sAXagliptin (Monograph)
Brand name: Onglyza
Drug class: Dipeptidyl Peptidase-4 (DPP-4) Inhibitors
VA class: HS502
Chemical name: (1S,3S,5S)-2-[(2S)-Amino(3-hydroxytricyclo(3.3.1.13,7)dec-1-yl)acetyl]2-azabicyclo(3.1.0)hexane-3-carbonitrile
Molecular formula: C18H25N3O2•H2O
CAS number: 945667-22-1
Introduction
Antidiabetic agent; dipeptidyl peptidase-4 (DPP-4) inhibitor.
Uses for sAXagliptin
Type 2 Diabetes Mellitus
Used as monotherapy as an adjunct to diet and exercise for management of type 2 diabetes mellitus in patients whose hyperglycemia cannot be controlled by diet and exercise alone.
Used in fixed combination with dapagliflozin (Qtern) or with dapagliflozin and extended-release metformin hydrochloride (Qternmet XR) as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus. Manufacturer states that the fixed combination of dapagliflozin, saxagliptin, and extended-release metformin hydrochloride (Qternmet XR) is intended for use only in patients currently receiving metformin.
Used in combination with metformin (separately or as fixed combination of saxagliptin and extended-release metformin), a sulfonylurea, a thiazolidinedione (e.g., a peroxisome proliferator-activated receptor-γ [PPAR-γ] agonist), or insulin for management of type 2 diabetes mellitus in patients who do not achieve adequate glycemic control with diet, exercise, and metformin, sulfonylurea, thiazolidinedione monotherapy, and/or insulin.
Current guidelines for the treatment of type 2 diabetes mellitus generally recommend metformin as first-line therapy in addition to lifestyle modifications in patients with recent-onset type 2 diabetes mellitus or mild hyperglycemia because of its well-established safety and efficacy (i.e., beneficial effects on glycosylated hemoglobin [hemoglobin A1c; HbA1c], weight, and cardiovascular mortality).
In patients with metformin contraindications or intolerance (e.g., risk of lactic acidosis, GI intolerance) or in selected other patients, some experts suggest that initial therapy with a drug from another class of antidiabetic agents (e.g., a glucagon-like peptide-1 [GLP-1] receptor agonist, sodium-glucose cotransporter 2 [SGLT2] inhibitor, DPP-4 inhibitor, sulfonylurea, thiazolidinedione, basal insulin) may be acceptable based on patient factors.
May need to initiate therapy with 2 agents (e.g., metformin plus another drug) in patients with high initial HbA1c (>7.5% or ≥1.5% above target). In such patients with metformin intolerance, some experts suggest initiation of therapy with 2 drugs from other antidiabetic drug classes with complementary mechanisms of action.
Consider early initiation of combination therapy for the treatment of type 2 diabetes mellitus to extend the time to treatment failure and more rapidly attain glycemic goals.
For patients with inadequate glycemic control on metformin monotherapy, consider patient comorbidities (e.g., atherosclerotic cardiovascular disease [ASCVD], established kidney disease, heart failure), hypoglycemia risk, impact on weight, cost, risk of adverse effects, and patient preferences when selecting additional antidiabetic agents for combination therapy. DPP-4 inhibitors recommended by some experts as one of several classes of drugs for use in combination therapy, particularly in patients with both postprandial and fasting plasma glucose elevations.
Consider early introduction of insulin for severe hyperglycemia (e.g., blood glucose of ≥300 mg/dL or HbA1c >9–10%), especially if accompanied by catabolic manifestations (e.g., weight loss, hypertriglyceridemia, ketosis) or symptoms of hyperglycemia.
Not indicated for type 1 diabetes mellitus or diabetic ketoacidosis.
sAXagliptin Dosage and Administration
Administration
Oral Administration
Saxagliptin Monotherapy
Administer once daily without regard to meals.
If a dose is missed, take missed dose as soon as it is remembered and resume regular schedule. If the missed dose is not remembered until time of next dose, skip missed dose and resume regular schedule. Do not double dose to replace missed dose.
Saxagliptin/Dapagliflozin Fixed Combination
Administer once daily with or without food.
