Glucophage
Generic name: metformin [ met-FOR-min ]
Other brand names of metformin include: Glucophage, Glucophage XR
Drug class: Non-sulfonylureas
The Glucophage brand name has been discontinued in the U.S. If generic versions of this product have been approved by the FDA, there may be generic equivalents available.
What is Glucophage?
Glucophage is an oral diabetes medicine that helps control blood sugar levels.
Glucophage is used together with diet and exercise to improve blood sugar control in adults with type 2 diabetes mellitus.
Glucophage is sometimes used together with insulin or other medications, but metformin is not for treating type 1 diabetes.
Warnings
You should not use Glucophage if you have severe kidney disease, metabolic acidosis, or diabetic ketoacidosis (call your doctor for treatment).
If you need to have any type of x-ray or CT scan using a dye that is injected into your veins, you may need to temporarily stop taking Glucophage.
You may develop lactic acidosis, a dangerous build-up of lactic acid in your blood. Call your doctor or get emergency medical help if you have unusual muscle pain, trouble breathing, stomach pain, dizziness, feeling cold, or feeling very weak or tired.
Before taking this medicine
You should not use Glucophage if you are allergic to metformin, or if you have:
-
severe kidney disease; or
-
metabolic acidosis or diabetic ketoacidosis (call your doctor for treatment).
If you need to have surgery or any type of x-ray or CT scan using a dye that is injected into your veins, you may need to temporarily stop taking Glucophage. Be sure your caregivers know ahead of time that you are using this medication.
Tell your doctor if you have ever had:
-
kidney disease (your kidney function may need to be checked before you take this medicine);
-
high ketone levels in your blood or urine;
-
heart disease, congestive heart failure;
-
liver disease; or
-
if you also use insulin, or other oral diabetes medications.
You may develop lactic acidosis, a dangerous build-up of lactic acid in your blood. This may be more likely if you have other medical conditions, a severe infection, chronic alcoholism, or if you are 65 or older. Ask your doctor about your risk.
Follow your doctor's instructions about using Glucophage if you are pregnant or you become pregnant. Controlling diabetes is very important during pregnancy, and having high blood sugar may cause complications in both the mother and the baby. Tell your doctor if you become pregnant while taking Glucophage.
Metformin may stimulate ovulation in a premenopausal woman and may increase the risk of unintended pregnancy. Talk to your doctor about your risk.
You should not breastfeed while using this medicine.
Glucophage should not be given to a child younger than 10 years old. Glucophage XR is not approved for use by anyone younger than 18 years old.
How should I take Glucophage?
Take Glucophage exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose. Use the medicine exactly as directed.
Take Glucophage with a meal, unless your doctor tells you otherwise. Glucophage XR is taken only once daily with the evening meal. Follow your doctor's instructions.
Do not crush, chew, or break an extended-release tablet. Swallow the tablet whole.
Glucophage XR tablet are made with a shell that is not absorbed or melted in the body. Part of this shell may appear in your stool. This is normal and will not make the medicine less effective.
You may have low blood sugar (hypoglycemia) and feel very hungry, dizzy, irritable, confused, anxious, or shaky. To quickly treat hypoglycemia, eat or drink a fast-acting source of sugar (fruit juice, hard candy, crackers, raisins, or non-diet soda).
Your doctor may prescribe a glucagon injection kit in case you have severe hypoglycemia. Be sure your family or close friends know how to give you this injection in an emergency.
Blood sugar levels can be affected by stress, illness, surgery, exercise, alcohol use, or skipping meals. Ask your doctor before changing your dose or medication schedule.
Glucophage is only part of a complete treatment program that may also include diet, exercise, weight control, regular blood sugar testing, and special medical care. Follow your doctor's instructions very closely.
Store at room temperature away from moisture, heat, and light.
Your doctor may have you take extra vitamin B12 while you are taking metformin. Take only the amount of vitamin B12 that your doctor has prescribed.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. An overdose can cause severe hypoglycemia or lactic acidosis.
What to avoid
Avoid drinking alcohol. It lowers blood sugar and may increase your risk of lactic acidosis.
Glucophage side effects
Get emergency medical help if you have signs of an allergic reaction to Glucophage: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Some people using metformin develop lactic acidosis, which can be fatal. Get emergency medical help if you have even mild symptoms such as:
-
unusual muscle pain;
-
feeling cold;
-
trouble breathing;
-
feeling dizzy, light-headed, tired, or very weak;
-
stomach pain, vomiting; or
-
slow or irregular heart rate.
Common Glucophage side effects may include:
-
low blood sugar;
-
nausea, upset stomach; or
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Rybelsus
Rybelsus tablets are used to improve blood sugar control in adults with type 2 diabetes, and may ...
Mounjaro
Mounjaro (tirzepatide) is FDA-approved to manage type 2 diabetes in adults. It lowers blood sugar ...
Trulicity
Trulicity is an injectable diabetes medicine that is used together with diet and exercise to ...
Lantus
Lantus is a long acting form of insulin used to treat type 1 or type 2 diabetes. Learn about side ...
Tresiba
Tresiba (insulin degludec) is used to treat diabetes mellitus. Includes Tresiba side effects ...
