Ketek Disease Interactions
There are 7 disease interactions with Ketek (telithromycin).
- Colitis
- Hepatitis
- Liver disease
- Myasthenia gravis
- QT interval prolongation
- Hemodialysis
- Renal dysfunction
Antibiotics (applies to Ketek) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
Telithromycin (applies to Ketek) hepatitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Autoimmune Hepatitis
The use of telithromycin is contraindicated in patients with previous history of hepatitis and/or jaundice associated with the use of any macrolide antibacterial agent.
Telithromycin (applies to Ketek) liver disease
Major Potential Hazard, Moderate plausibility. Applicable conditions: Alcoholism
Hepatic dysfunction, including elevated liver enzymes and hepatitis, with or without jaundice, has been reported with the use of telithromycin. Although these events are generally reversible, liver failure resulting in transplantation or death has been reported rarely during postmarketing use. Alcohol use may have been a contributing factor in some of the severe cases. Therapy with telithromycin should preferably be avoided in patients with alcoholism, liver disease, or a prior history of hepatitis/jaundice associated with use of the drug. Patients treated with telithromycin should be instructed to discontinue the drug and seek medical attention promptly if signs and symptoms of hepatic injury develop such as fever, pruritus, rash, anorexia, nausea, vomiting, fatigue, right upper quadrant pain, dark urine, and jaundice.
The pharmacokinetics of telithromycin is not significantly altered in the presence of hepatic impairment due to a compensatory increase in renal elimination. No dosage adjustment is necessary unless renal function is also severely impaired (CrCl < 30 mL/min).
Telithromycin (applies to Ketek) myasthenia gravis
Major Potential Hazard, High plausibility.
Telithromycin is contraindicated in patients with myasthenia gravis. There have been reports of fatal and life-threatening respiratory failure in patients with myasthenia gravis associated with the use of this drug.
Telithromycin (applies to Ketek) QT interval prolongation
Major Potential Hazard, Moderate plausibility. Applicable conditions: Abnormal Electrocardiogram, Arrhythmias, Electrolyte Abnormalities, Hypokalemia, Magnesium Imbalance
Telithromycin may prolong the QTc interval of the electrocardiogram in some patients. QTC prolongation has been associated with an increased risk of ventricular arrhythmias including ventricular tachycardia, ventricular fibrillation, and torsade de pointes. No cardiovascular morbidity or mortality attributable to QTc prolongation occurred with telithromycin treatment in nearly 5000 patients in clinical efficacy trials, including 204 patients who had a prolonged QTc interval at baseline. In addition, a pharmacokinetic study found no significant QT prolongation in 34 healthy volunteers at all heart rates tested following telithromycin administered as repeated doses of 800 mg or as single doses of up to 2400 mg. Nevertheless, therapy with telithromycin should be avoided in patients with preexisting arrhythmia or congenital prolongation of the QTc interval. It should also be avoided in the presence of proarrhythmic conditions such as uncorrected hypokalemia or hypomagnesemia; clinically significant bradycardia; or concomitant use of class IA or III antiarrhythmic drugs or other medications that are known to produce an increase in the QTc interval.
Telithromycin (applies to Ketek) hemodialysis
Moderate Potential Hazard, High plausibility.
The effect of hemodialysis on removing telithromycin from the body has not been studied. Doses should be given after the dialysis session on dialysis days.
Telithromycin (applies to Ketek) renal dysfunction
Moderate Potential Hazard, High plausibility.
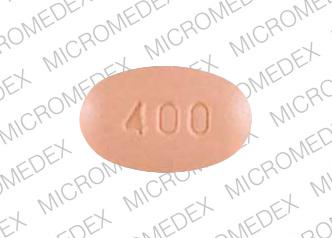
Telithromycin is eliminated by both renal and hepatic routes. In a multiple-dose study of subjects with varying degrees of renal impairment, patients classified as having severely impaired renal function (CrCl < 30 mL/min) had a 1.4-fold increase in steady-state peak plasma concentration (Cmax) and a 1.9-fold increase in systemic exposure (AUC) of telithromycin compared to healthy volunteers following administration of 800 mg once daily for 5 days. Renal excretion may serve as a compensatory elimination pathway for telithromycin in situations where metabolic clearance is impaired. In one study, coadministration of ketoconazole (which inhibits metabolism of telithromycin via CYP450 3A4) in 2 patients with severe renal impairment resulted in a 4- to 5-fold increase in telithromycin AUC compared to that in healthy subjects with normal renal function receiving telithromycin alone. Since patients with severe renal impairment are prone to conditions that may impair their metabolic clearance, telithromycin dosage should be reduced to 600 mg once daily in patients with severe renal impairment (CrCl < 30 mL/min), including those undergoing dialysis. The dosage should be further reduced to 400 mg once daily if there is coexisting hepatic impairment.
Switch to professional interaction data
Ketek drug interactions
There are 672 drug interactions with Ketek (telithromycin).
More about Ketek (telithromycin)
- Ketek consumer information
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: ketolides
- Breastfeeding
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.