missed dose; resume medication with the next scheduled dose.1 65 79
Dosage
Available as atorvastatin calcium; dosage expressed in terms of atorvastatin.1 65 79
LDL-cholesterol-based dosage adjustment occurs ≥4 weeks after initiation and/or titration.1 79
Pediatric Patients
Dyslipidemias
Heterozygous Familial Hypercholesterolemia
OralChildren ≥10 years of age: Initially, 10 mg once daily.1 65 79 Dosage range is 10–20 mg once daily.1 65 79
Homozygous Familial Hypercholesterolemia
OralChildren ≥10 years of age: Initially, 10–20 mg once daily. 1 79 Dosage range is 10–80 mg once daily.1 79
Adults
Reduction in Risk of Cardiovascular Events
Oral
Initially, 10–20 mg once daily.1 79 Dosage range is 10–80 mg once daily.1 79
Use maximally tolerated statin intensity to achieve optimal ASCVD risk reduction.400 High-intensity statin therapy (defined as reducing LDL-cholesterol concentrations by ≥50%) is preferred; if high-intensity statin therapy not possible (e.g., because of a contraindication or intolerable adverse effect), may consider moderate-intensity statin therapy (defined as reducing LDL-cholesterol concentrations by 30–49%).400
AHA/ACC guideline panel considers atorvastatin 40–80 mg daily to be a high-intensity statin and atorvastatin 10–20 mg daily to be a moderate-intensity statin.400
Dyslipidemias
Primary Hypercholesterolemia (Heterozygous Familial and Nonfamilial) or Mixed Dyslipidemia
OralInitially, 10–20 mg once daily.1 79
Patients who require reductions of >45% in LDL-cholesterol concentration: May initiate therapy with 40 mg once daily.1 79
Usual maintenance dosage: 10–80 mg once daily.1 79
Homozygous Familial Hypercholesterolemia
OralAtorvastatin/Amlodipine Fixed-combination Tablets (Caduet and generic equivalents)
OralPatients currently receiving atorvastatin in combination with amlodipine: Use fixed combination as a substitute for the individually titrated drugs.65 Can switch to the fixed-combination preparation containing corresponding individual doses of atorvastatin and amlodipine; alternatively, can increase the dosage of one or both components for additional antilipemic, antianginal, and/or antihypertensive effects.65 Maximum dosage of atorvastatin or amlodipine in the fixed-combination preparation is 80 or 10 mg daily, respectively.65
Dosage Modification for Concomitant Therapy
Saquinavir plus ritonavir, darunavir plus ritonavir, fosamprenavir, fosamprenavir plus ritonavir, elbasvir plus grazoprevir or letermovir:Maximum atorvastatin dosage: 20 mg once daily.1 65 79
Nelfinavir: Maximum atorvastatin dosage: 40 mg once daily.1 65 79
Clarithromycin: Maximum atorvastatin dosage: 20 mg once daily.1 65 79
Itraconazole: Maximum atorvastatin dosage: 20 mg once daily.1 65 79
Special Populations
Hepatic Impairment
No specific dosage recommendations.1 79 Contraindicated in patients with acute liver failure or decompensated cirrhosis.1 79 Use with caution in patients who consume substantial amounts of alcohol and/or have a history of liver disease.1 79
Renal Impairment
Dosage modification not required.1 79 Monitor for development of myopathy.1 79
Geriatric Patients
No specific dosage recommendations; however, use with caution.1
Pharmacogenomic Considerations
SLCO1B1 decreased or possible decreased function phenotype: Initial dosage ≤40 mg once daily recommmended.500
SLCO1B1 poor function phenotype: Initial dosage ≤20 mg once daily recommmended.500
Cautions for Atorvastatin Calcium
Contraindications
-
Known hypersensitivity to atorvastatin or any component in the formulation.1 79 Anaphylaxis, angioneurotic edema, erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis, have been reported.1 79
-
Atorvastatin and amlodipine fixed-combination tablets: Pregnancy, lactation, and active liver disease, which may include unexplained persistent elevations in hepatic transaminase levels.65
Warnings/Precautions
Musculoskeletal Effects
Myopathy (defined as muscle pain, tenderness, or weakness in conjunction with CK concentration increases) reported.1 79
Rhabdomyolysis with acute renal failure secondary to myoglobinuria reported; rare fatalities have occurred.1 79
Risk of myopathy or rhabdomyolysis increased in geriatric patients (≥65 years of age), in patients with uncontrolled hypothyroidism or renal impairment, and those receving a higher dosage.1 79
Certain drug or food interactions also may increase risk of myopathy and/or rhabdomyolysis.1 79
AHA/ACC recommends measurement of CK levels in patients with severe statin-associated muscle symptoms; however, routine monitoring is not useful.400
Discontinue therapy if serum CK concentrations become markedly elevated or if myopathy is diagnosed or suspected.1 79 Muscle symptoms and CK elevations may resolve following discontinuance.1 79
Temporarily withhold or discontinue therapy in any patient experiencing an acute, serious condition suggestive of myopathy or predisposing to the development of renal failure secondary to rhabdomyolysis (e.g., sepsis; severe hypovolemia; major surgery; trauma; severe metabolic, endocrine, or electrolyte disorders; uncontrolled seizures).1 79
Immune-Mediated Necrotizing Myopathy
Immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, reported rarely in patients receiving statins.1 79 Recurrence reported when the same or a different statin was administered.1 79
Characterized by proximal muscle weakness and elevated CK concentrations that persist despite discontinuance of statin therapy, positive anti-HMG CoA reductase antibody, muscle biopsy showing necrotizing myopathy, and improvement following therapy with immunosuppressive agents.1 79
Additional neuromuscular and serologic testing may be necessary; treatment with immunosuppressive agents may be required.1 79
Discontinue if IMNM suspected.1 79
Hepatic Effects
Increases in serum aminotransferase (AST, ALT) concentrations reported.1 79 Concentrations returned to or near pretreatment levels following dosage reduction or therapy interruption or discontinuance.1 79
Fatal and nonfatal hepatic failure reported rarely.1