Swallow whole; do not crush, cut, or chew.
If a dose is missed, take missed dose as soon as it is remembered and resume regular schedule. If the missed dose is not remembered until time of next dose, skip missed dose and resume regular schedule. Do not double dose to replace missed dose.
Saxagliptin/Extended-release Metformin Hydrochloride Fixed Combination
Administer once daily with the evening meal, increasing dosage gradually to minimize adverse GI effects of extended-release metformin component.
Swallow whole; do not cut, chew, or crush.
If a dose is missed, take the next dose as prescribed unless a healthcare provider instructs otherwise; do not take an extra dose the next day.
Saxagliptin/Extended-release Metformin Hydrochloride/Dapagliflozin Fixed Combination
Administer once daily in the morning with food; individualize dosage based on patient's current drug regimen, effectiveness, and tolerability.
Swallow whole; do not cut, chew, or crush.
If a dose is missed and it is ≥12 hours before the next scheduled dose, take the missed dose as soon as possible with food. If a dose is missed and it is <12 hours before the next scheduled dose, skip the missed dose and take the next dose at the usual time.
Dosage
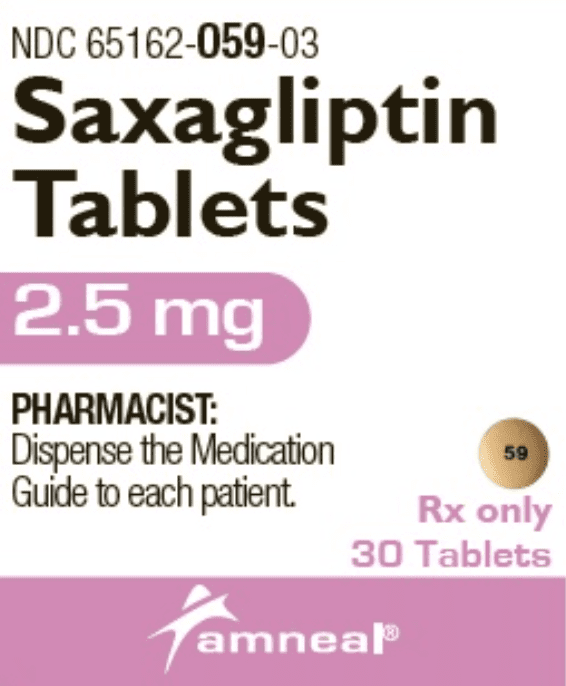
Available as saxagliptin hydrochloride (anhydrous); dosage expressed in terms of saxagliptin.
Adults
Type 2 Diabetes Mellitus
Saxagliptin Monotherapy
Oral2.5 or 5 mg once daily. Higher dosages (e.g., 10 mg once daily) did not provide additional benefit in clinical trials and are not recommended by manufacturer.
If used with a potent CYP3A4/5 inhibitor, limit dosage to 2.5 mg daily. (See Interactions.)
Saxagliptin/Dapagliflozin Fixed-combination Therapy
OralPatients not already receiving dapagliflozin: Initially, 5 mg of saxagliptin and 5 mg of dapagliflozin once daily in the morning.
If additional glycemic control needed and initial dosage tolerated, may increase dosage to 5 mg of saxagliptin and 10 mg of dapagliflozin once daily.
Do not use in patients receiving a potent CYP3A4/5 inhibitor. (See Drugs Affecting Hepatic Microsomal Enzymes under Interactions.)
Saxagliptin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
OralIndividualize dosage based on patient’s current antidiabetic regimen, clinical response, and tolerability. Undertake any change in therapy with caution and appropriate monitoring.
Patients inadequately controlled on monotherapy with saxagliptin 5 mg daily: Initially, 5 mg of saxagliptin and 500 mg of extended-release metformin hydrochloride once daily; increase dosage gradually to minimize adverse GI effects of metformin.
Patients inadequately controlled on monotherapy with extended-release metformin hydrochloride: Dosage of the fixed combination should provide metformin hydrochloride at the current dosage or the nearest therapeutically appropriate dosage. Following a switch from immediate-release to extended-release metformin hydrochloride, glycemic control should be closely monitored and dosage adjusted accordingly.
