Segluromet
Generic name: ertugliflozin and metformin [ ER-too-gli-FLOE-zin-and-met-FOR-min ]
Drug class: Antidiabetic combinations
What is Segluromet?
Segluromet contains a combination of ertugliflozin and metformin which help control blood sugar levels. Ertugliflozin works by helping the kidneys get rid of glucose from your bloodstream. Metformin works by helping your liver release lower amounts of sugar into your blood.
Segluromet is used together with diet and exercise to improve blood sugar control in adults with type 2 diabetes mellitus.
Segluromet is not for treating type 1 diabetes.
Warnings
You should not use Segluromet if you have severe kidney disease, if you are on dialysis, or if you have diabetic ketoacidosis.
Ertugliflozin may increase your risk of lower leg amputation, especially if you have had a prior amputation, a foot ulcer, heart disease, circulation problems, or nerve damage.
If you need to have any type of x-ray or CT scan using a dye that is injected into your veins, you may need to temporarily stop taking Segluromet.
Ertugliflozin can cause serious infections in the penis or vagina. Get medical help right away if you have burning, itching, odor, discharge, pain, tenderness, redness or swelling of the genital or rectal area, fever, or if you don't feel well.
You may develop lactic acidosis, a dangerous build-up of lactic acid in your blood. Get emergency medical help if you have even mild symptoms such as: unusual muscle pain, numb or cold feeling in your arms and legs, trouble breathing, stomach pain, nausea with vomiting, irregular heart rate, dizziness, or feeling very weak or tired.
Before taking this medicine
You should not use Segluromet if you are allergic to ertugliflozin or metformin, or if you have:
-
severe kidney disease (or if you are on dialysis); or
-
diabetic ketoacidosis (call your doctor for treatment).
If you need to have any type of x-ray or CT scan using a dye that is injected into your veins, you may need to temporarily stop taking this medicine.
Ertugliflozin may increase your risk of lower leg amputation, especially if you have had a prior amputation, a foot ulcer, heart disease, circulation problems, or nerve damage.
To make sure Segluromet is safe for you, tell your doctor if you have ever had:
-
heart problems;
-
a diabetic foot ulcer or amputation;
-
circulation problems or nerve problems in your legs or feet;
-
liver or kidney disease;
-
high ketone levels in your blood or urine;
-
bladder infections or other urination problems;
-
problems with your pancreas, including surgery;
-
if you drink alcohol often; or
-
if you are on a low salt diet.
You may develop lactic acidosis, a dangerous build-up of lactic acid in your blood. This may be more likely if you have other medical conditions, a severe infection, chronic alcoholism, or if you are 65 or older. Ask your doctor about your risk.
Follow your doctor's instructions about using Segluromet if you are pregnant. Blood sugar control is very important during pregnancy, and your dose needs may be different during each trimester of pregnancy. Having high blood sugar may cause complications in both the mother and the baby.
You should not use Segluromet during the second or third trimester of pregnancy.
Metformin may stimulate ovulation in a premenopausal woman and may increase the risk of unintended pregnancy. Talk to your doctor about your risk.
You should not breastfeed while using this medicine.
Segluromet is not approved for use by anyone younger than 18 years old.
How should I take Segluromet?
Segluromet is usually taken twice per day with meals. Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose.
Segluromet works best if you take it with food.
Call your doctor if you are sick with vomiting or diarrhea, if you consume less food or fluid than usual, or if you are sweating more than usual.
Your blood sugar will need to be checked often, and you may also need to test the level of ketones your urine. Segluromet can cause life-threatening ketoacidosis (too much acid in the blood). Even if your blood sugar is normal, contact your doctor if a urine test shows that you have ketones in the urine.
You may have low blood sugar (hypoglycemia) and feel very hungry, dizzy, irritable, confused, anxious, or shaky. To quickly treat hypoglycemia, eat or drink a fast-acting source of sugar (fruit juice, hard candy, crackers, raisins, or non-diet soda).
Your doctor may prescribe a glucagon injection kit in case you have severe hypoglycemia. Be sure your family or close friends know how to give you this injection in an emergency.
