Prialt: Package Insert / Prescribing Info
Package insert / product label
Generic name: ziconotide acetate
Dosage form: injection, solution
Drug class: Miscellaneous analgesics
J Code (medical billing code): J2278 (1 mcg, injection)
Medically reviewed by Drugs.com. Last updated on Jul 16, 2025.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
PRIALT (ziconotide) solution, intrathecal infusion
Initial U.S. Approval: 2004
WARNING: NEUROPSYCHIATRIC ADVERSE REACTIONS
See full prescribing information for complete boxed warning
Severe psychiatric symptoms and neurological impairment may occur during treatment with PRIALT. Do not treat patients with a pre-existing history of psychosis with PRIALT
Indications and Usage for Prialt
PRIALT (ziconotide) solution, intrathecal infusion is an N-type calcium channel antagonist indicated for the management of severe chronic pain in patients for whom intrathecal therapy is warranted, and who are intolerant of or refractory to other treatment, such as systemic analgesics, adjunctive therapies, or intrathecal morphine. (1)
Prialt Dosage and Administration
PRIALT is a non-opioid and non-NSAID analgesic agent used for the management of severe and chronic pain. Administer PRIALT intrathecally by or under the direction of a physician experienced in the technique of intrathecal administration and who is familiar with the drug and device labeling. (2)
- PRIALT is not for intravenous administration. (2.1)
- PRIALT is delivered using a programmable implanted variable-rate microinfusion device or an external microinfusion device and catheter. (2.1)
- PRIALT 25 mcg/mL is used undiluted. The 100 mcg/mL formulation must be used diluted until an appropriate dose has been established. (2.1)
- Saline solutions containing preservatives must not be used. (2.1)
- Refrigerate but do not freeze all PRIALT solutions after preparation. Begin infusion within 24 hours. (2.1)
- Initiate PRIALT at no more than 2.4 mcg/day (0.1 mcg/hr) and titrated to patient response. Doses may be titrated upward by up to 2.4 mcg/day (0.1 mcg/hr) at intervals of no more than 2–3 times per week, up to a recommended maximum of 19.2 mcg/day (0.8 mcg/hr) by Day 21. (2)
Dosage Forms and Strengths
Intrathecal solution (3):
- 25 mcg/mL
- 100 mcg/mL
Contraindications
- Patients with a known hypersensitivity to ziconotide or any of its formulation components and in patients with any other concomitant treatment or medical condition that would render intrathecal administration hazardous. (4)
- Patients with a pre-existing history of psychosis with ziconotide. (4)
- Contraindications to the use of intrathecal analgesia include conditions such as the presence of infection at the microinfusion injection site, uncontrolled bleeding diathesis, and spinal canal obstruction that impairs circulation of cerebrospinal fluid (CSF). (4)
Warnings and Precautions
- Cognitive and neuropsychiatric adverse reactions – Cognitive impairment and severe neuropsychiatric symptoms may occur with PRIALT use. (5.1)
- Meningitis and other infections – Patients, caregivers, and healthcare providers must be aware of the signs and symptoms of meningitis, including but not limited to fever, headache, stiff neck, altered mental status (e.g., lethargy, confusion, disorientation), nausea or vomiting, and occasionally seizures. (5.2)
- Reduced level of consciousness – Patients may become unresponsive or stuporous while receiving PRIALT. (5.3)
- Elevation of serum creatine kinase – Patients taking PRIALT may experience elevations in creatine kinase. Monitor serum CK in patients undergoing treatment with PRIALT periodically. (5.4)
- Withdrawal from opiates: Patients must not be abruptly withdrawn from opiates and must be gradually tapered over a few weeks and replaced with a pharmacologically equivalent dose of oral opiates. (5.5)
Adverse Reactions/Side Effects
The most frequently reported adverse reactions (≥ 25%) in clinical trials were dizziness, nausea, confusional state, nystagmus. (6)
To report SUSPECTED ADVERSE REACTIONS, contact TerSera Therapeutics at 1-844-344-4035 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
Drug Interactions
- Combination of PRIALT with intrathecal opiates is not recommended. (7)
- Patients taking concomitant antiepileptics, neuroleptics, sedatives, or diuretics may be at higher risk of depressed levels of consciousness. (5.3)
- The use of PRIALT may be associated with an increased incidence of CNS adverse reactions such as dizziness and confusion. (7.1)
Use In Specific Populations
- Geriatric Use: There is a higher incidence of confusion in elderly patients. The dose selection for an elderly patient should be cautious, starting at the low end of the dosing range. (8.5)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2025
Full Prescribing Information
WARNING: NEUROPSYCHIATRIC ADVERSE REACTIONS
PRIALT is contraindicated in patients with a preexisting history of psychosis. Severe psychiatric symptoms and neurological impairment may occur during treatment with PRIALT. Monitor all patients frequently for evidence of cognitive impairment, hallucinations, or changes in mood or consciousness. Discontinue PRIALT therapy in the event of serious neurological or psychiatric signs or symptoms.
1. Indications and Usage for Prialt
PRIALT (ziconotide) solution, intrathecal infusion is indicated for the management of severe chronic pain in adult patients for whom intrathecal therapy is warranted, and who are intolerant of or refractory to other treatment, such as systemic analgesics, adjunctive therapies, or intrathecal morphine.
2. Prialt Dosage and Administration
2.1 General Information
PRIALT is intended for administration by or under the direction of a physician experienced in the technique of intrathecal administration and who is familiar with the drug and device labeling.
PRIALT is not intended for intravenous administration.
PRIALT is intended for intrathecal delivery using the Medtronic SynchroMed® II and SynchroMed® III Infusion System [see Warnings and Precautions (5.2)]. Refer to the manufacturer's manual for specific instructions and precautions for programming the microinfusion device and/or refilling the reservoir.
PRIALT may be used for therapy undiluted (25 mcg/mL in 20 mL vial) or diluted (100 mcg/mL in 1 or 5 mL vials). The 100 mcg/mL formulation may be administered undiluted once an appropriate dose has been established.