Consider liver enzyme tests before initiation of therapy and as clinically indicated.1 79 Serious statin-related liver injury is rare and unpredictable, and routine periodic monitoring of liver enzymes does not appear to be effective in detecting or preventing serious liver injury.200 AHA/ACC cholesterol management guideline states that it is reasonable to obtain liver function tests in patients with symptoms of hepatotoxicity (e.g., unusual fatigue or weakness, loss of appetite, abdominal pain, dark colored urine, yellowing of skin or sclera); however, routine monitoring not recommended.400 \
If serious liver injury with clinical manifestations and/or hyperbilirubinemia or jaundice occurs, promptly interrupt atorvastatin therapy.1 79
Use with caution in patients who consume substantial amounts of alcohol and/or have a history of liver disease.1 79 Contraindicated in patients with acute liver failure or decompensated cirrhosis.1 79
Hyperglycemic Effects
Increases in HbA1c and fasting serum glucose concentrations reported.1 79 200 Possible increased risk of developing diabetes.200
AHA/ACC cholesterol management guideline states that in patients with increased risk of diabetes mellitus or new-onset diabetes mellitus, statin therapy and lifestyle modifications should be continued to reduce risk of ASCVD.400
Use in Patients with Recent Stroke or TIA
In hypercholesterolemic patients without clinically evident CHD who had a stroke or TIA within the past 1–6 months, long-term (median of 4.9 years) therapy with high-dose atorvastatin (80 mg daily) associated with higher incidence of hemorrhagic stroke compared with placebo.1 73 79 Risk is increased in patients with history of hemorrhagic or lacunar stroke.1 79 Weigh benefits against potential risks in patients with recent hemorrhagic stroke.1 79
Use of Fixed Combinations
When used in fixed combination with amlodipine, consider cautions, precautions, contraindications, and interactions associated with amlodipine.65
Specific Populations
Pregnancy
All statins were previously contraindicated in pregnant females because fetal risk was thought to outweigh any possible benefit.405 However, the totality of evidence to date indicates limited potential for statins to cause malformations and other adverse embryofetal effects; FDA has therefore requested removal of the contraindication.405 Most pregnant patients should still discontinue statins because of the possibility of fetal harm; however, some patients (e.g., those with homozygous familial hypercholesterolemia or established cardiovascular disease) may benefit from continued therapy.400 402 405 Consider patient's individual risks and benefits.402 405
Patients who become pregnant or suspect that they are pregnant while receiving a statin should notify their clinician; clinician should advise patient on the appropriate course of action.405
Increased risk of miscarriage reported in pregnant women exposed to statins; however, not clear whether drug-related or due to other confounding factors.400 405
Lactation
Distributed into milk in rats; may distribute into milk in humans.1 79 Use is not recommended in nursing females; females who require atorvastatin therapy should not breast-feed their infants.1 79 Many patients can stop statin therapy temporarily until breast-feeding is complete; patients who require ongoing statin treatment should not breast-feed and should use alternatives such as infant formula.400 402 405
Females and Males of Reproductive Potential
AHA/ACC cholesterol management guideline states females (including adolescents) of childbearing age who are sexually active should be counseled to use a reliable form of contraception.400
Pediatric Use
Safety and efficacy not established in children <10 years of age with heterozygous- or homozygous familial hypercholesterolemia, or in children with other types of hyperlipidemia.1 79
Safety and efficacy of atorvastatin in fixed combination with amlodipine not established in children; effect of the amlodipine component on blood pressure in children <6 years of age not known.65
Geriatric Use
No overall differences in efficacy or safety relative to younger adults.1 79
Use with caution, since age ≥65 years is a predisposing factor for myopathy.1 79
Select dosage with caution; monitor for increased risk of myopathy.1 79
Patients >75 years of age may have a higher risk of adverse effects and lower adherence to therapy; consider expected benefits versus adverse effects before initiating statin therapy in this population.400
Safety and efficacy of atorvastatin in fixed combination with amlodipine not established in geriatric patients.65
Hepatic Impairment
Use with caution in patients who consume substantial amounts of alcohol and/or have a history of liver disease.1 79
Contraindicated in patients with acute liver failure or decompensated cirrhosis.1 79
Renal Impairment
Dosage modification not necessary in patients with renal impairment.1 79 However, monitor more closely for development of myopathy, since history of renal impairment may be a risk factor for development of rhabdomyolysis.1
Studies have not been conducted in patients with end-stage renal disease (ESRD); hemodialysis not expected to substantially enhance clearance since atorvastatin is extensively bound to plasma proteins.1 79
Pharmacogenomic Considerations
Genetic variation in the solute carrier organic anion transporter (SLCO) family member (SLCO1B1), ABCG2 (also known as breast cancer resistance protein [BCRP]), and CYP2C9 genes alter systemic exposure to statins, which can increase the risk for statin-associated musculoskeletal symptoms.500
In patients with phenotypes that result in increased statin exposure, consider potential for other patient-specific issues that may increase statin exposure (e.g., renal and hepatic function, drug-drug interactions).500
Experts state statin therapy should neither be discontinued nor avoided based on SLCO1B1, ABCG2, or CYP2C9 genotype results for patients with an indication for statin therapy.500