Also watch for signs of high blood sugar (hyperglycemia) such as increased thirst or urination.
Blood sugar levels can be affected by stress, illness, surgery, exercise, alcohol use, or skipping meals. Ask your doctor before changing your dose or medication schedule.
This medicine can cause unusual results with certain lab tests. Tell any doctor who treats you that you are using Segluromet.
Segluromet is only part of a complete treatment program that may also include diet, exercise, weight control, regular blood sugar testing, and special medical care. Follow your doctor's instructions very closely.
Your doctor may have you take extra vitamin B12. Take only the amount of vitamin B12 that your doctor has prescribed.
Store Segluromet at room temperature away from moisture and heat.
Dosing information
Usual Adult Dose of Segluromet for Diabetes Type 2:
Individualize dose based on current regimen:
Initial dose: 1 tablet orally twice a day
-For patients on metformin: Start with tablet containing ertugliflozin 2.5 mg and one-half total daily dose of metformin
-For patients on ertugliflozin: Start with tablet containing one-half daily dose of ertugliflozin and metformin 500 mg
-For patients already treated with ertugliflozin and metformin: Start with tablet that provides one-half total daily dose of ertugliflozin and one-half of similar daily dose of metformin
Adjust dose based on effectiveness and tolerability
Maximum daily dose: Ertugliflozin 15 mg; Metformin 2000 mg
Comments:
-Volume depletion should be corrected prior to therapy initiation.
-Metformin dose should be gradually increased to reduce gastrointestinal side effects; taking with meals will also reduce gastrointestinal effects.
-This drug is not recommended for patients with type 1 diabetes mellitus or for the treatment of diabetic ketoacidosis.
Use: As an adjunct to diet and exercise to improve glycemic control in adults with Type 2 diabetes mellitus who are not adequately controlled on a regimen containing ertugliflozin or metformin, or in patients who are already treated with both ertugliflozin and metformin.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. An overdose can cause lactic acidosis.
What to avoid
Avoid drinking alcohol. It lowers blood sugar and may increase your risk of lactic acidosis.
Avoid getting up too fast from a sitting or lying position, or you may feel dizzy.
Segluromet side effects
Get emergency medical help if you have signs of an allergic reaction to Segluromet: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Seek medical attention right away if you have signs of a genital infection (penis or vagina): burning, itching, odor, discharge, pain, tenderness, redness or swelling of the genital or rectal area, fever, not feeling well. These symptoms may get worse quickly.
Call your doctor at once if you have:
-
new pain, tenderness, sores, ulcers, or infections in your legs or feet;
-
little or no urination;
-
lactic acidosis - unusual muscle pain, trouble breathing, stomach pain, vomiting, irregular heart rate, dizziness, feeling cold, or feeling very weak or tired;
-
ketoacidosis (too much acid in the blood) - nausea, vomiting, stomach pain, confusion, unusual drowsiness, or trouble breathing;
-
dehydration symptoms - dizziness, weakness, feeling light-headed (like you might pass out); or
-
signs of a bladder infection - pain or burning when you urinate, increased urination, blood in your urine, fever, pain in your pelvis or back.
Some side effects may be more likely to occur in older adults.
Common Segluromet side effects may include:
-
genital yeast infection;
-
stomach discomfort;
-
nausea, vomiting, diarrhea, gas;
-
headache, weakness; or
-
urinating more than usual.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
What other drugs will affect Segluromet?
When you start or stop taking Segluromet, your doctor may need to adjust the doses of any other diabetes medicines you use on a regular basis.
Other drugs may interact with ertugliflozin and metformin, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell your doctor about all your current medicines and any medicine you start or stop using.
Frequently asked questions
More about Segluromet (ertugliflozin / metformin)
- Check interactions
- Compare alternatives
- Pricing & coupons
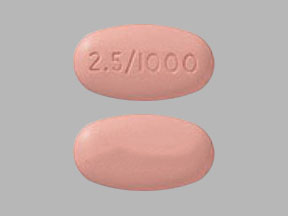
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: antidiabetic combinations
- En español
Professional resources
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use Segluromet only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 4.02.