Adalimumab Dosage
Medically reviewed by Drugs.com. Last updated on May 6, 2025.
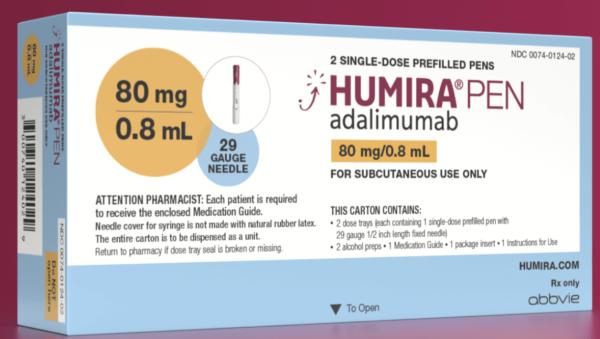
Applies to the following strengths: afzb 40 mg/0.8 mL; afzb 20 mg/0.4 mL; 80 mg/0.8 mL-40 mg/0.4 mL; 80 mg/0.8 mL; 40 mg/0.4 mL; 20 mg/0.2 mL; 10 mg/0.1 mL; 40 mg/0.8 mL; 10 mg/0.2 mL; 20 mg/0.4 mL; adbm 40 mg/0.8 mL; adbm 10 mg/0.2 mL; adbm 20 mg/0.4 mL; adbm 40 mg/0.4 mL; fkjp 40 mg/0.8 mL; fkjp 20 mg/0.4 mL; ryvk 80 mg/0.8 mL; ryvk 20 mg/0.2 mL; ryvk 40 mg/0.4 mL; atto 20 mg/0.2 mL; atto 40 mg/0.8 mL; atto 20 mg/0.4 mL; atto 10 mg/0.2 mL; atto 40 mg/0.4 mL; atto 80 mg/0.8 mL; adaz 80 mg/0.8mL; adaz 40 mg/0.4mL; adaz 20 mg/0.2mL; adaz 10 mg/0.1mL; adaz 80 mg/0.8mL-40 mg/0.4mL; aacf 40 mg/0.8 mL; aqvh 40 mg/0.8 ml; aaty 40 mg/0.4 mL; aaty 80 mg/0.8 mL; aaty 20 mg/0.2 mL; bwwd 40 mg/0.8 mL; bwwd 40 mg/0.4 mL; adaz 40 mg/0.8 mL
Usual Adult Dose for:
- Rheumatoid Arthritis
- Ankylosing Spondylitis
- Psoriatic Arthritis
- Crohn's Disease - Acute
- Crohn's Disease - Maintenance
- Ulcerative Colitis
- Plaque Psoriasis
- Uveitis
- Hidradenitis Suppurativa
Usual Pediatric Dose for:
- Juvenile Idiopathic Arthritis
- Crohn's Disease - Acute
- Crohn's Disease - Maintenance
- Uveitis
- Hidradenitis Suppurativa
Additional dosage information:
Usual Adult Dose for Rheumatoid Arthritis
40 mg subcutaneously every other week; some patients with RA not taking concomitant methotrexate may benefit from increasing the frequency to 40 mg every week
Comments:
- Methotrexate, glucocorticoids, salicylates, nonsteroidal anti-inflammatory drugs, analgesics, or other disease modifying agents may be given concomitantly.
Use: Rheumatoid Arthritis (RA): To reduce symptoms, induce major clinical response, inhibit the progression of structural damage, and improve physical function in adult patients with moderately to severely active RA alone or in combination with methotrexate or other nonbiologic disease-modifying anti-rheumatic drugs (DMARDs)
Usual Adult Dose for Ankylosing Spondylitis
40 mg subcutaneously every other week
Comments:
- Methotrexate, glucocorticoids, salicylates, nonsteroidal anti-inflammatory drugs, analgesics, or other disease modifying agents may be given concomitantly.
Uses:
- Psoriatic Arthritis (PsA): To reduce symptoms, inhibit the progression of structural damage, and improve physical function in adult patients with active PsA alone or in combination with nonbiologic DMARDs
- Ankylosing Spondylitis (AS): To reduce symptoms in adult patients with active AS
Usual Adult Dose for Psoriatic Arthritis
40 mg subcutaneously every other week
Comments:
- Methotrexate, glucocorticoids, salicylates, nonsteroidal anti-inflammatory drugs, analgesics, or other disease modifying agents may be given concomitantly.