Patients with solute carrier organic anion transporter SLCO1B1 decreased, possible decreased, or poor function phenotypes will have increased exposure and risk of statin-associated musculoskeletal symptoms.500 Lower doses or an alternative statin may be required.500
Common Adverse Effects
Common adverse effects (≥5%): Nasopharyngitis, arthralgia, diarrhea, pain in extremity, urinary tract infection.1 79
Drug Interactions
Substrate of P-gp, BCRP, and organic anion transporter protein (OATP) 1B1/1B3.1 79 339 501 502
When used in fixed combination with amlodipine, consider interactions associated with amlodipine.65 No formal drug interaction studies to date with fixed-combination preparation.65
Drugs and Foods Affecting Hepatic Microsomal Enzymes
Inhibitors of CYP3A4: Potential pharmacokinetic interaction (variable increases in plasma atorvastatin concentrations); increased risk of myopathy or rhabdomyolysis.1 79
Inducers of CYP3A4: Potential pharmacokinetic interaction (variable reductions in plasma atorvastatin concentrations).1 79
Drugs Affecting or Affected by Transport Systems
Inhibitors of OATP1B1, OAT1B3, P-gp, and BCRP: Potential pharmacokinetic interaction (increased bioavailability of atorvastatin); increased risk of myopathy or rhabdomyolysis.1 79
Specific Drugs and Foods
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amlodipine |
||
|
Antacids |
Decreased atorvastatin peak plasma concentrations and AUC1 79 |
|
|
Antifungals, azoles |
Increased risk of myopathy or rhabdomyolysis1 79 Itraconazole: Increased atorvastatin peak plasma concentration and AUC1 79 |
Weigh benefits against risks of concomitant use; carefully monitor for signs and symptoms of myopathy, particularly during initial months of therapy and following an increase in dosage of either drug1 79 Itraconazole: Do not exceed atorvastatin dosage of 20 mg daily1 79 |
|
Bile acid sequestrants |
Additive cholesterol-lowering effects20 Decreased absorption of atorvastatin505 |
Administer statins 1 hour before or 4 hours after the bile acid sequestrant505 |
|
Cimetidine |
Atorvastatin peak plasma concentration decreased; no change in AUC1 79 |
|
|
Colchicine |
Monitor for signs and symptoms of myopathy, particularly during initiation and upward dose titration1 79 |
|
|
Cyclosporine |
Increased atorvastatin peak plasma concentration and AUC; increased risk of myopathy or rhabdomyolysis1 79 339 |
Concomitant use not recommended1 79 Experts state dosages up to 10 mg may be considered with close monitoring for signs or symptoms of muscle-related toxicity339 502 |
|
Digoxin |
Increased peak plasma digoxin concentrations and AUC1 79 339 |
|
|
Diltiazem |
Increased atorvastatin AUC; no change in peak plasma concentration1 79 |
|
|
Elvitegravir, cobicistat-boosted |
Increased atorvastatin peak plasma concentration and AUC503 |
Experts recommend careful atorvastatin titration to lowest effective dosage and monitor for adverse effects; do not exceed 20 mg once daily503 |
|
Efavirenz |
Experts recommend atorvastatin dose adjustment based on clinical response; do not exceed maximum dosage503 |
|
|
Etravirine |
Possible reduction in atorvastatin AUC503 |
Experts recommend atorvastatin dose adjustment based on clinical response; do not exceed maximum dosage503 |
|
Fibric acid derivatives (e.g., fenofibrate, gemfibrozil) |
Increased risk of myopathy1 79 Fenofibrate: Slight increase in atorvastatin AUC79 |
Gemfibrozil: Concomitant use not recommended1 79 Other fibric acid derivatives (e.g., fenofibrate): Use concomitantly with caution and only if benefits outweigh risks; carefully monitor for signs and symptoms of myopathy, particularly during initial months of therapy and following an increase in dosage of either drug1 79 |
|
Grapefruit juice |
Increased atorvastatin peak plasma concentration and AUC; increased risk of myopathy or rhabdomyolysis1 79 |
|
|
HCV Antivirals |
Glecaprevir and pibrentasvir: Atorvastatin peak plasma concentrations and AUCincreased substantially1 79 Elbasvir and grazoprevir: Atorvastatin peak plasma concentrations and AUC increased1 79 Ledipasvir and sofosbuvir: Cases of myopathy and/or rhabdomyolysis reported79 |
Glecaprevir and pibrentasvir: Concomitant use not recommended1 79 Elbasvir and grazoprevir: Do not exceed atorvastatin dosage of 20 mg daily1 79 Ledipasvir and sofosbuvir: Use concomitantly with caution and only if benefits outweigh risks; carefully monitor for signs and symptoms of myopathy, particularly during initial months of therapy and following an increase in dosage of either drug1 |
|
HIV protease inhibitors |
Increased atorvastatin peak plasma concentration and AUC; increased risk of myopathy or rhabdomyolysis1 79 503 |
Weigh benefits against risks of concomitant use; carefully monitor for signs and symptoms of myopathy, particularly during initial months of therapy and following an increase in dosage of either drug1 79 Atazanavir, with or without ritonavir: Experts recommend atorvastatin titration to the lowest effective dosage; monitor for adverse effects503 Cobicistat-boosted atazanavir: Avoid concomitant use503 Ritonavir-boosted darunavir, cobicistat-boosted darunavir, fosamprenavir or ritonavir-boosted fosamprenavir, or ritonavir-boosted saquinavir: Use concomitantly with caution; do not exceed atorvastatin dosage of 20 mg daily1 79 503 Lopinavir/ritonavir: Use concomitantly with caution; use lowest necessary dosage of atorvastatin; experts recommend 20 mg daily maximum dosage1 79 502 503 Nelfinavir: Monitor closely; do not exceed atorvastatin dosage of 40 mg daily1 79 |
|
Lenacapavir |
Atorvastatin exposure may be increased503 |
Experts state no dosage adjustment necessary503 |
|
Letermovir |
Increased atorvastatin peak plasma concentration and AUC1 79 |
|
|
Lomitapide |
Increased peak plasma concentration and AUC of atorvastatin acid374 Increased lomitapide peak plasma concentration and AUC374 |
Adjustment of atorvastatin dosage not required; however, do not exceed lomitapide dosage of 30 mg daily374 |
|
Macrolides (i.e., clarithromycin, erythromycin) |
Clarithromycin, erythromycin: Increased atorvastatin peak plasma concentration and AUC; increased risk of myopathy or rhabdomyolysis1 79 |
