Chloromycetin Disease Interactions
There are 3 disease interactions with Chloromycetin (chloramphenicol).
Antibiotics (applies to Chloromycetin) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
Chloramphenicol (applies to Chloromycetin) bone marrow suppression
Major Potential Hazard, High plausibility. Applicable conditions: Bone Marrow Depression/Low Blood Counts
Chloramphenicol may cause bone marrow depression and other hematologic toxicities, which can be irreversible or reversible. The former type is independent of dose and results in aplastic anemia with a high rate of mortality, generally from hemorrhage or infection. It has been reported following both systemic and topical administration of chloramphenicol and has an estimated incidence of 1 in 25,000 to 1 in 40,000 courses of therapy. Bone marrow aplasia or hypoplasia may occur after a single dose but more often develops weeks or months after the drug has been discontinued. A reversible myelosuppression occurs much more frequently and is characterized by anemia, vacuolation of red blood cells, decreased reticulocyte count, leukopenia, thrombocytopenia, increased serum iron concentrations, and increased serum iron-binding capacity. It is dose-dependent, occurring regularly at chloramphenicol dosages exceeding 4 g/day (in adults) or at plasma drug concentrations >= 25 mcg/mL, and usually responds to withdrawal of the drug. Therapy with chloramphenicol should be administered cautiously, if at all, in patients with preexisting blood dyscrasias and/or bone marrow depression. Complete blood counts and differential reticulocyte counts should be performed in all patients prior to initiating therapy and approximately every 2 days during therapy. Marked depression of blood counts and/or development of other hematologic abnormalities may be indication for withdrawal of chloramphenicol therapy.
Chloramphenicol (applies to Chloromycetin) renal/liver disease
Major Potential Hazard, High plausibility. Applicable conditions: Renal Dysfunction
Chloramphenicol is primarily inactivated by glucuronyl transferase in the liver and eliminated in the urine as both parent drug and metabolites. In adults with normal renal and hepatic function, only 5% to 15% of a dose of chloramphenicol is excreted unchanged by the kidney, but approximately 30% is excreted when chloramphenicol is administered intravenously as the sodium succinate ester. However, the fraction of drug excreted unchanged may be highly variable, especially in neonates and children. Therapy with chloramphenicol should be administered cautiously in patients with significantly impaired renal and/or hepatic function, since drug accumulation may occur in such patients. The dosage should be reduced based on the degree of impairment as well as plasma drug concentrations.
Switch to professional interaction data
Chloromycetin drug interactions
There are 726 drug interactions with Chloromycetin (chloramphenicol).
More about Chloromycetin (chloramphenicol)
- Check interactions
- Compare alternatives
- Reviews (1)
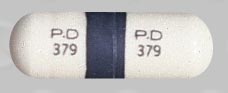
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antibiotics
- Breastfeeding
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.