PrandiMet Disease Interactions
There are 9 disease interactions with PrandiMet (metformin / repaglinide).
- Type I diabetes
- Lactic acidosis
- Liver disease
- Renal dysfunction
- Cardiovascular risk
- Hypoglycemia
- B12 deficiency
- Liver disease
- Renal impairment
Meglitinides (applies to PrandiMet) type I diabetes
Major Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Type 1, Diabetic Ketoacidosis
The use of meglitinides is contraindicated in patients with type I diabetes or for the treatment of diabetic ketoacidosis, with or without coma.
Metformin (applies to PrandiMet) lactic acidosis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Congestive Heart Failure, Myocardial Infarction, Shock, Anemia, Dehydration, Alcoholism, Renal Dysfunction, Diarrhea, Asphyxia, Vomiting, Diabetic Ketoacidosis
Metformin is contraindicated in patients with acute or chronic metabolic acidosis (including diabetic ketoacidosis) with or without coma. Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. Risk factors include renal dysfunction, age 65 years and older, hypoxic states, excessive alcohol intake, and liver dysfunction. Lactic acidosis has been associated with metformin accumulation in plasma at levels generally exceeding 5 mcg/mL. The risk of metformin-associated lactic acidosis increases with the patient's age because patients 65 years and older have a greater likelihood of having hepatic, renal, or cardiac impairment. Renal function should be assessed more frequently in older adult patients. Several postmarketing cases of metformin-associated lactic acidosis occurred in the setting of acute congestive heart failure, especially when accompanied by hypoperfusion and hypoxemia; cardiovascular collapse (shock), acute myocardial infarction, sepsis, and other conditions associated with hypoxemia (e.g., severe anemia, asphyxia) have been associated with lactic acidosis and may cause prerenal azotemia. When such an event occurs, metformin should be discontinued. Dehydration (e.g., severe diarrhea or vomiting) may increase the risk for volume depletion, hypotension, and renal impairment; such patients may be at increased risk for lactic acidosis. Alcohol potentiates the effect of metformin on lactate metabolism; patients should be advised against excessive alcohol intake while receiving metformin. All patients treated with metformin should have renal function monitored regularly (at least annually or more frequently if necessary). If metformin-associated lactic acidosis is suspected, general supportive measures should be instituted promptly in a hospital setting, as well as immediate discontinuation of metformin. If lactic acidosis is diagnosed or strongly suspected, prompt hemodialysis is recommended to correct the acidosis and remove accumulated metformin. Patients and their families should be educated about the symptoms of lactic acidosis and, if these symptoms occur, they should be instructed to discontinue metformin and contact their health care provider.
Metformin (applies to PrandiMet) liver disease
Major Potential Hazard, Moderate plausibility.
Metformin decreases the liver uptake of lactate increasing lactate blood levels which may increase the risk of lactic acidosis, especially in at-risk patients. There have been reports of cases of metformin-associated lactic acidosis in patients with liver dysfunction. Metformin should generally be avoided in patients with evidence of hepatic disease.
Metformin (applies to PrandiMet) renal dysfunction
Major Potential Hazard, Moderate plausibility.
The use of metformin is contraindicated in patients with severe renal dysfunction (estimated GFR [eGFR] less than 30 mL/min/1.73 m2). Metformin is substantially excreted by the kidney; the risk of metformin accumulation and lactic acidosis increases with the degree of renal dysfunction. Before starting metformin, an eGFR should be obtained. Initiation of metformin is not recommended in patients with eGFR between 30 and 45 mL/min/1.73 m2. An eGFR should be obtained at least annually in all patients; in those at risk of developing renal dysfunction (e.g., older adult patients), renal function should be assessed more frequently. In patients whose eGFR falls below 45 mL/min/1.73 m2, the benefit/risk of continuing therapy should be assessed. Postmarketing cases of metformin-associated lactic acidosis primarily occurred with significant renal dysfunction; metformin plasma levels generally exceeded 5 mcg/mL.