Weigh benefits against risks of concomitant use; carefully monitor for signs and symptoms of myopathy, particularly during initial months of therapy and following an increase in dosage of either drug1 79 Clarithromycin: Do not exceed atorvastatin dosage of 20 mg daily1 79 |
|
Nevirapine |
Decreased atorvastatin exposure503 |
Experts recommend atorvastatin dosage adjustment based on clinical response; do not exceed maximum dosage503 |
|
Niacin (antilipemic dosages [≥1 g daily]) |
Weigh benefits against risks of concomitant use1 79 Use concomitantly with caution; consider using lower initial and maintenance dosages of atorvastatin; carefully monitor patients for signs and symptoms of myopathy, particularly during initial months of atorvastatin therapy or following an increase in dosage of either drug1 79 |
|
|
Omega-3-acid ethyl esters |
No effect on rate or extent of exposure to atorvastatin, 2-hydroxyatorvastatin, or 4-hydroxyatorvastatin at steady state505 |
|
|
Oral contraceptives |
Increased peak plasma concentrations and AUC of ethinyl estradiol and norethindrone1 79 |
|
|
Rifampin |
Variable effects on plasma atorvastatin concentrations; delayed administration of atorvastatin following administration of rifampin associated with substantial reductions in plasma atorvastatin concentrations1 |
|
|
Warfarin |
Some experts recommend closer monitoring of INR when statin therapy is initiated or adjusted339 |
Atorvastatin Calcium Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following oral administration; undergoes extensive first-pass metabolism in the liver.1 79
Peak plasma concentrations attained at 1–2 hours.1 79
Absolute bioavailability is approximately 14%.1 79 Systemic availability of HMG-CoA reductase inhibitory activity approximately 30%.1 79
Evening administration associated with a decrease in the extent of absorption; however, antilipemic activity remains unchanged.1 79
Onset
Therapeutic response usually is apparent within 2 weeks; maximal response occurs within 4 weeks.1 79
Food
Atorvastatin tablets: Food decreases rate and extent of absorption but does not alter antilipemic effects.1
Atorvastatin oral suspension: High fat meal decreases AUC and peak plasma concentration; administer on an empty stomach (1 hour before or 2 hours after a meal).79
Distribution
Extent
Statins are distributed mainly to the liver.1
Distributes into milk in rats; may distribute into human milk.1 79
Plasma Protein Binding
Elimination
Metabolism
Extensively metabolized in the liver,1 mainly by CYP3A4, to active metabolites.1 79
Elimination Route
Excreted principally in feces; <2% of a dose excreted in urine.1 79
Half-life
Approximately 14 hours.1
Special Populations
Hepatic impairment (Child-Pugh class A and B) or alcoholic liver disease: Markedly increased concentrations.1 79
Renal impairment: No effect on plasma concentrations or antilipemic effect.1 79
Geriatric patients: Peak plasma concentration and AUC are 40 and 30% higher, respectively, in geriatric individuals (≥65 years of age) compared with younger adults.1 79
Pediatric patients: Clearance similar to that of adults when scaled allometrically by body weight.1 79
Females have slightly increased peak plasma concentrations and AUC; not clinically significant.1 79
Stability
Storage
Oral
Suspension
20–25°C; excursions permitted to 15–30°C.79 Store and dispense in the original bottle.79 Use within 60 days of first opening the bottle; discard any remainder.79
Tablets
Atorvastatin: 20–25°C.1
Atorvastatin/amlodipine fixed combination: 25°C (excursions permitted to 15–30°C).65
Actions
-
Selectively and competitively inhibits HMG-CoA reductase, causing subsequent reductions in hepatic cholesterol synthesis.1 501 Reduces serum concentrations of total cholesterol, LDL-cholesterol, apo B, triglycerides, VLDL-cholesterol, IDL-cholesterol, and non-HDL-cholesterol, and increases serum concentrations of HDL-cholesterol and apo A-1.1 5 24
-
Other favorable (pleiotropic) effects include an antiproliferative influence on smooth muscle cells, reconstruction of endothelial activity, and antioxidant, antithrombotic, anticancer, and anti-inflammatory effects.501
Advice to Patients
-
Advise patients of the importance of adhering to nondrug therapies and measures, including adherence to a heart-healthy diet, regular exercise, avoidance of tobacco products, and maintenance of a healthy weight.1 79 400
-
Stress importance of periodic monitoring of lipoprotein profile to determine goal attainment.1 79
-
Advise patients of the risk of myopathy and/or rhabdomyolysis; risk is increased with higher dosages, when consuming large quantities of grapefruit juice, or when used concomitantly with certain drugs.1 Stress importance of patients promptly reporting any unexplained and/or persistent muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever, or if manifestations persist after discontinuance of therapy.1
-
Advise patients of the risk of adverse hepatic effects.1 Stress importance of promptly reporting any symptoms suggestive of liver injury (e.g., fatigue, anorexia, right upper abdominal discomfort, dark urine, jaundice).1 79
-
Advise patients of the risk of increased glucose concentrations and development of type 2 diabetes.1
-
Advise patients that atorvastatin should be administered at the same time each day, at any time of day.1
-
Advise patients that atorvastatin tablets may be administered with or without food.1
-
Advise patients that atorvastatin oral suspension should be administered on an empty stomach (1 hour before or 2 hours after a meal).79 Advise patients to shake the bottle of atorvastatin oral suspension before measuring the dose with a calibrated oral dosing syringe or other oral dosing device scored using metric units of measurements (i.e., mL).79
-
Advise patients that the fixed-combination preparation containing atorvastatin and amlodipine (Caduetand generic equivalents) should be administered as a whole tablet with or without food at the same time each day, at any time of day.65 Do not break the tablet before administration.65
-