Uses:
- Psoriatic Arthritis (PsA): To reduce symptoms, inhibit the progression of structural damage, and improve physical function in adult patients with active PsA alone or in combination with nonbiologic DMARDs
- Ankylosing Spondylitis (AS): To reduce symptoms in adult patients with active AS
Usual Adult Dose for Crohn's Disease - Acute
- Initial dose: 160 mg subcutaneously on Day 1 (given in 1 day or split over 2 consecutive days), followed by 80 mg subcutaneously 2 weeks later (Day 15)
- Maintenance dose: Starting 2 weeks later (Day 29): 40 mg subcutaneously every other week
Comments:
- Aminosalicylates and/or corticosteroids may be continued during therapy.
- Azathioprine, 6-mercaptopurine (6-MP), or methotrexate (MTX) may be continued during therapy if necessary.
- Therapy beyond one year in CD has not been established.
- Therapy in UC should only be continued in patients who have shown evidence of clinical remission by 8 weeks (Day 57).
Uses:
- Adult Crohn's Disease (CD): To reduce symptoms and induce and maintain remission in adult patients with moderately to severely active CD who have had an inadequate response to conventional therapy; to reduce symptoms and induce remission in these patients if they have also lost response to or are intolerant to infliximab
- Ulcerative Colitis (UC): To induce and sustain remission in adult patients with moderately to severely active UC who have had an inadequate response to immunosuppressants such as corticosteroids, azathioprine or 6-mercaptopurine (6-MP); effectiveness of this drug has not been established in patients who have lost response to or were intolerant to TNF blockers
Usual Adult Dose for Crohn's Disease - Maintenance
- Initial dose: 160 mg subcutaneously on Day 1 (given in 1 day or split over 2 consecutive days), followed by 80 mg subcutaneously 2 weeks later (Day 15)
- Maintenance dose: Starting 2 weeks later (Day 29): 40 mg subcutaneously every other week
Comments:
- Aminosalicylates and/or corticosteroids may be continued during therapy.
- Azathioprine, 6-mercaptopurine (6-MP), or methotrexate (MTX) may be continued during therapy if necessary.
- Therapy beyond one year in CD has not been established.
- Therapy in UC should only be continued in patients who have shown evidence of clinical remission by 8 weeks (Day 57).
Uses:
- Adult Crohn's Disease (CD): To reduce symptoms and induce and maintain remission in adult patients with moderately to severely active CD who have had an inadequate response to conventional therapy; to reduce symptoms and induce remission in these patients if they have also lost response to or are intolerant to infliximab
- Ulcerative Colitis (UC): To induce and sustain remission in adult patients with moderately to severely active UC who have had an inadequate response to immunosuppressants such as corticosteroids, azathioprine or 6-mercaptopurine (6-MP); effectiveness of this drug has not been established in patients who have lost response to or were intolerant to TNF blockers
Usual Adult Dose for Ulcerative Colitis
- Initial dose: 160 mg subcutaneously on Day 1 (given in 1 day or split over 2 consecutive days), followed by 80 mg subcutaneously 2 weeks later (Day 15)
- Maintenance dose: Starting 2 weeks later (Day 29): 40 mg subcutaneously every other week
Comments:
- Aminosalicylates and/or corticosteroids may be continued during therapy.
- Azathioprine, 6-mercaptopurine (6-MP), or methotrexate (MTX) may be continued during therapy if necessary.
- Therapy beyond one year in CD has not been established.
- Therapy in UC should only be continued in patients who have shown evidence of clinical remission by 8 weeks (Day 57).
Uses:
- Adult Crohn's Disease (CD): To reduce symptoms and induce and maintain remission in adult patients with moderately to severely active CD who have had an inadequate response to conventional therapy; to reduce symptoms and induce remission in these patients if they have also lost response to or are intolerant to infliximab
- Ulcerative Colitis (UC): To induce and sustain remission in adult patients with moderately to severely active UC who have had an inadequate response to immunosuppressants such as corticosteroids, azathioprine or 6-mercaptopurine (6-MP); effectiveness of this drug has not been established in patients who have lost response to or were intolerant to TNF blockers
Usual Adult Dose for Plaque Psoriasis
80 mg subcutaneously once, followed by 40 mg subcutaneously every other week, starting one week after the initial dose
Comments:
- This drug should only be administered to patients with plaque psoriasis who will be closely monitored and have regular follow-up visits with a physician.
- Therapy beyond one year for moderate to severe Ps has not been studied.