Victoza
Victoza helps control blood sugar levels and reduce the risk of serious heart problems in people ...
Basaglar
Basaglar (insulin glargine) is a long-acting insulin that is used to improve blood sugar control in ...
Levemir
Levemir (insulin detemir) is a long acting insulin used to treat diabetes in adults and children ...
Dosing information
Usual Adult Dose for Diabetes Type 2:
Immediate-release:
Initial dose: 500 mg orally twice a day or 850 mg orally once a day
Dose titration: Increase in 500 mg weekly increments or 850 mg every 2 weeks as tolerated
Maintenance dose: 2000 mg daily in divided doses
Maximum dose: 2550 mg/day
Extended-release:
Initial dose: 500 to 1000 mg orally once a day
Dose titration: Increase in 500 mg weekly increments as tolerated
Maintenance dose: 2000 mg daily
Maximum dose: 2500 mg daily
Comments:
-Metformin, if not contraindicated, is the preferred initial pharmacologic agent for treatment of type 2 diabetes mellitus.
-Immediate-release: Take in divided doses 2 to 3 times a day with meals; titrate slowly to minimize gastrointestinal side effects. In general, significant responses are not observed with doses less than 1500 mg/day.
-Extended-release: Take with the evening meal; if glycemic control is not achieved with 2000 mg once a day, may consider 1000 mg of extended-release product twice a day; if glycemic control is still not achieve, may switch to immediate-release product.
Use: To improve glycemic control in adults with type 2 diabetes mellitus as an adjunct to diet and exercise.
Usual Pediatric Dose for Diabetes Type 2:
10 years or older:
Immediate-release:
Initial dose: 500 mg orally twice a day
Dose titration: Increase in 500 mg weekly increments as tolerated
Maintenance dose: 2000 mg daily
Maximum dose: 2000 mg daily
Comments: Take in divided doses 2 to 3 times a day with meals. Titrate slowly to minimize gastrointestinal side effects.
Safety and effectiveness of Glucophage extended-release has not been established in pediatric patients less than 18 years of age.
Use: To improve glycemic control in children with type 2 diabetes mellitus as an adjunct to diet and exercise.
What other drugs will affect Glucophage?
Many drugs can interact with metformin, making it less effective or increasing your risk of lactic acidosis. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed here. Tell your doctor about all your current medicines and any medicine you start or stop using.
Popular FAQ
How long does metformin take to work?
Metformin will usually start lowering your blood sugar (glucose) levels in the first week of treatment, but it may take 2 to 3 months to see its full effect. Metformin is a preferred initial oral treatment for people with type 2 diabetes, and is usually taken on a long-term basis. It may be combined with other blood glucose-lowering treatments, if needed. Continue reading
Is Ozempic better than metformin?
Ozempic (semaglutide) and metformin have not been directly compared in head-to-head clinical studies, so it is difficult to know if one works better than the other to treat type 2 diabetes. In separate studies, metformin and Ozempic lowered hemoglobin A1C by a similar percentage. There are several factors that can help determine if Ozempic or metformin is the best treatment option for you, including route of administration, side effects, and cost. Continue reading
Can you take metformin without food?
If you take metformin without food you may end up with an upset stomach, especially if you are just starting treatment. Nausea and vomiting is one of the most common side effects with metformin and can occur in over a quarter of patients. Continue reading
Why does Metformin smell like fish?
Pharmacists and patients are well aware that metformin may come with a fishy smell when you open the bottle. The smell does not mean the drug is spoiled, it's just due to it's inherent chemical characteristics. Continue reading
When is the best time to take metformin?
Metformin should be taken after having a meal or eating food, especially when you are first starting treatment. This can help reduce any stomach side effects like nausea, vomiting, diarrhea or gas. These side effects generally go away within a few weeks after starting treatment. Continue reading
What is the safest diabetes medication?
Most experts consider metformin to be the safest medicine for type 2 diabetes because it has been used for many decades, is effective, affordable, and safe. Metformin is recommended as a first-line treatment for type 2 diabetes by the American Diabetes Association (ADA).
Continue readingWhy does metformin cause diarrhea?
According to the manufacturer, about 53% of people taking metformin immediate-release tablets experienced diarrhea in one clinical study. In another study, 10% of people taking metformin extended-release tablets reported diarrhea as a side effect. Continue reading
More FAQ
- How long does glucophage/Metformin stay in your system?
- What are the ingredient drugs contained in Qternmet XR?
More about Glucophage (metformin)
- Check interactions
- Compare alternatives
- Reviews (39)
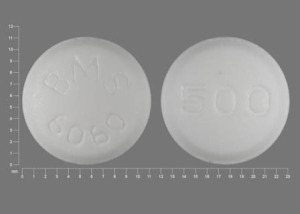
- Drug images
- Latest FDA alerts (18)
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- Support group
- Drug class: non-sulfonylureas
- Breastfeeding
Patient resources
Other brands
Glumetza, Fortamet, Riomet, Riomet ER
Professional resources
Other brands
Glumetza, Glucophage XR, Fortamet, Riomet
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use Glucophage only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 19.01.