If a dose of atorvastatin tablets, oral suspension, or the fixed-combination preparation containing atorvastatin and amlodipine is missed, advise patients to take the missed dose as soon as possible.1 65 79 If it has been more than 12 hours since the missed dose, advise patients to wait and take the dose at the next scheduled time; do not double the next dose.1 65 79
-
Advise females of reproductive potential (including adolescents) of the risk to a fetus and to use effective contraception during treatment.400 Advise females to contact their clinician if they become pregnant or suspect pregnancy during therapy405
-
Advise females not to breastfeed during therapy.1
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.1
-
Inform patients of other important precautionary information.1
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Suspension |
4 mg (of atorvastatin) per mL* |
Atorvastatin Calcium Suspension |
|
|
Atorvaliq |
CMP Pharma |
|||
|
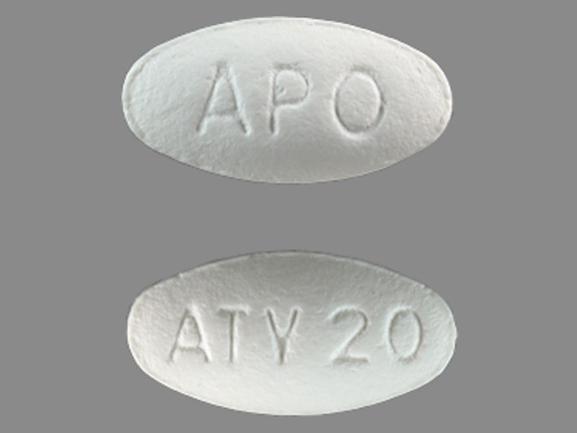
Tablets, film-coated |
10 mg (of atorvastatin)* |
Atorvastatin Calcium Tablets |
||
|
Lipitor |
Pfizer |
|||
|
20 mg (of atorvastatin)* |
Atorvastatin Calcium Tablets |
|||
|
Lipitor |
Pfizer |
|||
|
40 mg (of atorvastatin)* |
Atorvastatin Calcium Tablets |
|||
|
Lipitor |
Pfizer |
|||
|
80 mg (of atorvastatin)* |
Atorvastatin Calcium Tablets |
|||
|
Lipitor |
Pfizer |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
10 mg (of atorvastatin) with Amlodipine Besylate 2.5 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|
|
Caduet |
Pfizer |
|||
|
10 mg (of atorvastatin) with Amlodipine Besylate 5 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
10 mg (of atorvastatin) with Amlodipine Besylate 10 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
20 mg (of atorvastatin) with Amlodipine Besylate 2.5 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
20 mg (of atorvastatin) with Amlodipine Besylate 5 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
20 mg (of atorvastatin) with Amlodipine Besylate 10 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
40 mg (of atorvastatin) with Amlodipine Besylate 2.5 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
40 mg (of atorvastatin) with Amlodipine Besylate 5 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
40 mg (of atorvastatin) with Amlodipine Besylate 10 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
80 mg (of atorvastatin) with Amlodipine Besylate 5 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
|||
|
80 mg (of atorvastatin) with Amlodipine Besylate 10 mg (of amlodipine)* |
Atorvastatin Calcium and Amlodipine Besylate Tablets |
|||
|
Caduet |
Pfizer |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
Only references cited for selected revisions after 1984 are available electronically.
1. Pfizer. Lipitor (atorvastatin calcium) tablets prescribing information. New York, NY; 2022 Dec.
5. Kastelein JJP, Isaacsohn JL, Ose L et al. Comparison of effects of simvastatin versus atorvastatin on high-density lipoprotein cholesterol and apolipoprotein A-I levels. Am J Cardiol. 2000; 86:221-3. https://pubmed.ncbi.nlm.nih.gov/10913488
7. Lea AP, McTavish D. Atorvastatin: A review of its pharmacology and therapeutic potential in the management of hyperlipidaemias. Drugs. 1997;53(5):828-847. https://pubmed.ncbi.nlm.nih.gov/9129869
9. McKenney JM, McCormick LS, Weiss S et al. A randomized trial of the effects of atorvastatin and niacin in patients with combined hyperlipidemia or isolated hypertriglyceridemia. Am J Med. 1998;104:137-43. https://pubmed.ncbi.nlm.nih.gov/9528731
10. Ooi TC, Heinonen T, Alaupovic P, et al. Efficacy and safety of a new hydroxymethylglutaryl-coenzyme A reductase inhibitor, atorvastatin, in patients with combined hyperlipidemia: comparison with fenofibrate. Arterioscler Thromb Vasc Biol. 1997;17:1793-9. https://pubmed.ncbi.nlm.nih.gov/9327779
12. Heinonen T, Stein E, Issacsohn J, et al. Atorvastatin in the treatment of severe hypercholesterolemia. In: 66th Congress of the European Atherosclerosis Society Abstract Book: 1996 July 13-17, Florence Italy, 214. Abstract.
13. Bakker-Arkema RG, Davidson MH, Goldstein RJ, et al. Efficacy and safety of a new HMG Co-A reductase inhibitor, atorvastatin, in patients with hypertriglyceridemia. JAMA. 1996;275:128-33.
15. Heinonen T, Black D. Atorvastatin monotherapy and combination therapy in the treatment of severe hypercholesterolemia. Atherosclerosis. 1995;115 (Suppl):S20. Abstract.
16. Bairaktari ET, Tzallas CS, Tsimihodimos VK, et al. Comparison of the efficacy of atorvastatin and micronized fenofibrate in the treatment of mixed hyperlipidemia. J Cardiovasc Risk. 1999;6:113-6. https://pubmed.ncbi.nlm.nih.gov/10353071
17. Hunninghake D, Bakker-Arkema RG, Wigand JP, et al. Treating to meet NCEP-recommended LDL-cholesterol concentrations with atorvastatin, fluvastatin, lovastatin, or simvastatin in patients with risk factors for coronary heart disease. J Fam Pract. 1998;47(5):349-56. https://pubmed.ncbi.nlm.nih.gov/9834769
18. Nawrocki JW, Weiss SR, Davidson MH, et al. Reduction of LDL-C cholesterol by 25% to 60% in patients with primary hypercholesterolemia by atorvastatin, a new HMG-CoA reductase inhibitor. Arterioscler Thromb Vasc Biol. 1995;15:678-82. https://pubmed.ncbi.nlm.nih.gov/7749881
19. Heinonen TM, Stein F, Weiss SR, et al. The lipid lowering effects of atorvastatin, a new HMG-CoA reductase inhibitor: results of a randomized, double-masked study. Clin Ther. 1996;18(5):853-63. https://pubmed.ncbi.nlm.nih.gov/8930429
20. Heinonen TM, Schrott H, McKenney JM, et al. Atorvastatin, a new HMG-CoA reductase inhibitor as monotherapy and combined with colestipol. J Cardiovasc Pharmacol Therapeut. 1996;1(2):117-22.
21. Murillas J, Martin T, Ramos A et al. Atorvastatin for protease inhibitor-related hyperlipidaemia. AIDS. 1999; 13:1424-5. https://pubmed.ncbi.nlm.nih.gov/10449305
22. Witzum JL. Drugs used in the treatment of hyperlipoproteinemias. In: Hardman JG, Limbird LE, Molinoff PB et al eds. Goodman and Gilman’s the pharmacological basis of therapeutics. 9th ed. New York: McGraw-Hill; 1996:875-97.