Dilute PRIALT with 0.9% Sodium Chloride Injection, USP (preservative free) using aseptic procedures to the desired concentration prior to placement in the microinfusion pump.
- Saline solutions containing preservatives are not appropriate for intrathecal drug administration and should not be used due to risk of neurotoxicity.
- Refrigerate but do not freeze all PRIALT solutions after preparation and begin infusion within 24 hours.
Inspect vials of PRIALT visually for particulate matter and discoloration prior to administration whenever solution and container permit. Discard any PRIALT solution with observed particulate matter or discoloration and any unused portion left in the vial.
2.2 Dosing
Dose Initiation
Initiate dosing with PRIALT via intrathecal device at no more than 2.4 mcg/day (0.1 mcg/hr).
Dose Titration
Titrate doses by up to 2.4 mcg/day (0.1 mcg/hr) at intervals of no more than 2 to 3 times per week based on analgesic response and adverse events. Dose increases in increments of less than 2.4 mcg/day (0.1 mcg/hr) and less frequently than 2 to 3 times per week may be used. For each dose titration, assess the dosing requirements and adjust the pump infusion flow rate as required to achieve the new dosing.
The maximum recommended dose is 19.2 mcg/day (0.8 mcg/hr).
Adjust the dose of intrathecal PRIALT according to the severity of pain, the patient's response to therapy, and the occurrence of adverse reactions.
2.3 Instructions for Use with the Medtronic SynchroMed II and SynchroMed III Infusion System
Refer to the manufacturer's manuals for specific instructions and precautions for performing a reservoir rinse, initial filling, refilling the reservoir, and programming. [see Warnings and Precautions (5.2)]
Naïve Pump Priming (i.e., first time use with PRIALT)
Use only the undiluted 25 mcg/mL formulation for naïve pump priming. Rinse the internal surfaces of the pump with 2 mL of PRIALT at 25 mcg/mL. Repeat twice for a total of three rinses.
Initial Pump Fill
Use only the undiluted 25 mcg/mL formulation for the initial pump fill. Fill the naïve pump after priming with the appropriate volume of PRIALT 25 mcg/mL. Begin dosing at a delivery rate no higher than 2.4 mcg/day (0.1 mcg/hr). In a naïve pump, PRIALT is lost due to two factors that do not occur upon subsequent refills: adsorption on internal device surfaces, such as titanium, and by dilution in the residual space of the device. Consequently, the pump reservoir should be refilled with PRIALT within 14 days of the initial fill to ensure appropriate dose administration.
Pump Refills
For subsequent pump refills, fill the pump at least every 40 days if PRIALT is used diluted. For undiluted PRIALT, fill the pump at least every 84 days. To ensure aseptic transfer of PRIALT into the device, use the Medtronic refill kit. Empty the pump contents prior to refill with PRIALT.
If the internal infusion system must be surgically replaced while the person is receiving PRIALT, rinse the replacement pump with PRIALT according to Naïve Pump Priming [see Dosage and Administration (2.4)], and replace the initial fill solution within 14 days according to Initial Pump Fill [see Dosage and Administration (2.4)].
| PRIALT
(ziconotide) solution, intrathecal infusion | Initial Fill
Expiry | Refill
Expiry |
| 25 mcg/mL, undiluted | 14 Days | 84 Days |
| 100 mcg/mL, undiluted | N/A | 84 Days |
| 100 mcg/mL, diluted | N/A | 40 Days |
3. Dosage Forms and Strengths
PRIALT (ziconotide) solution, intrathecal infusion is supplied as a 25 mcg/mL concentration in single-use 20 mL glass vials and as a 100 mcg/mL concentration in single-use glass vials containing 1 mL or 5 mL of solution.
4. Contraindications
- PRIALT is contraindicated in patients with a known hypersensitivity to ziconotide or any of its formulation components.
- PRIALT is contraindicated in patients with any other concomitant treatment or medical condition that would render intrathecal administration hazardous. Contraindications to the use of intrathecal analgesia include the presence of infection at the microinfusion injection site, uncontrolled bleeding diathesis, and spinal canal obstruction that impairs circulation of CSF.
- PRIALT is contraindicated in patients with a pre-existing history of psychosis.
5. Warnings and Precautions
5.1 Cognitive and Neuropsychiatric Adverse Reactions
Severe psychiatric symptoms and neurological impairment may occur during treatment with PRIALT. PRIALT is contraindicated in patients with a pre-existing history of psychosis. Monitor all patients frequently for evidence of cognitive impairment, hallucinations, or changes in mood or consciousness. PRIALT therapy can be interrupted or discontinued abruptly without evidence of withdrawal effects in the event of serious neurological or psychiatric signs or symptoms.
Events of acute psychiatric disturbances such as hallucinations (12%), paranoid reactions (3%), hostility (2%), delirium (2%), psychosis (1%), and manic reactions (0.4%) have been reported in patients treated with PRIALT. Patients with pretreatment psychiatric disorders may be at an increased risk. PRIALT may cause or worsen depression with the risk of suicide in susceptible patients. In placebo-controlled trials, there was a higher incidence of suicide, suicide attempts, and suicide ideations in PRIALT-treated patients than in the placebo group (0.27/patient year for PRIALT patients and 0.10/patient year for placebo patients).
Management of psychiatric complications may need to include discontinuation of PRIALT, treatment with psychotherapeutic agents and/or short-term hospitalization. Before drug is reinitiated, careful evaluation must be performed on an individual basis.
Use of PRIALT has been associated with cognitive impairment and decreased alertness/unresponsiveness. The following cognitive adverse reaction rates were reported: confusion (33%), memory impairment (22%), speech disorder (14%), aphasia (12%), thinking abnormal (8%), and amnesia (1%). Cognitive impairment may appear gradually after several weeks of treatment. Reduce the dose of PRIALT or discontinue the use of PRIALT if signs or symptoms of cognitive impairment develop, but other contributing causes must also be considered. The cognitive effects of PRIALT are generally reversible within 2 weeks after drug discontinuation. The median time to reversal of the individual cognitive effects ranged from 3 to 15 days. The elderly (≥ 65 years of age) are at higher risk for confusion. [see Use in Specific Populations (8.5)]
There may be additive effects on cognitive impairment and decreased alertness when PRIALT is used in conjunction with other CNS-depressant drugs that may necessitate dosage adjustments.
