Pimavanserin Disease Interactions
There are 9 disease interactions with pimavanserin.
- Dementia
- NMS
- Hepatic impairment
- QT prolongation
- Seizure
- Hematologic abnormalities
- Hyperglycemia/diabetes
- Hyperprolactinemia
- Renal impairment
Atypical antipsychotic agents (applies to pimavanserin) dementia
Major Potential Hazard, High plausibility.
Antipsychotic drugs are not approved for the treatment of patients with dementia-related psychosis. Older patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death; although the causes were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. A causal relationship with antipsychotic use has not been established. In controlled trials in older patients with dementia-related psychosis, patients randomized to risperidone, aripiprazole, and olanzapine had higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack), including fatalities, compared to patients treated with placebo.
Neuroleptics (applies to pimavanserin) NMS
Major Potential Hazard, High plausibility. Applicable conditions: Neuroleptic Malignant Syndrome
The central dopaminergic blocking effects of neuroleptic agents may precipitate or aggravate a potentially fatal symptom complex known as neuroleptic malignant syndrome (NMS). NMS is observed most frequently when high-potency agents like haloperidol are administered intramuscularly, but may occur with any neuroleptic agent given for any length of time. Clinical manifestations of NMS include hyperpyrexia, muscle rigidity, altered mental status and autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac arrhythmias). Additional signs may include elevated creatine phosphokinase, myoglobinuria, and acute renal failure. Neuroleptic agents should not be given to patients with active NMS and should be immediately discontinued if currently being administered in such patients. In patients with a history of NMS, introduction or reintroduction of neuroleptic agents should be carefully considered, since NMS may recur.
Pimavanserin (applies to pimavanserin) hepatic impairment
Major Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
The use of pimavanserin is not recommended in patients with hepatic impairment, as this drug has not been evaluated in this patient population.
Pimavanserin (applies to pimavanserin) QT prolongation
Major Potential Hazard, Moderate plausibility. Applicable conditions: Arrhythmias, Hypokalemia, Magnesium Imbalance
Pimavanserin prolongs the QT interval and should be avoided in patients with known QT prolongation or in patients taking other drugs known to prolong QT interval (class 1A and class 3 antiarrhythmics, certain antipsychotics, and some antibiotics). Pimavanserin should also be avoided in patients with cardiac arrhythmias and other circumstances that might increase the risk of the occurrence of Torsade de Pointes and/or sudden death, including symptomatic bradycardia, hypokalemia or hypomagnesemia.
Antipsychotic/neuroleptic agents (applies to pimavanserin) seizure
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Alcoholism
Antipsychotic and neuroleptic drugs can lower the seizure threshold and trigger seizures in a dose-dependent manner. This risk is greatest in patients with a history of seizures or with conditions that lower the seizure threshold. Therapy with these drugs should be administered cautiously in patients with a history of seizures or other predisposing factors, such as head trauma, CNS abnormalities, and alcoholism.
Atypical antipsychotic agents (applies to pimavanserin) hematologic abnormalities
Moderate Potential Hazard, High plausibility. Applicable conditions: Neutropenia
Cases of leukopenia, neutropenia, and agranulocytosis have been reported with the use of atypical antipsychotic agents. Patients with preexisting low white blood cell count may be at increased risk. Therapy with these agents should be administered cautiously in patients with a history of, or predisposition to, decreased white blood cell or neutrophil counts. Clinical monitoring of hematopoietic function is recommended. At the first sign of a clinically significant decline in white blood cells, discontinuation of atypical antipsychotic therapy should be considered in the absence of other causative factors, and the patient closely monitored for fever or other signs and symptoms of infection.
Atypical antipsychotic agents (applies to pimavanserin) hyperglycemia/diabetes
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Obesity
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported with the use of atypical antipsychotic agents. Patients with diabetes should be monitored for worsening control of blood glucose when treated with these agents. It is recommended that patients with risk factors for diabetes mellitus starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment, and periodically thereafter. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when treatment with these agents was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of the atypical antipsychotic drug.
Neuroleptics (applies to pimavanserin) hyperprolactinemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Breast Cancer
The chronic use of neuroleptic agents can cause persistent elevations in prolactin levels due to antagonism of dopamine D2 receptors. Based on in vitro data, approximately one-third of human breast cancers are thought to be prolactin-dependent. The clinical significance of this observation with respect to long-term neuroleptic therapy is unknown. Chronic administration of neuroleptic drugs has been associated with mammary tumorigenesis in rodent studies but not in human clinical or epidemiologic studies. Until further data are available, therapy with neuroleptic agents should be administered cautiously in patients with a previously detected breast cancer. Caution is also advised in patients with preexisting hyperprolactinemia. Hyperprolactinemia may suppress hypothalamic gonadotrophin releasing hormone (GnRH), resulting in reduced pituitary gonadotropin secretion. This, in turn, may inhibit reproductive function by impairing gonadal steroidogenesis in both female and male patients. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported in patients receiving prolactin-elevating compounds; however, the clinical significance of elevated serum prolactin levels is unknown for most patients. Long-standing hyperprolactinemia when associated with hypogonadism may lead to decreased bone density in both female and male patients.
Pimavanserin (applies to pimavanserin) renal impairment
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction
The use of pimavanserin is not recommended in patients with severe renal impairment (CrCl < 30 mL/min), as it has not been evaluated in this patient population. No dose adjustment is needed for patients with mild to moderate renal disease.
Switch to professional interaction data
Pimavanserin drug interactions
There are 358 drug interactions with pimavanserin.
Pimavanserin alcohol/food interactions
There is 1 alcohol/food interaction with pimavanserin.
More about pimavanserin
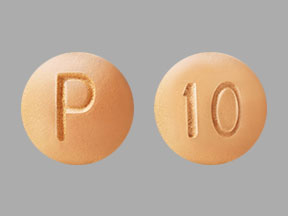
- pimavanserin consumer information
- Check interactions
- Compare alternatives
- Reviews (15)
- Side effects
- Dosage information
- During pregnancy
- Drug class: atypical antipsychotics
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.