23. McVey D, Patel H, Eminton Z et al. An assessment of the efficacy of atorvastatin in treating patients with dyslipidaemia to target LDL-cholesterol goals: the atorvastatin matrix study. Int J Clin Pract. 1999; 53:509-13. https://pubmed.ncbi.nlm.nih.gov/10692735
24. Wierzbicki AS, Lumb PJ, Crook MA et al. Comparison of therapy with simvastatin 80 mg and atorvastatin 80 mg in patients with familial hypercholesterolaemia. Int J Clin Pract. 1999; 53:609-11. https://pubmed.ncbi.nlm.nih.gov/10692755
25. Cilla DD, Gibson DM, Whitfield LR, et al. Pharmacodynamic effects and pharmacokinetics of atorvastatin after administration to normocholesterolemic subjects in the morning and evening. J Clin Pharmacol. 1996;36:604-9. https://pubmed.ncbi.nlm.nih.gov/8844442
26. Crouse JR, Frohlich J, Ose L, et al. Effects of high doses of simvastatin and atorvastatin on high-density lipoprotein cholesterol and apolipoprotein A-I. Am J Cardiol. 1999;83:1476-80. https://pubmed.ncbi.nlm.nih.gov/10335764
27. Dart A, Jerums G, Nicholson G, et al. A multicenter, double-blind, one year study comparing safety and efficacy of atorvastatin versus simvastatin in patients with hypercholesterolemia. Am J Cardiol. 1997;80:39-44. https://pubmed.ncbi.nlm.nih.gov/9205017
28. Raal FJ, Pilcher GJ, Veller MG et al. Efficacy of vitamin E compared with either simvastatin or atorvastatin in preventing the progression of atherosclerosis in homozygous familial hypercholesterolemia. Am J Cardiol. 1999; 84:1344-6. https://pubmed.ncbi.nlm.nih.gov/10614803
30. Davidson MM, McKenney JM, Stein EA, et al. Comparison of one-year efficacy and safety of atorvastatin versus lovastatin in primary hypercholesterolemia. Am J Cardiol. 1997;79:1475-1481. https://pubmed.ncbi.nlm.nih.gov/9185636
31. Stern R, Yang B, Horton M, et al. Renal dysfunction does not alter the pharmacokinetics or low density lipoprotein concentration reduction of atorvastatin. J Clin Pharmacol. 1997;37(9):816-9. https://pubmed.ncbi.nlm.nih.gov/9549635
32. Gibson DM, Yang BB, Abel RB, et al. Effects of hepatic and renal impairment on pharmacokinetics (pk) and pharmacodynamics (pd) of atorvastatin (abstract). Pharm Res. 1996;13(suppl):428S.
35. Waters DD. Medical therapy versus revascularization: the atorvastatin versus revascularization treatment AVERT trial. Can J Cardiol. 2000; 16(suppl A):11-3A.
36. Farnier M, Portal JJ, Maigret P. Efficacy of atorvastatin compared with simvastatin in patients with hypercholesterolemia. J Cardiovasc Pharmacol Therapeut. 2000; 5:27-31.
40. Raal FJ, Pappu AS, Illingworth DR et al. Inhibition of cholesterol synthesis by atorvastatin in homozygous familial hypercholesterolaemia. Atherosclerosis. 2000; 150:421-8. https://pubmed.ncbi.nlm.nih.gov/10856535
44. Japan Cholesterol Lowering Atorvastatin Study (J-CLAS) Group. Efficacy of atorvastatin in primary hypercholesterolemia. Am J Cardiol. 1997;79:1248-51. https://pubmed.ncbi.nlm.nih.gov/9164896
45. Marais AD, Naoumova RP, Firth JC, et al. Decreased production of low density lipoprotein by atorvastatin after apheresis in homozygous familial hypercholesterolemia. J Lipid Res. 1997;38:2071-78. https://pubmed.ncbi.nlm.nih.gov/9374129
51. Jones P, Kafonek S, Laurora I, et al. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (The CURVES Study). Am J Cardiol. 1998;81:582-587. https://pubmed.ncbi.nlm.nih.gov/9514454
52. Brown AS, Bakker-Arkema RG, Yellen L, et al. Treating patients with documented atherosclerosis to National Cholesterol Education Program-recommended low-density-lipoprotein cholesterol goals with atorvastatin, fluvastatin, lovastatin, and simvastatin. J Am Coll Cardiol. 1998;32(3):665-72. https://pubmed.ncbi.nlm.nih.gov/9741509
53. McCormick L, Black DM, Waters D, et al. Rationale, design, and baseline characteristics of a trial comparing aggressive lipid lowering with atorvastatin versus revascularization treatments (AVERT). Am J Cardiol. 1997;80:1130-33. https://pubmed.ncbi.nlm.nih.gov/9359537
54. Pitt B, Waters D, Brown WV, et al. Aggresive lipid-lowering therapy compared with angioplasty in stable coronary artery disease. N Engl J Med. 1999;341(2):70-76. https://pubmed.ncbi.nlm.nih.gov/10395630
56. Bertolini S, Bon GB, Campbell LM, et al. Efficacy and safety of atorvastatin compared to pravastatin in patients with hypercholesterolemia. Atherosclerosis. 1997;130:191-7. https://pubmed.ncbi.nlm.nih.gov/9126664
57. Brown MS, Goldstein JL. Lipoprotein receptors in the liver: control signals for plasma cholesterol traffic. J Clin Invest. 1983;72:743-7. https://pubmed.ncbi.nlm.nih.gov/6309907
58. Goldstein JL, Brown MS. The low-density lipoprotein pathway and its relation to atherosclerosis. Ann Rev Biochem. 1977; 46:897-930. https://pubmed.ncbi.nlm.nih.gov/197883
61. Schwartz GG, Olsson AG, Ezekowitz MD et al for the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) study investigators. JAMA. 2001;285:1711-8.
62. Anon. Choice of lipid-regulating drugs. Med Lett Drugs Ther. 2001; 43:43-8. https://pubmed.ncbi.nlm.nih.gov/11378632
64. Organon. Zetia (ezetimibe) tablets prescribing information.Jersey City, NJ; 2024 Feb.
65. Pfizer Labs. Caduet (amlodipine besylate/atorvastatin calcium) tablets prescribing information. New York, NY; 2023 Oct.
