Type 2 Diabetes in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
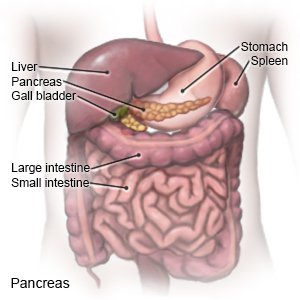
Type 2 diabetes is a disease that affects how your child's body uses glucose (sugar). When the blood sugar level increases, the pancreas should make more insulin. Insulin helps move sugar out of the blood so it can be used for energy. Type 2 diabetes develops because either the body cannot make enough insulin, or it cannot use the insulin correctly. You can help your child manage diabetes with healthy nutrition and physical activity choices.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) if:
- Your child has a seizure or cannot be woken.
- Your child's heartbeat is fast and weak.
- Your child's breath has a fruity, sweet smell.
- Your child has a low blood sugar level and it does not improve with treatment.
Call your child's doctor or diabetes care team if:
- Your child's blood sugar levels are high after several checks.
- Your child's blood sugar level does not lower with extra insulin.
- Your child often has blood sugar levels that are too low.
- Your child has abdominal pain, diarrhea, or is vomiting.
- Your child has numbness in his or her arms or legs.
- Your child has warm, red patches of skin or a wound that does not heal.
- Your child is anxious or depressed.
- You have questions or concerns about your child's condition or care.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Diabetes education:
Diabetes care team providers may come to your house and teach you and your child more about diabetes. You and your child may instead attend classes with others who have diabetes. Providers will teach the following:
- About your child's blood sugar level: You will be given information on when and how to check your child's blood sugar level. Your healthcare provider will help you and your child create a blood sugar level range. The goal is to keep your child's blood sugar within the range so it does not go too high or too low. Write down the times of your child's checks and the levels. Take them to all follow-up appointments.
- A glucose meter is a device that uses a test strip to check your child's blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your child's blood.

- A continuous glucose monitor (CGM) uses a sensor to check your child's blood sugar level. The sensor is placed on your child's abdomen or arm. A transmitter on the sensor gets a glucose reading. CGM data may be linked to an insulin pump, if needed. The data will help your child's provider see how much time your child's blood sugar level stayed in range. The provider may recommend nutrition, physical activity, or medicine changes if the levels were often above or below range.

- A glucose meter is a device that uses a test strip to check your child's blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your child's blood.
- About diabetes medicines: Non-insulin diabetes medicine may be given to help control your child's blood sugar levels. Insulin may be added if non-insulin diabetes medicine becomes less effective over time. Insulin may be given through a pump or pen, or injected. You, your child, and the diabetes care team will discuss the best method for your child:
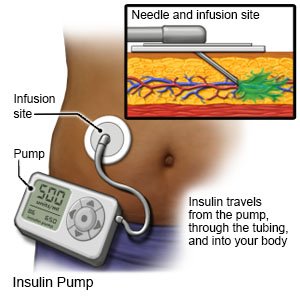
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
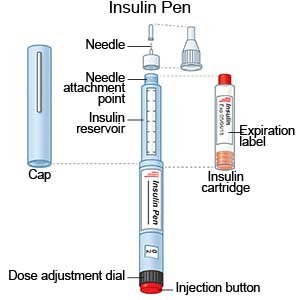
- An insulin pen is a device prefilled with insulin. Most insulin pens are disposable. You throw the pen away after it is empty or used for a certain amount of time. Some pens have a replaceable cartridge filled with insulin. You keep the pen and only throw away the cartridge.
- Insulin injections are given with a needle and syringe. Your child's provider will tell you if this is the best method for your child. You, your child, and family members will be taught how to draw up and give insulin. You will also be taught how to dispose of used needles and syringes.
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
- About nutrition: A dietitian will help you make a meal plan to keep your child's blood sugar level steady. You will learn how food affects your child's blood sugar level. You will also learn to keep track of sugar and starchy foods (carbohydrates). Do not let your child skip meals. Blood sugar levels may drop too low if your child has received insulin and does not eat.
- About physical activity and diabetes: You and your child will learn why physical activity, such as exercise, is important. A plan will be made for your child to get 60 minutes of moderate to intense aerobic activity every day. Your child can choose from activities such as brisk walking, dancing, running, or jumping rope. The plan may also include flexibility and resistance training, such as yoga and lifting weights, 3 days each week.