5.2 Meningitis and Other Infections
Meningitis can occur due to inadvertent contamination of the microinfusion device and other means such as CSF seeding due to hematogenous or direct spread from an infected pump pocket or catheter tract. While meningitis is rare with an internal microinfusion device and surgically-implanted catheter, the incidence increases substantially with external devices. In PRIALT clinical trials, meningitis occurred in 3% (40) of patients in the PRIALT group using either internal or external microinfusion devices and 1% (1 case) of patients in the placebo group.
The risk of meningitis was particularly high in patients with external microinfusion devices and catheters, occurring in 38 out of 41 patients (93%), 37 of whom received PRIALT and one who received placebo.
Patients, caregivers, and healthcare providers must be particularly vigilant for the signs and symptoms of meningitis, including but not limited to fever, headache, stiff neck, altered mental status (e.g., lethargy, confusion, disorientation), nausea or vomiting, and occasionally seizures. Serious infection or meningitis can occur within 24 hours of a breach in sterility such as a disconnected catheter, the most common cause of meningitis with external microinfusion devices. The patient and health care provider must be familiar with the handling of the external microinfusion device and care of the catheter skin exit site.
Strict aseptic procedures must be used during the preparation of the PRIALT solution and refilling of the microinfusion device to decrease the risk of introducing contaminants or other environmental pathogens into the reservoir. In suspected cases (especially in immuno-compromised patients) or in confirmed cases of meningitis, CSF cultures must be obtained and appropriate antibiotic therapy must be promptly instituted. Treatment of meningitis usually requires removal of the microinfusion system, catheter, and any other foreign body materials within the intrathecal space and, therefore, discontinuation of PRIALT therapy.
5.3 Reduced Level of Consciousness
Patients have become unresponsive or stuporous while receiving PRIALT. The incidence of unresponsiveness or stupor in clinical trials was 2% in PRIALT-treated patients. During these episodes, patients sometimes appear to be conscious and breathing is not depressed. If reduced levels of consciousness occur, discontinue PRIALT until the event resolves, and other etiologies (e.g., meningitis) must be considered. There is no known pharmacologic antagonist for this effect. Patients taking concomitant antiepileptics, neuroleptics, sedatives, or diuretics may be at higher risk of depressed levels of consciousness. If altered consciousness occurs, discontinue other CNS-depressant drugs as clinically appropriate.
5.4 Elevation of Serum Creatine Kinase
In clinical studies, 40% of PRIALT-treated patients had serum creatine kinase (CK) levels above the upper limit of normal (ULN), and 11% had CK levels that were greater than three times the ULN. In cases where CK was fractionated, only the muscle isoenzyme (MM) was elevated. The time to occurrence was sporadic, but the greatest incidence of CK elevation was during the first two months of treatment. One case of symptomatic myopathy with EMG findings, and two cases of acute renal failure associated with rhabdomyolysis and extreme CK elevations (17,000–27,000 IU/L) have been reported in PRIALT-treated patients.
Therefore, monitor serum CK in patients undergoing treatment with PRIALT periodically (e.g., every other week for the first month and monthly as appropriate thereafter). Evaluate patients clinically and obtain CK measurements in the setting of new neuromuscular symptoms (e.g., myalgias, myasthenia, muscle cramps, asthenia) or a reduction in physical activity. If these symptoms continue and CK levels remain elevated or continue to rise, reduce the dose or discontinue the use of PRIALT.
5.5 Withdrawal From Opiates
PRIALT is not an opiate and cannot prevent or relieve the symptoms associated with the withdrawal of opiates.
To avoid withdrawal syndrome when opiate withdrawal is necessary, do not abruptly reduce or withdraw opioid medications.
For patients being withdrawn from intrathecal opiates or intrathecal opiate infusion, gradually taper over a few weeks and replace with a pharmacologically equivalent dose of oral opiates.
5.6 Driving and Operating Machinery
Use of PRIALT has been associated with cognitive impairment and decreased alertness/unresponsiveness. Therefore, caution patients against engaging in hazardous activities that require complete mental alertness or motor coordination such as operating machinery or driving a motor vehicle.
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates in clinical practice.
A total of 1254 adult patients received PRIALT as a continuous infusion in acute and severe chronic pain trials with an exposure of 662 patient-years. The mean duration of treatment was 193 days with 173 patients (14%) treated for at least 1 year. The average final dose was 17.6 mcg/day (0.73 mcg/hr).
The most frequently reported adverse reactions (≥ 25%) in clinical trials were dizziness, nausea, confusional state and nystagmus. Slower titration of PRIALT may result in fewer serious adverse reactions and discontinuation of PRIALT for adverse reactions [see Clinical Studies (14) and Dosage and Administration (2)].
Adverse reactions during the slow titration placebo-controlled trial that occurred in 5% or greater of patients and more commonly with PRIALT than with placebo are summarized in Table 1.