66. Cannon CP, Braunwald E, McCabe CH et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004; 350: 1495-504. https://pubmed.ncbi.nlm.nih.gov/15007110
67. Nissen SE, Tuzcu EM, Schoenhagen P et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004; 291: 1071-80. https://pubmed.ncbi.nlm.nih.gov/14996776
68. LaRosa JC, Grundy SM, Waters DD et al for the Treating to New Targets (TNT) investigators. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005; 352:1425-35. https://pubmed.ncbi.nlm.nih.gov/15755765
69. Waters DD, Guyton JR, Herrington DM et al for the TNT steering committee members and investigators. Treating to New Targets (TNT) study: does lowering low-density lipoprotein cholesterol levels below currently recommended guidelines yield incremental clinical benefit? Am J Cardiol. 2004; 93:154-8.
70. Pitt B. Low-density lipoprotein cholesterol in patients with stable coronary heart disease—is it time to shift our goals? N Engl J Med. 2005; 352:1483-4.
71. Deedwania P, Barter P, Carmena R et al for the Treating to New Targets Investigators. Reduction of low-density lipoprotein cholesterol in patients with coronary heart disease and metabolic syndrome: analysis of the Treating to New Targets study. Lancet. 2006; 368:919–28. https://pubmed.ncbi.nlm.nih.gov/16962881
73. The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transiet ischemic attack. N Engl J Med. 2006; 355:549-59. https://pubmed.ncbi.nlm.nih.gov/16899775
74. Kent DM. Stroke—An equal opportunity for the initiation of statin therapy. N Engl J Med. 2006; 355:613-5. https://pubmed.ncbi.nlm.nih.gov/16899782
79. CMP Pharma. Atorvaliq(atorvastatin calcium) oral suspension prescribing information. Farmville, NC; 2023 Feb.
81. Pedersen TR, Faergeman O, Kastelein JJ, Olsson AG, Tikkanen MJ, Holme I, Larsen ML, Bendiksen FS, Lindahl C, Szarek M, Tsai J; Incremental Decrease in End Points Through Aggressive Lipid Lowering (IDEAL) Study Group. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005 Nov 16;294(19):2437-45. doi: 10.1001/jama.294.19.2437. Erratum in: JAMA. 2005 Dec 28;294(24):3092. PMID: 16287954.
82. van Dam M, Zwart M, de Beer F, Smelt AH, Prins MH, Trip MD, Havekes LM, Lansberg PJ, Kastelein JJ. Long term efficacy and safety of atorvastatin in the treatment of severe type III and combined dyslipidaemia. Heart. 2002 Sep;88(3):234-8. doi: 10.1136/heart.88.3.234. PMID: 12181212; PMCID: PMC1767327.
200. Food and Drug Administration. FDA drug safety communication: Important safety label changes to cholesterol-lowering statin drugs. Rockville, MD; 2012 Feb 28. From FDA website. http://www.fda.gov/Drugs/DrugSafety/ucm293101.htm
201. Food and Drug Administration. FDA expands advice on statin risks. Rockville, MD; 2012 Feb 27. From FDA website. http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm293330.htm
202. McKenney JM, Davidson MH, Jacobson TA et al. Final conclusions and recommendations of the National Lipid Association Statin Safety Assessment Task Force. Am J Cardiol. 2006; 97(suppl):89-94C.
309. Cannon CP, Blazing MA, Giugliano RP et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med. 2015; 372:2387-97. https://pubmed.ncbi.nlm.nih.gov/26039521
336. Cholesterol Treatment Trialists' (CTT) Collaborators, Mihaylova B, Emberson J et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012; 380:581-90. https://pubmed.ncbi.nlm.nih.gov/22607822
337. Baigent C, Keech A, Kearney PM et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005; 366:1267-78. https://pubmed.ncbi.nlm.nih.gov/16214597
338. Cholesterol Treatment Trialists’ (CTT) Collaboration, Baigent C, Blackwell L et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010; 376:1670-81. https://pubmed.ncbi.nlm.nih.gov/21067804
339. Wiggins BS, Saseen JJ, Page RL et al. Recommendations for Management of Clinically Significant Drug-Drug Interactions With Statins and Select Agents Used in Patients With Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2016; 134:e468-e495.
350. Stone NJ, Robinson J, Lichtenstein AH et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; :. http://circ.ahajournals.org/content/early/2013/11/11/01.cir.0000437738.63853.7a
351. Stone NJ, Robinson JG, Lichtenstein AH et al. Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Disease Risk in Adults: Synopsis of the 2013 ACC/AHA Cholesterol Guideline. Ann Intern Med. 2014; :. https://pubmed.ncbi.nlm.nih.gov/24474185
352. Eckel RH, Jakicic JM, Ard JD et al. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2960-84. https://pubmed.ncbi.nlm.nih.gov/24239922
353. ACCORD Study Group, Ginsberg HN, Elam MB et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010; 362:1563-74. https://pubmed.ncbi.nlm.nih.gov/20228404
354. AIM-HIGH Investigators, Boden WE, Probstfield JL et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011; 365:2255-67. https://pubmed.ncbi.nlm.nih.gov/22085343
356. Miller M, Stone NJ, Ballantyne C et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011; 123:2292-333. https://pubmed.ncbi.nlm.nih.gov/21502576
357. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011; 128 Suppl 5:S213-56. https://pubmed.ncbi.nlm.nih.gov/22084329
369. HPS2-THRIVE Collaborative Group, Landray MJ, Haynes R et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014; 371:203-12. https://pubmed.ncbi.nlm.nih.gov/25014686
371. Anderson TJ, Boden WE, Desvigne-Nickens P et al. Safety profile of extended-release niacin in the AIM-HIGH trial. N Engl J Med. 2014; 371:288-90. https://pubmed.ncbi.nlm.nih.gov/25014706
373. GlaxoSmithKline. Lovaza (omega-3-acid ethyl esters) capsules prescribing information. Research Triangle Park, NC; 2014 May.