Oral hypoglycemic agents (applies to PrandiMet) cardiovascular risk
Major Potential Hazard, Moderate plausibility. Applicable conditions: Cardiovascular Disease
The use of oral hypoglycemic agents may be associated with an increased risk of cardiovascular mortality compared to treatment with diet alone or diet with insulin. This warning is based on the University Group Diabetes Program (UGDP) study, a long-term prospective clinical trial designed to evaluate the effectiveness of glucose-lowering drugs in preventing or delaying vascular complications in patients with non-insulin-dependent diabetes. Patients treated with diet plus a fixed dosage of either tolbutamide (a sulfonylurea) or phenformin (a biguanide) for 5 to 8 years had a cardiovascular mortality rate approximately 2.5 times that of patients treated with diet alone, resulting in discontinuation of both these treatments in the study. Despite controversy regarding interpretation of these results, clinicians and patients should be aware of the potential risk when making treatment decisions for diabetes, particularly in the presence of underlying cardiovascular disease. Data are not available for other sulfonylureas or biguanides, nor for hypoglycemic agents belonging to other classes. However, given the similarities in chemical structure and/or mode of action, the same caution should be applied.
Insulin/oral hypoglycemic agents (applies to PrandiMet) hypoglycemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Adrenal Insufficiency, Malnourished, Autonomic Neuropathy, Panhypopituitarism, Anorexia/Feeding Problems, Adrenal Insufficiency, Malnourished, Panhypopituitarism, Autonomic Neuropathy, Anorexia/Feeding Problems
Hypoglycemia may commonly occur during treatment with insulin and/or oral hypoglycemic agents. Care should be taken in patients who may be particularly susceptible to the development of hypoglycemic episodes during the use of these drugs, including those who are debilitated or malnourished, those with defective counterregulatory mechanisms (e.g., autonomic neuropathy and adrenal or pituitary insufficiency), and those receiving beta-adrenergic blocking agents.
Metformin (applies to PrandiMet) B12 deficiency
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Folic Acid/Cyanocobalamin Deficiency, Anemia Associated with Vitamin B12 Deficiency
Metformin may interfere with vitamin B12 absorption from the B12-intrinsic factor complex. A decrease to subnormal levels of previously normal serum vitamin B12 levels was reported in about 7% of patients treated with metformin during clinical trials. Such decrease may be associated with anemia but appears to be rapidly reversible with metformin discontinuation or vitamin B12 supplementation. Certain patients (those with inadequate vitamin B12 or calcium intake or absorption) appear to be predisposed to developing subnormal levels of vitamin B12; caution may be warranted when metformin is administered to these patients. It is recommended to measure vitamin B12 every 2 to 3 years and hematologic parameters annually in patients on metformin. Any abnormalities should be managed.
Repaglinide (applies to PrandiMet) liver disease
Moderate Potential Hazard, Moderate plausibility.
Repaglinide is almost completely metabolized in the liver to pharmacologically inactive substances. Patients with impaired liver function may be exposed to higher concentrations of repaglinide and its associated metabolites. Higher serum drug levels, in addition to diminished gluconeogenic capacity secondary to hepatic insufficiency, may increase the potential for severe hypoglycemic episodes. Therapy with repaglinide should be administered cautiously in patients with liver disease. Longer intervals between dosage adjustments may be required.
Repaglinide (applies to PrandiMet) renal impairment
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction, Diabetes Mellitus
Patients with severely reduced renal function treated with repaglinide had elevated plasma drug concentrations. Patients with type 2 diabetes who have severe renal function impairment should initiate repaglinide therapy with the 0.5 mg dose and subsequently, patients should be carefully titrated.
Switch to professional interaction data
PrandiMet drug interactions
There are 644 drug interactions with PrandiMet (metformin / repaglinide).
PrandiMet alcohol/food interactions
There are 2 alcohol/food interactions with PrandiMet (metformin / repaglinide).
More about PrandiMet (metformin / repaglinide)
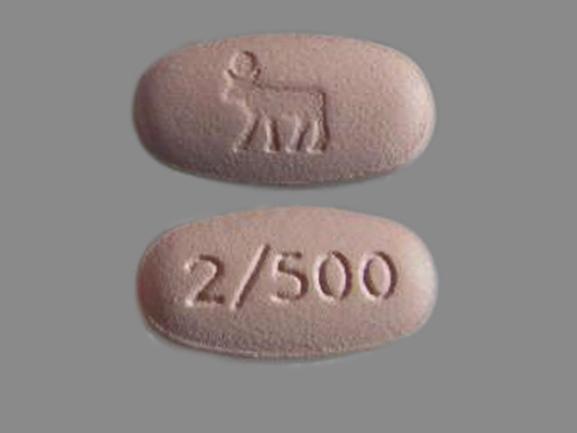
- PrandiMet consumer information
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: antidiabetic combinations
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.