Upper Endoscopy in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about an upper endoscopy?
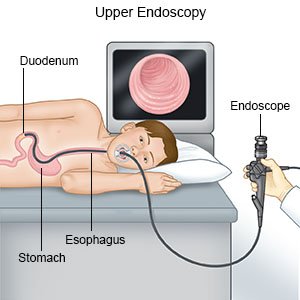
An upper endoscopy is also called an upper gastrointestinal (GI) endoscopy, or an esophagogastroduodenoscopy (EGD). The upper intestines include the esophagus, stomach, and duodenum (first part of the small intestine). A scope (thin, flexible tube with a light and camera) is used to examine the lining of your child's upper intestines. An upper endoscopy is used to look for problems, such as bleeding, swelling, polyps, ulcers, or infection. An upper endoscopy in children is often used to find the cause of abdominal pain, difficulty swallowing, or nausea and vomiting. It may also be done to remove foreign bodies such as a swallowed coin or toy.
 |
How do I prepare my child for an upper endoscopy?
- Your child's provider will tell you when your child should stop eating or drinking before the procedure. If the procedure will be later in the day, you may be able to give your child clear liquids until 2 to 4 hours before the procedure. Clear liquids include water, oral rehydration solutions (ORS), or juices without pulp. Do not give your child clear liquids that are red or purple. Stop breastfeeding your child 4 hours before the procedure.
- Your child's provider will tell you what medicines your child should take or not take on the day of the procedure. If your child is 6 years of age or older, explain what might happen during the procedure, to decrease anxiety. This may also increase his or her cooperation and tolerance for the procedure. Your child's provider may give your child medicine to help him or her relax before the procedure starts.
Related medications
What will happen during an upper endoscopy?
- Your child may receive IV sedation or general anesthesia. IV sedation will make your child feel sleepy and help him or her relax during the procedure. General anesthesia may be given to keep your child asleep and free from pain during the procedure. Your child's healthcare provider may have you come into the procedure room until your child is asleep. This may decrease your child's anxiety and help him or her cooperate with providers.
- Your child may also be given medicine to numb his or her throat. Your child may need to wear a plastic mouthpiece to help hold his or her mouth open and protect the teeth and tongue. Your child's provider will gently insert the endoscope through your child's mouth and down into the throat. Your child may feel pressure in his or her throat but should not feel pain. The endoscope will not prevent your child from breathing.
- Your child's provider will watch the scope on a monitor. He or she will take pictures with the scope and look for any abnormal areas. Your child's provider may gently inject air to see your child's digestive tract clearly. Tissue samples may be taken and sent to a lab for tests. Your child's provider may remove foreign objects, tumors, or polyps that may be blocking your child's upper intestines. He or she may also insert tools through the scope to treat bleeding or place a stent (tube). When the procedure is finished, the endoscope will be slowly removed.
What will happen after an upper endoscopy?
Your child may feel bloated, gassy, or have some abdominal discomfort or distention. Your child's throat may be sore for 24 to 36 hours after the procedure. It is normal for your child to spit up a small amount of blood. Your child may burp or pass gas from air that is still inside the body after the procedure. Your child may need to take short walks or lie on his or her left side to help move the gas out. Your child may be able to go home after he or she is awake and can drink liquids.
What are the risks of an upper endoscopy?
Your child's esophagus, stomach, or duodenum may be punctured or torn during the procedure. This is because of increased pressure as the scope and air are passing through. Your child may bleed more than expected or get an infection. Your child may have a slow or irregular heartbeat, or low blood pressure, during the procedure. This can cause sweating and fainting. Fluid may enter your child's lungs and he or she may have trouble breathing. These problems can be life-threatening.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