Patients inadequately controlled on monotherapy with saxagliptin 2.5 mg daily: Initially, 2.5 mg of saxagliptin and 1 g of extended-release metformin hydrochloride daily. Use the individual components in patients who require 2.5 mg of saxagliptin and are either metformin naive or require a metformin hydrochloride dose >1 g.
If used with a potent CYP3A4/5 inhibitor, limit dosage to 2.5 mg of saxagliptin and 1 g of extended-release metformin hydrochloride. (See Drugs Affecting Hepatic Microsomal Enzymes under Interactions.)
Saxagliptin/Extended-release Metformin Hydrochloride/Dapagliflozin Fixed-combination Therapy
Manufacturer states that the fixed-combination preparation containing saxagliptin, extended-release metformin hydrochloride, and dapagliflozin is intended only for patients currently taking metformin hydrochloride. Recommended initial dosage based on patient's current antidiabetic drug regimen.
In patients not already receiving dapagliflozin, recommended initial total daily dosage is saxagliptin 5 mg, extended-release metformin hydrochloride 1 or 2 g, and dapagliflozin 5 mg once daily in the morning.
Do not use in patients receiving a potent CYP3A4/5 inhibitor. (See Drugs Affecting Hepatic Microsomal Enzymes under Interactions.)
Prescribing Limits
Adults
Type 2 Diabetes Mellitus
Oral
Saxagliptin: Maximum 5 mg daily. Dosages >5 mg daily (e.g., 10 mg once daily) did not provide additional benefit in clinical trials and are not recommended by manufacturer.
Fixed combination with extended-release metformin hydrochloride: Maximum 5 mg of saxagliptin and 2 g of metformin hydrochloride daily.
Fixed combination with extended-release metformin hydrochloride and dapagliflozin: Maximum 5 mg of saxagliptin, 2 g of metformin hydrochloride, and 10 mg of dapagliflozin daily.
Special Populations
Hepatic Impairment
Saxagliptin Monotherapy
Oral
Manufacturer makes no recommendation.
Saxagliptin/Dapagliflozin Fixed-combination Therapy
Oral
Manufacturer makes no recommendation.
Saxagliptin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
Oral
Use not recommended.
Renal Impairment
Saxagliptin Monotherapy
Oral
eGFR ≥45 mL/minute per 1.73 m2: No dosage adjustment recommended.
eGFR <45 mL/minute per 1.73 m2: 2.5 mg once daily.
End-stage renal disease requiring hemodialysis: 2.5 mg once daily, following hemodialysis.
Peritoneal dialysis: Not studied.
Saxagliptin/Dapagliflozin Fixed-combination Therapy
Oral
eGFR ≥45 mL/minute per 1.73 m2: No dosage adjustment necessary.
eGFR <45 mL/minute per 1.73 m2: Contraindicated.
End-stage renal disease or requiring hemodialysis: Contraindicated.
Saxagliptin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
Oral
eGFR between 30–45 mL/minute per 1.73 m2: Initiation of the fixed combination not recommended.
eGFR decreases to 30 to <45 mL/minute per 1.73 m2 during therapy: Assess risks and benefits of continuing the fixed combination; limit dosage of saxagliptin component to 2.5 mg once daily.
eGFR <30 mL/minute per 1.73 m2: Contraindicated.
Geriatric Patients
Dosage adjustment of saxagliptin not required based solely on age. Because of the greater frequency of decreased renal function in geriatric patients, select saxagliptin dosage with caution.
Cautions for sAXagliptin
Contraindications
-
Known serious hypersensitivity (e.g., anaphylaxis, angioedema, exfoliative skin reaction) to saxagliptin or any ingredient in the formulation.
Warnings/Precautions
Pancreatitis and Pancreatic Precancerous Changes
Acute pancreatitis reported during postmarketing experience.
FDA has been evaluating unpublished findings suggesting an increased risk of pancreatitis and precancerous pancreatic cell changes in patients with type 2 diabetes mellitus receiving incretin mimetics.
FDA has recommended that clinicians continue to follow the recommendations in the prescribing information for incretin mimetics.