Use: Plaque Psoriasis (Ps): For adult patients with moderate to severe chronic Ps who are candidates for systemic therapy or phototherapy, and when other systemic therapies are medically less appropriate
Usual Adult Dose for Uveitis
80 mg subcutaneously once, followed by 40 mg subcutaneously every other week, starting one week after the initial dose
Use: Uveitis (UV): For noninfectious intermediate, posterior, and panuveitis
Usual Adult Dose for Hidradenitis Suppurativa
- Initial dose: 160 mg subcutaneously on Day 1 (given in 1 day or split over 2 consecutive days) followed by 80 mg subcutaneously 2 weeks later (Day 15)
- Maintenance dose (starting Day 29 and subsequent doses): 40 mg subcutaneously every week
Comments:
- Antibiotics may be continued during therapy if necessary.
- The patient should use a topical antiseptic wash on their HS lesions daily during therapy.
Use: For the treatment of moderate to severe hidradenitis suppurativa (HS)
Usual Pediatric Dose for Juvenile Idiopathic Arthritis
2 years and older:
10 kg to less than 15 kg: 10 mg subcutaneously every other week
15 kg to less than 30 kg: 20 mg subcutaneously every other week
30 kg or greater: 40 mg subcutaneously every other week
Comments:
- Safety and efficacy have not been established patients with polyarticular JIA less than 2 years or with weight less than 10 kg.
- Methotrexate, glucocorticoids, NSAIDs and/or analgesics may be continued during therapy.
Use: Juvenile Idiopathic Arthritis (JIA): To reduce symptoms of moderately to severely active polyarticular JIA in patients 2 years older; this drug can be used alone or in combination with methotrexate
Usual Pediatric Dose for Crohn's Disease - Acute
6 years and older:
17 kg to less than 40 kg: 80 mg subcutaneously on Day 1, followed by 40 mg subcutaneously 2 weeks later (Day 15), then 20 mg subcutaneously every other week
40 kg or greater: 160 mg subcutaneously on Day 1, followed by 80 mg subcutaneously 2 weeks later (Day 15), then 40 mg subcutaneously every other week
Comments:
- Safety and efficacy have not been established pediatric patients with CD less than 6 years or less than 17 kg.
Use: Pediatric Crohn's Disease (CD): To reduce symptoms and induce and maintain remission in patients 6 years and older with moderately to severely active CD who have had an inadequate response to corticosteroids or immunomodulators such as azathioprine, 6-mercaptopurine, or methotrexate
Usual Pediatric Dose for Crohn's Disease - Maintenance
6 years and older:
17 kg to less than 40 kg: 80 mg subcutaneously on Day 1, followed by 40 mg subcutaneously 2 weeks later (Day 15), then 20 mg subcutaneously every other week
40 kg or greater: 160 mg subcutaneously on Day 1, followed by 80 mg subcutaneously 2 weeks later (Day 15), then 40 mg subcutaneously every other week
Comments:
- Safety and efficacy have not been established pediatric patients with CD less than 6 years or less than 17 kg.
Use: Pediatric Crohn's Disease (CD): To reduce symptoms and induce and maintain remission in patients 6 years and older with moderately to severely active CD who have had an inadequate response to corticosteroids or immunomodulators such as azathioprine, 6-mercaptopurine, or methotrexate
Usual Pediatric Dose for Uveitis
2 years and older:
10 kg to less than 15 kg: 10 mg subcutaneously every other week
15 kg to less than 30 kg: 20 mg subcutaneously every other week
30 kg or greater: 40 mg subcutaneously every other week
Comments:
- Safety and efficacy has not been established patients with polyarticular JIA less than 2 years or with a weight less than 10 kg.
- Methotrexate, glucocorticoids, NSAIDs and/or analgesics may be continued during therapy.
Use: Uveitis (UV): For non-infectious intermediate, posterior, and panuveitis in pediatric patients 2 years of age and older
Usual Pediatric Dose for Hidradenitis Suppurativa
12 years and older:
30 kg to less than 60 kg: 80 mg subcutaneously initially on Day 1, then 40 mg subcutaneously on Day 8, then 40 mg subcutaneously every other week
60 kg or greater: 160 mg subcutaneously initially on Day 1 (given in 1 day or split over 2 consecutive days), then 80 mg subcutaneously on Day 15, then 40 mg subcutaneously on Day 29, then 40 mg subcutaneously every week
Comments:
- Antibiotics may be continued during therapy if necessary.
- The patient should use a topical antiseptic wash on their HS lesions daily during therapy.
