Vagus Nerve Stimulation
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
AMBULATORY CARE:
What you need to know about vagus nerve stimulation (VNS):
VNS is a treatment used for epilepsy and depression. VNS is used when medicines and other treatments have not worked well. VNS may also help shorten the recovery time after you have a seizure. VNS may also help decrease symptoms of depression. It may take several months to notice changes in your seizure or depression symptoms.
How VNS works:
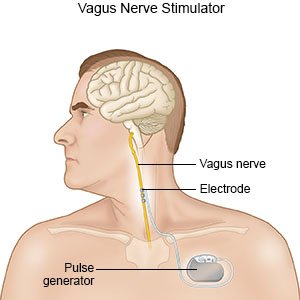
- A device called a pulse generator is used to stimulate the vagus nerve with electrical impulses. You have one vagus nerve on each side of your body. The nerve goes from your brain, through your neck, to your chest and abdomen. The vagus nerves carry messages from your brain to your organs, such as your heart and lungs. The nerves also carry messages to other parts of your brain that regulate mood, sleep, and other functions.
- The pulse generator device is about the size of a watch face. The device is placed into your chest during surgery. A wire under your skin connects the device to your left vagus nerve. You do not need the device surgically implanted if it is used for treatment of cluster headaches. The device is turned on a few weeks after surgery. This gives the surgery area time to heal. The device is powered by a battery that usually lasts about 10 years.
 |
How to prepare for VNS surgery:
Your healthcare provider will talk to you about how to prepare for surgery. He or she may tell you not to eat or drink anything after midnight on the day of your surgery. He or she will tell you what medicines to take or not take on the day of your surgery. You may be given an antibiotic through your IV to help prevent a bacterial infection. Arrange to have someone drive you home.
What will happen during VNS surgery:
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given local anesthesia to numb the surgery area. With local anesthesia, you may still feel pressure or pushing during surgery, but you should not feel any pain.
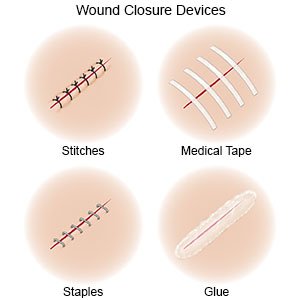
- Your surgeon will make 2 incisions. One is on your upper left chest or under your arm. The other is on the left side of your neck. He or she will place the stimulator device in your chest. Your surgeon will then guide a wire under your skin from the device to your neck. He or she will attach it to your left vagus nerve through the second incision in your neck. The incisions will be closed with medical glue, tape, or stitches.
What will happen after VNS surgery:
- The device is turned on when you see your surgeon or neurologist for a follow-up visit. This is usually a few weeks after surgery. He or she will program your device to deliver electric impulses to your vagus nerve. The impulses can be set to cycle at different levels, times, and strengths. The impulses usually start at a low level and can be increased gradually if needed.
- You may have symptoms when the impulses are happening. These may include tingling or discomfort in your neck, or a hoarse voice. You will receive a hand-held magnet. This can be used to start the impulse, such as when you sense you are going to have a seizure. The magnet can also be used to turn the device off, such as when you exercise. This is because it may be programmed to detect increased heart rate.
Related medications
Risks of VNS or surgery to place the generator:
You may bleed more than expected or develop an infection. You may have pain or discomfort where the device is placed. You may have an allergic reaction to the device or the wire. You may have pain or feel a shock during stimulation. You may have headaches, tingling on your skin, or trouble sleeping. The wire may move and you may need to have surgery again.
Call your doctor or surgeon if:
- Your surgery area has healed but you are having pain at the pulse generator site.
- You have a fever.
- Your surgery area is red, swollen, or has pus coming from it.
- Your symptoms return or get worse.
- You have new pain or new symptoms with stimulation.
- You feel like you are being shocked with the stimulator on or off.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antibiotics help prevent a bacterial infection.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care:
- Ask your surgeon about daily activities. You may need to limit activity until your surgery area heals.
- Care for your surgery area as directed. Carefully wash the area with soap and water. Gently pat the area dry.
- Keep the magnet or other programming device with you at all times.
- Tell other providers that you have an implanted VNS device. This is so other treatments or testing (such as MRI) do not interfere with the device.
Follow up with your doctor or surgeon as directed:
You will need regular visits to make sure the device is working correctly. Healthcare providers will also check the position of the device and wire. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