Monitor patients for manifestations of pancreatitis. If pancreatitis is suspected, promptly discontinue saxagliptin and institute appropriate management. Safety and efficacy not established in patients with a history of pancreatitis; unknown whether such patients are at increased risk for pancreatitis.
Severe Arthralgia
Severe, disabling joint pain reported in patients receiving DPP-4 inhibitors (e.g., sitagliptin, saxagliptin, linagliptin, alogliptin). Onset of such symptoms has ranged from 1 day to years following initiation of therapy. Symptoms resolved upon discontinuance of the DPP-4 inhibitor; symptoms recurred in some patients when the same or another DPP-4 inhibitor was restarted.
Consider DPP-4 inhibitors as a possible cause of severe joint pain and discontinue if appropriate. (See Advice to Patients.)
Concomitant Therapy with Hypoglycemic Agents
Increased risk of hypoglycemia in patients receiving saxagliptin in combination with an insulin secretagogue (e.g., sulfonylurea) or insulin; reduction in sulfonylurea or insulin dosage may be necessary.
Reduction in Lymphocyte Counts
Dose-related mean decreases in absolute lymphocyte count reported with saxagliptin dosages of 5 and 10 mg daily; clinical importance not known. When clinically indicated (i.e., settings of unusual or prolonged infection), measure lymphocyte count.
Dermatologic and Sensitivity Reactions
Postmarketing cases of bullous pemphigoid requiring hospitalization reported with DPP-4 inhibitor use. Usually resolved after discontinuation of the DPP-4 inhibitor and treatment with topical or systemic immunosuppressive therapy. Advise patients to report the development of blisters or erosions while receiving saxagliptin. Discontinue drug if bullous pemphigoid is suspected and consider referral to a dermatologist for diagnosis and appropriate treatment.
Risk of serious allergic and hypersensitivity reactions (e.g., anaphylaxis, angioedema, exfoliative skin conditions); rash and urticaria also reported. Onset usually within first 3 months after treatment initiation, but may occur after first dose. (See Cautions: Contraindications.)
If serious hypersensitivity reactions suspected, promptly discontinue drug, assess for other potential causes, institute appropriate treatment, and initiate alternative antidiabetic therapy.
Use caution in patients with a history of angioedema to other DPP-4 inhibitors; unknown whether such patients will be predisposed to angioedema with saxagliptin.
Cardiovascular Effects
Macrovascular Outcomes
Manufacturer states that evidence of macrovascular risk reduction with saxagliptin not conclusively demonstrated in clinical trials.
Heart Failure Risk
Possible increased risk of heart failure, particularly in patients with history of heart failure or renal impairment. In a randomized, placebo-controlled, double-blind study in patients with type 2 diabetes mellitus and established ASCVD or at high risk for ASCVD, hospitalization for heart failure was more common with saxagliptin (27% increased risk versus placebo). Patients with a history of heart failure or renal impairment had higher risk of hospitalization regardless of treatment assignment.
Consider potential risks and benefits of saxagliptin therapy prior to use in patients at higher risk for heart failure. Monitor patients for manifestations of heart failure. (See Advice to Patients.) If heart failure develops, institute appropriate treatment according to current standards of care and consider discontinuance of saxagliptin.
Use of Fixed Combinations
When saxagliptin is used in fixed combination with metformin, dapagliflozin, and/or other drugs, consider the cautions, precautions, contraindications, and drug interactions associated with the concomitant agent(s) in addition to those associated with saxagliptin.
Specific Populations
Pregnancy
Data on use of saxagliptin in pregnant women insufficient to determine a drug-associated risk for major birth defects or miscarriage.
In animal studies, no adverse developmental effects were observed when saxagliptin was administered to pregnant rats and rabbits during organogenesis (at exposures 1503 and 152 times the 5-mg dose, respectively) or in pregnant or lactating rats (at exposures up to 470 times the 5-mg dose) during the prenatal and postnatal period.
Lactation
Saxagliptin distributed into milk in rats; not known whether distributed into human milk. Consider benefits of breast-feeding and the importance of saxagliptin to the woman as well as potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy of saxagliptin alone or in fixed combination with dapagliflozin or extended-release metformin not established in children <18 years of age.