| MedDRA System Organ Class
MedDRA Preferred term | PRIALT
N=112 | Placebo
N=108 |
| Percentage of Patients | ||
| Any AE | 93 | 82 |
| Ear and Labyrinth Disorders | ||
| Vertigo | 7 | 0 |
| Eye Disorders | ||
| Vision Blurred | 12 | 3 |
| Gastrointestinal Disorders | ||
| Diarrhea | 18 | 15 |
| Nausea | 40 | 29 |
| Vomiting | 16 | 14 |
| General Disorders and Administration Site Conditions | ||
| Asthenia | 18 | 6 |
| Gait Abnormal | 14 | 2 |
| Pyrexia | 5 | 3 |
| Rigors | 7 | 5 |
| Infections and Infestations | ||
| Sinusitis | 5 | 2 |
| Metabolism and Nutrition Disorders | ||
| Anorexia | 6 | 2 |
| Musculoskeletal and Connective Tissue Disorders | ||
| Muscle Spasms | 6 | 4 |
| Pain in Limb | 5 | 2 |
| Nervous System Disorders | ||
| Amnesia | 8 | 0 |
| Ataxia | 14 | 1 |
| Dizziness | 46 | 13 |
| Dysarthria | 7 | 0 |
| Dysgeusia | 5 | 5 |
| Headache | 13 | 11 |
| Memory Impairment | 7 | 1 |
| Nystagmus | 8 | 0 |
| Somnolence | 17 | 10 |
| Tremor | 7 | 3 |
| Psychiatric Disorders | ||
| Anxiety | 8 | 3 |
| Confusional State | 15 | 5 |
| Insomnia | 6 | 9 |
| Renal and Urinary Disorders | ||
| Urinary Retention | 9 | 0 |
| Skin and Subcutaneous Disorders | ||
| Pruritis | 7 | 7 |
| Sweating Increased | 5 | 6 |
Other Adverse Reactions Observed During Clinical Studies of PRIALT
The following adverse reactions assessed as related to PRIALT have been reported in 2% or greater of patients participating in the clinical studies:
EYE DISORDERS: diplopia, visual disturbance
GASTROINTESTINAL DISORDERS: abdominal pain, constipation, dry mouth, nausea aggravated
GENERAL DISORDERS AND ADMINISTRATION SITE CONDITIONS: fall, fatigue, lethargy, edema peripheral
INVESTIGATIONS: blood creatine phosphokinase increased
METABOLISM AND NUTRITION DISORDERS: appetite decreased
MUSCULOSKELETAL AND CONNECTIVE TISSUE DISORDERS: muscle cramp, muscle weakness, myalgia, pain in limb
NERVOUS SYSTEM DISORDERS: aphasia, areflexia, balance impaired, burning sensation, coordination abnormal, disturbance in attention, dizziness postural, dysarthria, dysgeusia, hypoaesthesia, mental impairment, paraesthesia, sedation, speech disorder
PSYCHIATRIC DISORDERS: agitation, anxiety, cognitive disorder, confusional state, depression, depression aggravated, disorientation, hallucination, hallucination auditory, hallucination visual, insomnia, irritability, mood disorder, nervousness, paranoia
RENAL AND URINARY DISORDERS: dysuria, urinary hesitation
VASCULAR DISORDERS: hypotension, orthostatic hypotension.
The following medically important adverse reactions occurred in less than 2% of patients were assessed by the clinical investigators as related to PRIALT: acute renal failure, atrial fibrillation, cerebrovascular accident, sepsis, meningitis, psychotic disorder, suicidal ideation, respiratory distress, rhabdomyolysis, electrocardiogram abnormal, stupor, loss of consciousness, clonic convulsion and grand mal convulsion. Fatal aspiration pneumonia and suicide attempt were reported in less than 1% of patients.
6.2 Postmarketing Experience
The following adverse events have been reported during post-approval use of PRIALT. Because these events are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure: Hypersensitivity reactions including angioedema, serious skin reactions including bullous dermatitis, skin ulcers, skin exfoliation, and burning skin sensation.
Related/similar drugs
7. Drug Interactions
Formal PK drug-drug interaction studies have not been performed with PRIALT. As ziconotide is a peptide, it is expected to be completely degraded by endopeptidases and exopeptidases (Phase I hydrolytic enzymes) widely located throughout the body, and not by other Phase I biotransformation processes (including the cytochrome P450 system) or by Phase II conjugation reactions. Thus, intrathecal administration, low plasma ziconotide concentrations, and metabolism by ubiquitous peptidases make metabolic interactions of other drugs with ziconotide unlikely. Further, as ziconotide is not highly bound in plasma (approximately 50%) and has low plasma exposure following intrathecal administration, clinically relevant plasma protein displacement reactions involving ziconotide and co-administered medications are unlikely.
Over 90% of patients treated with intrathecal PRIALT used systemic opiates and in the slow titration study, 98% of patients received opioids.
The combination of PRIALT with intrathecal opiates has not been studied in placebo-controlled clinical trials and is not recommended.
7.1 Interaction with CNS Depressants
Almost all patients in the PRIALT clinical trials received concomitant non-intrathecal medication. Most patients received several concomitant drugs, including antidepressants (66%), anxiolytics (52%), antiepileptics (47%), neuroleptics (46%), and sedatives (34%). The use of drugs with CNS-depressant activities may be associated with an increased incidence of CNS adverse reactions such as dizziness and confusion [see Warnings and Precautions (5)].
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Available data from postmarketing reports are insufficient to identify a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. In an animal reproduction study, ziconotide did not cause embryo-fetal toxicity when administered to pregnant rats and rabbits during the period of organogenesis by continuous intravenous infusion at 400- and 940-times, respectively, the maximum recommended human dose (MRHD) of 19.2 mcg/day. In a pre- and post-natal development study, ziconotide did not affect pup development or reproductive performance when administered to rats by continuous intravenous infusion at 3800-times the MRHD (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Animal Data
Ziconotide caused embryo-fetal mortality in rats when given as a continuous intravenous infusion during the major period of organogenesis as evidenced by significant increases in post-implantation loss because of an absence or a reduced number of live fetuses. Estimated exposure for embryo-fetal mortality in the rat was approximately 700-fold above the expected exposure resulting from the maximum recommended human daily intrathecal dose of 0.8 mcg/hr (19.2 mcg/day). Ziconotide did not result in malformations when administered to pregnant rats by continuous intravenous infusion at doses up to 30 mg/kg/day or to pregnant rabbits up to 5 mg/kg/day during the major period of organ development. Estimated exposures in the female rat and rabbit were approximately 26,000-fold and 940-fold higher than the expected exposure resulting from the maximum recommended human daily dose of 0.8 mcg/hr (19.2 mcg/day) based on plasma exposure. Maternal toxicity in the rat and rabbit, as evidenced by decreased body weight gain and food consumption, was present at all dose levels. Maternal toxicity in the rat led to reduced fetal weights and transient, delayed ossification of the pubic bones at doses ≥ 15 mg/kg/day, which is approximately 8900-fold higher than the expected exposure resulting from the maximum recommended human daily intrathecal dose of 0.8 mcg/hr (19.2 mcg/day) based on plasma exposure. The no observable adverse effect level (NOAEL) for embryo-fetal development in rats was 0.5 mg/kg/day and in rabbits was 5 mg/kg/day. Estimated NOAEL exposures in the rat and rabbit were approximately 400-fold and 940-fold higher than the expected exposure resulting from the maximum recommended human daily intrathecal dose of 0.8 mcg/hr (19.2 mcg/day) based on plasma exposure.