Use: For the treatment of moderate to severe hidradenitis suppurativa (HS) in patients 12 years of age and older
Renal Dose Adjustments
Data not available
Liver Dose Adjustments
Data not available
Precautions
US BOXED WARNINGS:
- SERIOUS INFECTIONS: There is an increased risk of serious infections leading to hospitalization or death, including tuberculosis (TB), bacterial sepsis, invasive fungal infections (such as histoplasmosis), and infections due to other opportunistic pathogens. This drug should be discontinued if a patient develops a serious infection or sepsis during therapy. A test should be performed for latent TB; if positive, treatment for TB should be started prior to starting therapy. All patients should be monitored for active TB during therapy, even if the initial latent TB test is negative.
- MALIGNANCY: Lymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with TNF blockers. Hepatosplenic T-cell lymphoma (HSTCL) has been reported. Most cases have occurred in patients with Crohn's disease or ulcerative colitis and the most were in adolescent and young adult males. Almost all these patients had received therapy with azathioprine or 6-mercaptopurine (6-MP) concomitantly with a TNF blocker at or prior to diagnosis. It is uncertain whether the occurrence of HSTCL is related to use of a TNF blocker or a TNF blocker in combination with these other immunosuppressants.
CONTRAINDICATIONS:
- None
Rheumatoid Arthritis (RA)/Psoriatic Arthritis (PsA)/Ankylosing Spondylitis (AS)/Ulcerative Colitis (UC)/Plaque Psoriasis (Ps): Safety and effectiveness have not been established in patients younger than 18 years.
- Pediatric Polyarticular JIA: Safety and effectiveness have not been established in patients younger than 2 years.
- Pediatric Crohn's Disease: Safety and effectiveness have not been established in patients younger than 6 years.
- Hidradenitis Suppurativa (HS): Safety and effectiveness have not been established in patients younger than 12 years.
- Uveitis (UV): Safety and effectiveness have not been established in patients younger than 2 years.
Consult WARNINGS section of additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Following training in subcutaneous injection technique, patients may self-inject this drug.
- Self-injection sites include the thigh or abdomen.
- Injection sites should be rotated and this drug should not be injected into areas where the skin is tender, bruised, red, or hard.
Storage requirements:
- Refrigerate at 2C to 8C; do not freeze.
- If necessary, single prefilled syringes or pens may be stored at room temperature (below 25C) and protected from light for up to 14 days. Once removed from the refrigerator for storage at room temperature, the syringe should be used within 14 days or discarded, regardless of whether it is returned to the refrigerator or not.
General:
- There is an increased risk of lymphoma in rheumatoid arthritis patients with long standing, highly active, inflammatory disease.
- Use of live vaccines should be avoided during therapy.
Monitoring:
- Cardiovascular: Signs and symptoms of new or worsening congestive heart failure
- Hematologic: Blood dyscrasias
- Immunologic: Infections and development of autoantibodies
- Neurologic: New onset or exacerbation of clinical symptoms and/or radiographic evidence of central nervous system demyelinating disease
- Oncologic: Lymphomas or other malignancies, particularly in rheumatoid arthritis patients, patients with a history of malignancy, COPD patients, and patients with a history of heavy smoking
- Patients with a medical history of extensive immunosuppressant therapy and psoriasis patients with a history of PUVA treatment should be examined for the presence of non-melanoma skin cancer prior to and during therapy.
Patient advice:
- Patients using a prefilled pen or syringe should be instructed to inject the full amount in the device.
- If removing the syringe from the refrigerator for room temperature storage, record the date of removal to allow the syringe to be discarded after the maximum of 14 days if not used.
Frequently asked questions
- What medications are known to cause hair loss?
- What are the new drugs for rheumatoid arthritis (RA)?
- Can you take Humira with antibiotics?
- Cosentyx vs Humira: How do they compare?
- Skyrizi vs Humira for plaque psoriasis - How do they compare?
- Is Amjevita interchangeable with Humira?
- What is the difference between Cyltezo and Humira?
- What are the new drugs for plaque psoriasis?
- What are biologic drugs and how do they work?
More about adalimumab
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (748)
- Side effects
- Patient tips
- During pregnancy
- Support group
- Drug class: antirheumatics
- Breastfeeding
Patient resources
- Adalimumab drug information
- Adalimumab-aacf (Advanced Reading)
- Adalimumab-aaty (Advanced Reading)
- Adalimumab-adaz (Advanced Reading)
- Adalimumab-adbm (Advanced Reading)
Other brands
Humira, Hyrimoz, Hadlima, Amjevita, ... +7 more
Professional resources
- Adalimumab monograph
- Adalimumab Injection (FDA)
- Adalimumab-aacf (FDA)
- Adalimumab-adaz (FDA)
- Adalimumab-adbm (FDA)
Other brands
Humira, Hyrimoz, Hadlima, Amjevita, ... +7 more
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.