374. Amryt Pharmaceuticals. Juxtapid (lomitapide mesylate) capsules prescribing information. Dublin, Ireland; 2020 Sep.
387. Wanner C, Krane V, März W et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005; 353:238-48. https://pubmed.ncbi.nlm.nih.gov/16034009
400. Grundy SM, Stone NJ, Bailey AL et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019; 139:e1082-e1143. https://pubmed.ncbi.nlm.nih.gov/30586774
401. American Diabetes Association Professional Practice Committee. 10. Cardiovascular Disease and Risk Management: Standards of Care in Diabetes-2024. Diabetes Care. 2024 Jan 1;47(Suppl 1):S179-S218. doi: 10.2337/dc24-S010. PMID: 38078592; PMCID: PMC10725811.
402. Virani SS, Newby LK, Arnold SV, Bittner V, Brewer LC, Demeter SH, Dixon DL, Fearon WF, Hess B, Johnson HM, Kazi DS, Kolte D, Kumbhani DJ, LoFaso J, Mahtta D, Mark DB, Minissian M, Navar AM, Patel AR, Piano MR, Rodriguez F, Talbot AW, Taqueti VR, Thomas RJ, van Diepen S, Wiggins B, Williams MS. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2023 Aug 29;148(9):e9-e119. Doi: 10.1161/CIR.0000000000001168. Epub 2023 Jul 20. Erratum in: Circulation. 2023 Sep 26;148(13):e148. Erratum in: Circulation. 2023 Dec 5;148(23):e186. PMID: 37471501.
403. Writing Committee; Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Covington AM, DePalma SM, Minissian MB, Orringer CE, Smith SC Jr, Waring AA, Wilkins JT. 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Oct 4;80(14):1366-1418. doi: 10.1016/j.jacc.2022.07.006. Epub 2022 Aug 25. Erratum in: J Am Coll Cardiol. 2023 Jan 3;81(1):104. PMID: 36031461.
404. Wiegman A, Gidding SS, Watts GF, Chapman MJ, Ginsberg HN, Cuchel M, Ose L, Averna M, Boileau C, Borén J, Bruckert E, Catapano AL, Defesche JC, Descamps OS, Hegele RA, Hovingh GK, Humphries SE, Kovanen PT, Kuivenhoven JA, Masana L, Nordestgaard BG, Pajukanta P, Parhofer KG, Raal FJ, Ray KK, Santos RD, Stalenhoef AF, Steinhagen-Thiessen E, Stroes ES, Taskinen MR, Tybjærg-Hansen A, Wiklund O; European Atherosclerosis Society Consensus Panel. Familial hypercholesterolaemia in children and adolescents: gaining decades of life by optimizing detection and treatment. Eur Heart J. 2015 Sep 21;36(36):2425-37. doi: 10.1093/eurheartj/ehv157. Epub 2015 May 25. PMID: 26009596; PMCID: PMC4576143.
405. US Food and Drug Administration. FDA Drug Safety Communication: FDA requests removal of strongest warning against using cholesterol-lowering statins during pregnancy; still advises most pregnant patients should stop taking statins. Silver Spring, MD; 2021 July 20. From FDA website. Accessed 2021 Sept 9. https://www.fda.gov/safety/medical-product-safety-information/statins-drug-safety-communication-fda-requests-removal-strongest-warning-against-using-cholesterol
406. Cheeley MK, Saseen JJ, Agarwala A et al. NLA scientific statement on statin intolerance: a new definition and key considerations for ASCVD risk reduction in the statin intolerant patient. J Clin Lipidol. 2022; 16:361-375.
407. Bouhairie VE, Goldberg AC. Familial hypercholesterolemia. Cardiol Clin. 2015;33(2):169-179.
408. Bajaj A, Cuchel M. Advancements in the treatment of homozygous familial hypercholesterolemia. J Atheroscler Thromb. 2022;29(8):1125-1135.
409. Watts GF, Gidding SS, Hegele RA, etc. International Atherosclerosis Society guidance for implementing best practice in the care of familial hypercholesterolemia. Nat Rev Cardiol. 2023; Jun 15. [online ahead of print].
500. Cooper-DeHoff RM, Niemi M, Ramsey LB, et al. The Clinical Pharmacogenetics Implementation Consortium Guideline for SLCO1B1, ABCG2, and CYP2C9 genotypes and Statin-Associated Musculoskeletal Symptoms. Clin Pharmacol Ther. 2022 May;111(5):1007-1021. doi: 10.1002/cpt.2557. Epub 2022 Mar 11. PMID: 35152405; PMCID: PMC9035072.
501. Sadowska A, Osiński P, Roztocka A, Kaczmarz-Chojnacka K, Zapora E, Sawicka D, Car H. Statins-From Fungi to Pharmacy. Int J Mol Sci. 2023 Dec 29;25(1):466. doi: 10.3390/ijms25010466. PMID: 38203637; PMCID: PMC10779115.
502. Balasubramanian R, Maideen NMP. HMG-CoA Reductase Inhibitors (Statins) and their Drug Interactions Involving CYP Enzymes, P-glycoprotein and OATP Transporters-An Overview. Curr Drug Metab. 2021;22(5):328-341. doi: 10.2174/r2029200222666210114122729. PMID: 33459228.
503. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services. (February 27, 2024). Accessed 2024 Apr 18. Available at https://clinicalinfo.hiv.gov/en/guidelines [Web]
504. Gagné C, Gaudet D, Bruckert E; Ezetimibe Study Group. Efficacy and safety of ezetimibe coadministered with atorvastatin or simvastatin in patients with homozygous familial hypercholesterolemia. Circulation. 2002 May 28;105(21):2469-75. doi: 10.1161/01.cir.0000018744.58460.62. PMID: 12034651.
505. Ho CK, Walker SW. Statins and their interactions with other lipid-modifying medications: safety issues in the elderly. Ther Adv Drug Saf. 2012 Feb;3(1):35-46. doi: 10.1177/2042098611428486. PMID: 25083224; PMCID: PMC4110829.
Related/similar drugs
Frequently asked questions
- Can you use limes or lime juice while taking statin drugs (i.e. atorvastatin)?
- Do I need to eat food when taking atorvastatin?
- What are the side effects of statins?
- How long does atorvastatin stay in the system after stopping the drug?
- Do statins help treat COVID-19?
- Can I trust a generic drug manufacturer?
More about atorvastatin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (303)
- Drug images
- Latest FDA alerts (6)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: statins
- Breastfeeding
- En español