In a pre- and post-natal study in rats, ziconotide given as a continuous intravenous infusion did not affect pup development or reproductive performance up to a dose of 10 mg/kg/day, which is approximately 3800-fold higher than the expected exposure resulting from the maximum recommended human daily intrathecal dose of 0.8 mcg/hr (19.2 mcg/day) based on plasma exposure. Maternal toxicity, as evidenced by clinical observations, and decreases in body weight gain and food consumption were observed at all doses.
8.2 Lactation
Risk Summary
There are no data on the presence of ziconotide in either human or animal milk, the effects on the breastfed infant, or the effects on milk production. Infants exposed to PRIALT through breast milk should be monitored for sedation which may result in respiratory depression and/or feeding problems. The developmental and health benefits of breastfeeding should be weighed against the mother´s clinical need for PRIALT and any potential adverse effect on the breastfed infant from PRIALT or from the underlying maternal condition.
8.5 Geriatric Use
Of the total number of subjects in clinical studies of PRIALT, 22% were 65 and over, while 7% were 75 and over. In all trials, there was a higher incidence of confusion in older patients (42% for ≥ 65 year old versus 29% for < 65 year old subgroups). Other reported clinical experience has not identified differences in responses between elderly and younger patients. In general, the dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
10. Overdosage
The maximum recommended intrathecal PRIALT dose is 19.2 mcg/day. The maximum intrathecal dose of PRIALT in clinical trials was 912 mcg/day. In some patients who received intrathecal doses greater than the maximum recommended dose, exaggerated pharmacological effects (e.g., ataxia, nystagmus, dizziness, stupor, unresponsiveness, spinal myoclonus, confusion, sedation, hypotension, word-finding difficulties, garbled speech, nausea, and vomiting) were observed. There was no indication of respiratory depression. Overdoses may occur due to pump programming errors or incorrect drug concentration preparations. In these cases, patients were observed and ziconotide was either temporarily discontinued or permanently withdrawn. Most patients recovered within 24 hours after withdrawal of drug. In the event of an overdose, elimination of ziconotide from CSF would be expected to remain constant (CSF t½=4.6 hours). Therefore, within 24 hours of stopping therapy, the ziconotide CSF concentration should be less than 5% of peak levels.
There is no known antidote to ziconotide. General medical supportive measures should be administered to patients who receive an overdose until the exaggerated pharmacological effects of the drug have resolved. Treatment for an overdose is hospitalization, when needed, and symptom-related supportive care. Ziconotide does not bind to opiate receptors and its pharmacological effects are not blocked by opioid antagonists.
In the event of an inadvertent intravenous or epidural administration, adverse reactions could include severe hypotension, which can be treated with a recumbent posture and blood pressure support as required. The half-life of PRIALT in serum is 1.3 hours.
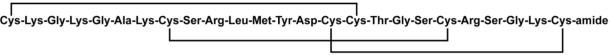
11. Prialt Description
PRIALT contains ziconotide, a synthetic equivalent of a naturally occurring conopeptide found in the piscivorous marine snail, Conus magus. Ziconotide is a 25 amino acid, polybasic peptide containing three disulfide bridges with a molecular weight of 2639 daltons and a molecular formula of C102H172N36O32S7. The amino acid sequence and disulfide bridging pattern are given below:
Ziconotide is a hydrophilic molecule that is freely soluble in water and is practically insoluble in methyl t-butyl ether.
PRIALT is formulated as a sterile, preservative-free, isotonic solution for intrathecal administration using an appropriate microinfusion device [see Dosage and Administration (2)]. Each 1 or 5 mL vial of PRIALT (100 mcg/mL) respectively contains 100 or 500 mcg of ziconotide acetate, and the 20 mL vial of PRIALT (25 mcg/mL) contains 500 mcg of ziconotide acetate, with L-methionine and sodium chloride as excipients at pH 4.0–5.0. Each vial is intended for single use only, either undiluted or after dilution to the appropriate concentration with 0.9% Sodium Chloride Injection, USP (preservative free).
12. Prialt - Clinical Pharmacology
12.1 Mechanism of Action
Ziconotide binds to N-type calcium channels located on the primary nociceptive (A-δ and C) afferent nerves in the superficial layers (Rexed laminae I and II) of the dorsal horn in the spinal cord. Although the mechanism of action of ziconotide has not been established in humans, results in animals suggest that its binding blocks N-type calcium channels, which leads to a blockade of excitatory neurotransmitter release from the primary afferent nerve terminals and antinociception.
12.2 Pharmacodynamics
Interaction with Opioids
Ziconotide does not bind to opioid receptors and its pharmacological effects are not blocked by opioid antagonists. In animal models, intrathecal ziconotide potentiated opioid-induced reduction in gastrointestinal (GI) motility, but did not potentiate morphine-induced respiratory depression. In rats receiving ziconotide, additive analgesic effects were observed with concurrent administration of morphine, baclofen, or clonidine. Concurrent administration of intrathecal ziconotide and morphine did not prevent the development of morphine tolerance in rats.