- About sick day management: Blood sugar levels can be too high or too low when your child is sick. Your child's care team will give you information about managing your child's diabetes during sick days.
- About complications of diabetes: Diabetes that is not controlled can lead to complications such as diabetic ketoacidosis (DKA), neuropathy, and retinopathy. You will also learn how to prevent conditions that may happen with diabetes, such as high blood pressure and high cholesterol.
Your child's nutrition:
A dietitian will help you and your child create a meal plan. The plan will help keep your child's blood sugar level steady. The following are tips to start helping with your child's nutrition:
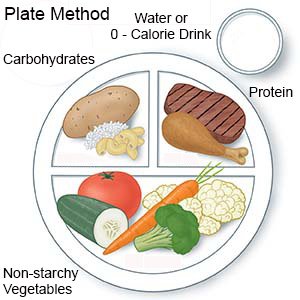
- Keep track of carbohydrates (sugar and starchy foods). Your child's blood sugar level can get too high if he or she eats too many carbohydrates. His or her dietitian will help you plan meals and snacks that have the right amount of carbohydrates. You may be taught the plate method. With the plate method, ½ of the plate contains non-starchy vegetables. The other half is divided so ¼ contains protein, and ¼ contains carbohydrates.
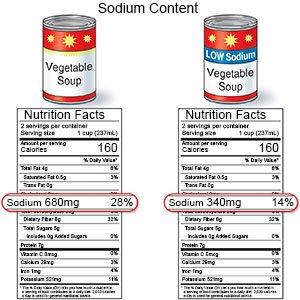
- Give your child low-fat and low-sodium foods. Examples of low-fat foods are lean meat, fish, skinless chicken or turkey, and low-fat milk. Limit high-sodium foods, such as potato chips and soup. Do not add salt to food you cook. Limit your child's use of table salt.
- Give your child high-fiber foods. Fiber helps improve blood sugar levels. Fiber also lowers your child's risk for heart disease and other problems diabetes can cause. Examples of high-fiber foods include vegetables, whole-grain bread, and beans such as pinto beans. A dietitian can tell you how much fiber to give your child each day.

Help your child manage type 2 diabetes:
- Talk to your child's care team if you or your child become stressed about diabetes care. Learning about diabetes care can be stressful. The stress can cause your child not to want to help in his or her own care. The stress can also cause you to feel overwhelmed. Your child's care team can help by offering tips. The care team may suggest you and your child talk to a mental health provider. The provider can listen and offer help with issues and feelings of being overwhelmed. You and your child may choose to see the provider at separate times. You and your child may, instead, choose to see the provider together.
- Make sure your child always wears medical alert jewelry or carries a card that says he or she has diabetes. Ask your child's care team provider where to get these items.

- Give instructions to your child's school and care providers. Make sure your child's teachers and care providers know he or she has diabetes. Provide written instructions about what to do if your child has symptoms of high or low blood sugar levels.
- Help your child maintain a healthy weight. Ask your child's team what a healthy weight is for your child. A healthy weight can help control diabetes and prevent heart disease. Ask the team to help your child create a weight-loss plan, if needed. The team will help set a weight loss goal, such as 10% of his or her extra weight. Together you and your team can set manageable weight loss goals.
- Do not smoke around your child. Do not let others smoke around him or her. Do not let your older child smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung and heart damage. Cigarette smoke can worsen the problems that occur with diabetes. Ask your care team provider for information if you or your child currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you or your child use these products.
- Bring your child in for screenings as directed. Your child will need to be screened for complications of diabetes and other conditions that may develop. Some screenings may begin right away and some may happen within the first 5 years of diagnosis. Your child will need to continue screenings through his or her lifetime. Keep your child's follow-up appointments with all providers.
- Your child will need to have his or her A1c checked. This will help make sure that your child's diabetes is well controlled. His or her care plan may need to be adjusted if the level is higher than recommended.
- Your child will have screenings for complications or other problems. Examples include kidney problems, high cholesterol, high blood pressure, blood vessel problems, eye problems, and sleep apnea. Your child may also be screened for an eating disorder or polycystic ovary syndrome (PCOS). Your child's nerves, arteries, eyes, and kidneys can be damaged.
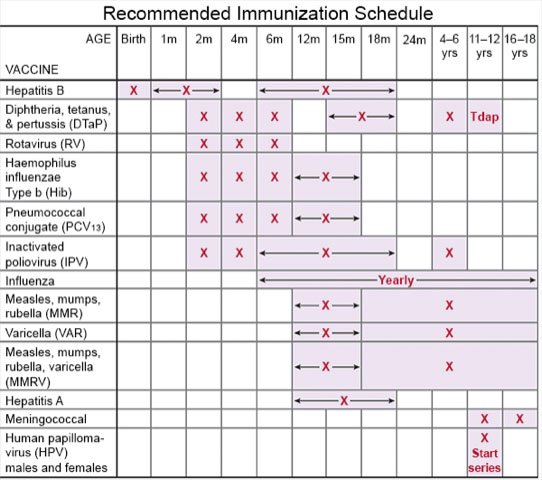
- Ask about vaccines your child may need. Your child has a higher risk for serious illness if he or she gets the flu, COVID-19, or pneumonia. Ask if your child should get vaccines to prevent these or other diseases, and when to get the vaccines.
- Talk to your child's provider about weight loss medicines, if needed. Certain medicines may be given along with other diabetes medicines to children 10 years or older who have obesity or overweight. These medicines are not used to lower blood sugar, but your child's level may decrease from weight loss.
Follow up with your child's doctor or diabetes care team as directed:
Your child will need to return to have his or her A1c checked. The care team will make sure that treatment is working. Your child's treatment may need to be adjusted. Write down questions that you and your child have so you remember to ask them during his or her visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Type 2 Diabetes
- Diabetes Medications and Alcohol Interactions
- FDA-Approved Weight Loss Drugs: Can They Help You?
- OneTouch Blood Glucose Meters
- Side Effects of Weight Loss Drugs
- Top 10 Diabetes Treatments You May Have Missed
- Which Drugs Cause Weight Gain?
Treatment options
Care guides
- Diabetes and your Skin
- Diabetic Hyperglycemia
- How to Draw Up Insulin
- Type 2 Diabetes in Adults: New Diagnosis
- Type 2 Diabetes in Children
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