12.3 Pharmacokinetics
The cerebrospinal fluid (CSF) pharmacokinetics (PK) of ziconotide have been studied after one-hour intrathecal infusions of 1 to 10 mcg of PRIALT to patients with chronic pain. The plasma PK following intravenous infusion (0.3 to 10 mcg/kg/day) have also been studied. Both intrathecal and intravenous data are shown below (Table 2).
| Route | Fluid | N | CL
(mL/min) | Vd
(mL) | T1/2elim
(hr) |
| Intrathecal | CSF | 23 | 0.38 ± 0.56 | 155 ± 263 | 4.6 ± 0.9 |
| Intravenous | Plasma | 21 | 270 ± 44 | 30,460 ± 6366 | 1.3 ± 0.3 |
Following one-hour intrathecal administration of 1 to 10 mcg of PRIALT, both total exposure (AUC; range: 83.6 to 608 ng•h/mL) and peak exposure (Cmax; range: 16.4 to 132 ng/mL) values in the CSF were variable and dose-dependent, but appeared approximately dose-proportional. During 5 or 6 days of continuous intrathecal infusions of PRIALT at infusion rates ranging from 0.1 to 7.0 mcg/hr in patients with chronic pain, plasma ziconotide levels could not be quantified in 56% of patients using an assay with a lower limit of detection of approximately 0.04 ng/mL. Predictably, patients requiring higher intrathecal infusion dose rates were more likely to have quantifiable ziconotide levels in plasma. Plasma ziconotide levels, when detectable, remain constant after many months of intrathecal PRIALT infusion in patients followed for up to 9 months.
Distribution
Ziconotide is about 50% bound to human plasma proteins. The mean CSF volume of distribution (Vd) of ziconotide following intrathecal administration approximates the estimated total CSF volume (140 mL).
Elimination
Metabolism
Ziconotide is cleaved by endopeptidases and exopeptidases at multiple sites on the peptide. Following passage from the CSF into the systemic circulation during continuous intrathecal administration, ziconotide is expected to be susceptible to proteolytic cleavage by various ubiquitous peptidases/proteases present in most organs (e.g., kidney, liver, lung, muscle, etc.), and thus readily degraded to peptide fragments and their individual constituent free amino acids. Human and animal CSF and blood exhibit minimal hydrolytic activity toward ziconotide in vitro. The biological activity of the various expected proteolytic degradation products of ziconotide has not been assessed.
Excretion
Minimal amounts of ziconotide (< 1%) were recovered in human urine following intravenous infusion. The terminal half-life of ziconotide in CSF after an intrathecal administration was around 4.6 hours (range 2.9 to 6.5 hours). Mean CSF clearance (CL) of ziconotide approximates adult human CSF turnover rate (0.3 to 0.4 mL/min).
Specific Populations
No formal studies were conducted to assess the effect of demographic factors (age, race, gender, and weight), renal or hepatic dysfunction, or to assess the effect of concomitant drugs on the pharmacokinetics of ziconotide due to the low systemic exposure of ziconotide following intrathecal administration.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
No carcinogenicity studies have been conducted in animals.
Mutagenesis
Ziconotide was negative in the in vitro bacterial reverse mutation assay, in vitro mouse lymphoma assay, in vivo mouse micronucleus assay, and in the in vitro Syrian hamster embryo (SHE) cell transformation assay.
Impairment of Fertility
Ziconotide did not affect male fertility in rats when administered as a continuous intravenous infusion at a dose of up to 10 mg/kg/day when administered for approximately 8 weeks, including a 28-day pre-mating period, or female fertility at a dose of 3 mg/kg/day when administered for approximately 6 weeks, including a 14-day pre-mating period. Estimated exposures for the male and female rats were approximately 6500-fold and 1700-fold higher, respectively, than the expected exposure resulting from the maximum recommended human daily intrathecal dose of 0.8 mcg/hr (19.2 mcg/day) based on plasma exposure.
Female fertility in rats was significantly affected following continuous intravenous infusion at a dose of 10 mg/kg/day. Significant reductions in corpora lutea, implantation sites, and number of live fetuses were observed.
14. Clinical Studies
The efficacy of intrathecal PRIALT in the management of severe chronic pain was studied in three double-blind, placebo-controlled, multicenter studies in a total of 457 patients (268 PRIALT, 189 placebo) using two different titration schedules. The slow titration schedule tested dose increases 2 to 3 times per week with a maximum dose of 19.2 mcg/day (0.8 mcg/hr) at 21 days. The fast titration schedule used daily increases up to a maximum dose of 57.6 mcg/day (2.4 mcg/hr) in 5 to 6 days but resulted in less tolerability and substantially more frequent adverse events.
A randomized, double-blind, placebo-controlled study of PRIALT was conducted in adult patients with severe chronic pain not adequately controlled with intrathecally delivered analgesics including morphine, bupivacaine and/or clonidine; or who were intolerant to analgesics and/or systemic analgesics using the 21-day slow titration schedule. All prior intrathecal medications were discontinued over a one to three week period, and patients were maintained on a stable regimen of non-intrathecal analgesics, including opiates, for at least 7 days prior to randomization. Dosing with PRIALT was started at 2.4 mcg/day (0.1 mcg/hr) and the dose was increased by 2.4 mcg/day (0.1 mcg/hr) two to three times/week (minimum titration interval 24 hours) to a maximum dose of 19.2 mcg/day (0.8 mcg/hr) as needed for management of pain. The final mean dose at the end of the trial at 21 days was 6.9 mcg/day (0.29 mcg/hr).
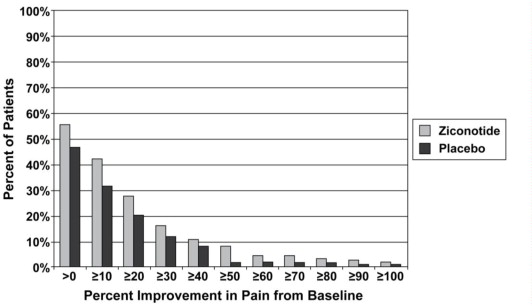
Using a 100 mm Visual Analog Scale of Pain Intensity (VASPI) where 100 mm represented the worst possible pain, mean baseline pain scores were 81 in both the PRIALT and placebo groups. The primary efficacy variable was the mean percent change in the VASPI score from baseline to day 21. In the intent-to-treat efficacy analysis, there was a statistically significant difference between groups in the mean percent change in VASPI score from baseline with the PRIALT group having a 12% mean improvement at Week 3 compared to a 5% mean improvement in the placebo group. The 95% confidence interval for the treatment difference (PRIALT–placebo) was 0.4%, 13%.
The effect of intrathecal PRIALT on pain was variable over the time period of treatment for some patients. Patients exhibited various degrees of improvement in pain after three weeks of treatment compared with baseline pain assessment. Figure 1 depicts the fraction of patients by their degree of improvement. The figure is cumulative, so that patients whose change from baseline is, for example, 30%, are also included at every level of improvement below 30%. Patients who did not have a VASPI score recorded at Week 3 (Study days 17–23, inclusive) were assigned 0% improvement. The improvement in the proportion of “responders,” defined as having a ≥ 30% improvement from baseline in VASPI, was 16% in the PRIALT group compared to 12% in the placebo group, for a net difference of 4%. The use of non-intrathecal opioids decreased by 24% in the PRIALT group and by 17% in the placebo group.
14.1 Laboratory Tests
Monitor serum CK in patients undergoing treatment with PRIALT periodically (e.g., every other week for the first month and monthly as appropriate thereafter). Evaluate patients clinically and obtain CK measurements in the setting of new neuromuscular symptoms (e.g., myalgias, myasthenia, muscle cramps, asthenia) or a reduction in physical activity. If these symptoms continue and CK levels remain elevated or continue to rise, reduce the dose or discontinue the use of PRIALT.
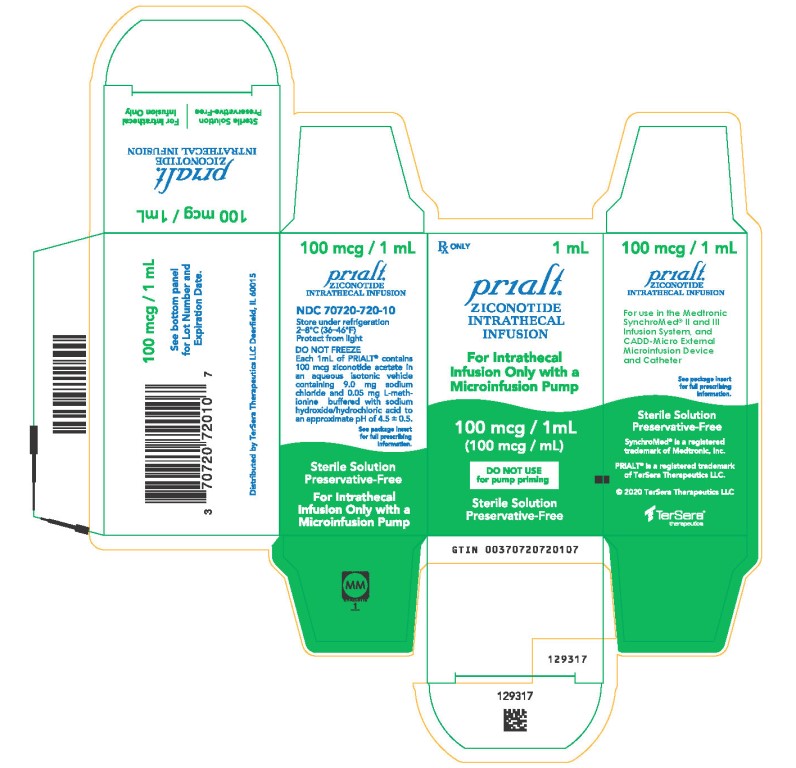
16. How is Prialt supplied
16.1 How Supplied
PRIALT is supplied as a 25 mcg/mL solution in a single-use 20 mL glass vial and as a 100 mcg/mL solution in single-use glass vials containing 1 mL or 5 mL of solution. One vial is packaged per carton.
Presentation (NDC)
25 mcg/mL: 20 mL vial (70720-723-10). Only the undiluted 25 mcg/mL formulation should be used for PRIALT naïve pump priming.
100 mcg/mL: 1 mL vial (70720-720-10)
5 mL vial (70720-722-10)
17. Patient Counseling Information
- Advise patients that psychiatric symptoms (paranoia, hostility, mania, depressive, suicidal) and cognitive symptoms (confusion, memory problems, speech disorder) may occur during treatment with PRIALT.
- Caution patients against engaging in hazardous activity requiring complete mental alertness or motor coordination such as operating machinery or driving a motor vehicle during treatment with PRIALT.
- Caution patients about possible combined effects with other CNS-depressant drugs. Dosage adjustments may be necessary when PRIALT is administered with such agents because of the potentially additive effects.
- Advise patients to contact a physician if the patient experiences new or worsening muscle pain, soreness, weakness with or without darkened urine.
-
Instruct patients and their caregivers to contact a physician immediately if the patient has any of the following
- A change in mental status (e.g., lethargy, confusion, disorientation, decreased alertness)
- A change in mood, perception (hallucinations, including unusual tactile sensations in the oral cavity)
- Symptoms of depression or suicidal ideation
- Nausea, vomiting, seizures, fever, headache, and/or stiff neck, as these may be symptoms of developing meningitis
- Decreased level of consciousness, unresponsiveness or stupor
- New muscular symptoms (e.g., muscle cramps, myalgias)
- Withdrawal symptoms (e.g., nausea, insomnia, flu-like symptoms) as a result of abruptly discontinuing opioid therapy
- Development of serious skin reaction (e.g., bullous dermatitis, skin ulcers, skin exfoliation)
- Lactation: Advise mothers who have been administered PRIALT to monitor neonates for signs of sedation which may result in respiratory depression and/or feeding problems [see Use in Specific Populations (8.2)]
For use only in the Medtronic SynchroMed® II and SynchroMed® III Infusion System.
Distributed by:
TerSera Therapeutics, LLC
Deerfield, IL 60015
© 2023 TerSera Therapeutics
PRIALT® is a registered trademark of TerSera Therapeutics, LLC.
SynchroMed® is a registered trademark of Medtronic, Inc.
U.S. Patent Nos. 5,364,842; 5,795,864; and 5,891,849
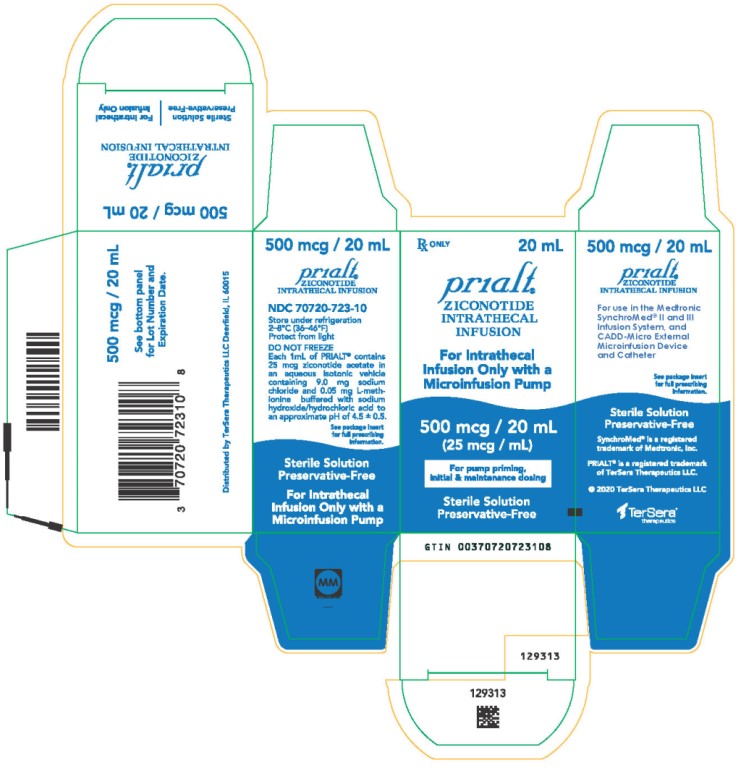
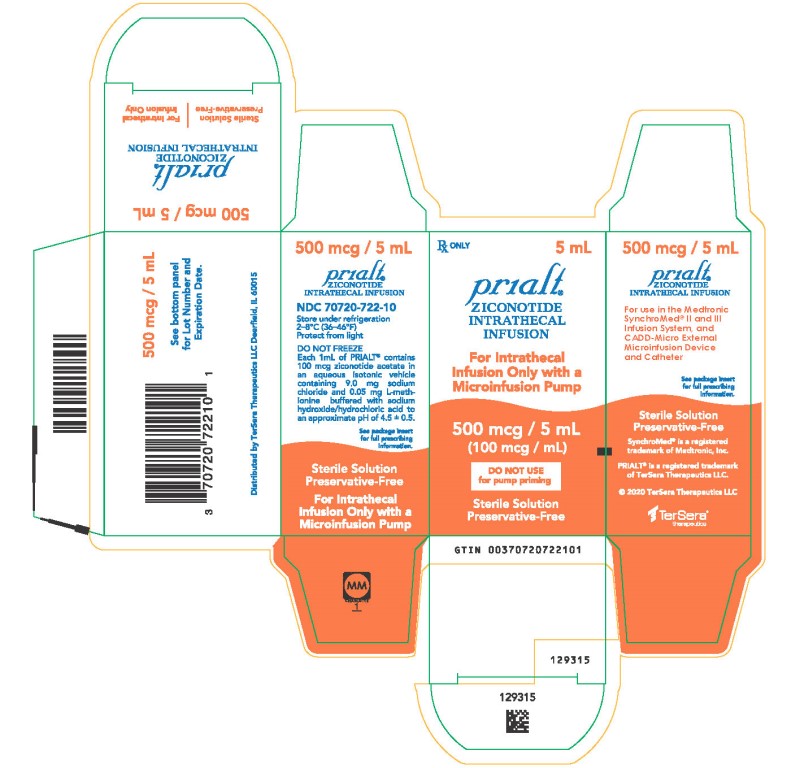
PRINCIPAL DISPLAY PANEL - 20 mL Carton
NDC 70720-723-10
Principal Display Panel
Rx ONLY 20 mL
PRIALT®
(ZICONOTIDE)
INTRATHECAL INFUSION
For Intrathecal
Infusion Only with a
Microinfusion Pump
500 mcg / 20 mL
(25 mcg / mL)
For pump priming,
initial & maintenance dosing
Sterile Solution
Preservative-Free
Left Side Panel
500 mcg / 20 mL
PRIALT®
(ZICONOTIDE)
INTRATHECAL INFUSION
NDC 70720-723-10
Store under refrigeration
2–8°C (36–46°F)
Protect from light
DO NOT FREEZE
Each 1mL of PRIALT® contains
25 mcg ziconotide acetate in
an aqueous isotonic vehicle
containing 9.0 mg sodium
chloride and 0.05 mg L-meth-
ionine buffered with sodium
hydroxide/hydrochloric acid to
an approximate pH of 4.5 ± 0.5.
See package insert
for full prescribing
information.
Sterile Solution
Preservative-Free
For Intrathecal
Infusion Only with a
Microinfusion Pump
Right Side Panel
500 mcg / 20 mL
PRIALT®
(ZICONOTIDE)
INTRATHECAL INFUSION
For use in the Medtronic
SynchroMed® II and III
Infusion System
See package insert
for full prescribing
information.
Sterile Solution
Preservative-Free
SynchroMed® is a registered
trademark of Medtronic, Inc.
PRIALT® is a registered trademark
of TerSera Therapeutics LLC.
TerSera therapeutics
Back Panel
500 mcg / 20 mL
See bottom panel
for Lot Number and
Expiration Date.
Distributed by TerSera Therapeutics LLC Deerfield, IL 60015
| PRIALT
ziconotide acetate injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| PRIALT
ziconotide acetate injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| PRIALT
ziconotide acetate injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - TerSera Therapeutics LLC (080226115) |
More about Prialt (ziconotide)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (12)
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: miscellaneous analgesics
- Breastfeeding
- En español