Geriatric Use
No substantial differences in safety and efficacy of saxagliptin relative to younger adults, but increased sensitivity cannot be ruled out.
Saxagliptin eliminated in part by kidneys; assess renal function periodically since geriatric patients are more likely to have decreased renal function.
Hepatic Impairment
Hepatic impairment increases exposure to saxagliptin and its active metabolite; not considered clinically important. (See Special Populations under Pharmacokinetics.)
Fixed combination of saxagliptin and dapagliflozin: May be used in patients with hepatic impairment. However, safety and efficacy not studied in those with severe hepatic impairment; consider benefits and risks of the fixed combination in such patients.
Fixed combination of saxagliptin and extended-release metformin: Not recommended in patients with hepatic impairment.
Renal Impairment
Renal impairment increases exposure to saxagliptin and its active metabolite. (See Special Populations under Pharmacokinetics.) Dosage adjustment for saxagliptin recommended for patients with eGFR <45 mL/minute per 1.73 m2 or end-stage renal disease requiring hemodialysis. (See Renal Impairment under Dosage and Administration.)
Fixed combination of saxagliptin and dapagliflozin: Use contraindicated in patients with eGFR <45 mL/minute per 1.73 m2 or end-stage renal disease and in those requiring hemodialysis.
Fixed combination of saxagliptin and extended-release metformin: Initiation not recommended in patients with eGFR between 30–45 mL/minute per 1.73 m2; contraindicated in patients with eGFR <30 mL/minute per 1.73 m2. (See Renal Impairment under Dosage and Administration.)
Assess renal function prior to initiation of therapy and periodically thereafter.
Common Adverse Effects
Saxagliptin monotherapy: Upper respiratory infection, urinary tract infection, headache.
Saxagliptin in combination with dapagliflozin and metformin: Upper respiratory tract infection, urinary tract infection, dyslipidemia, headache, diarrhea, back pain, genital infection, arthralgia.
Saxagliptin in combination with immediate-release metformin: Headache, nasopharyngitis.
Drug Interactions
Metabolized principally via CYP3A4 and CYP3A5.
Saxagliptin and its active metabolite do not inhibit CYP isoenzymes 1A2, 2A6, 2B6, 2C9, 2C19, 2D6, 2E1, or 3A4 in vitro and do not induce CYP isoenzymes 1A2, 2B6, 2C9, or 3A4 in vitro.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP3A4/5 inhibitors: Substantial increases in saxagliptin plasma concentrations and AUC are expected. Limit saxagliptin dosage to 2.5 mg daily when used concomitantly with a potent CYP3A4/5 inhibitor.
Drugs Metabolized by Hepatic Microsomal Enzymes
Drugs metabolized by CYP isoenzymes 1A2, 2A6, 2B6, 2C9, 2C19, 2D6, 2E1, or 3A4: Pharmacokinetic interactions unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum-, magnesium-, and simethicone-containing) |
Decreased peak concentration of saxagliptin; AUC unchanged |
No dosage adjustment required |
|
Antifungals, azole (e.g., itraconazole, ketoconazole) |
Ketoconazole (potent CYP3A4/5 inhibitor): Decreased peak concentration and AUC of ketoconazole; increased peak concentration and AUC of saxagliptin Itraconazole (potent CYP3A4/5 inhibitor): Substantial increase expected in plasma concentrations and AUC of saxagliptin |
Limit saxagliptin dosage to 2.5 mg daily |
|
Dapagliflozin |
Saxagliptin pharmacokinetics not substantially altered |
No dosage adjustment required |
|
Digoxin |
Pharmacokinetic interaction unlikely |
No dosage adjustment required |
|
Diltiazem |
Increased peak concentration of diltiazem; increased peak concentration and AUC of saxagliptin and 5-hydroxysaxagliptin |
No dosage adjustment required |
|
Famotidine |
Increased peak concentration of saxagliptin |
No dosage adjustment required |
|
HIV protease inhibitors (e.g., atazanavir, indinavir, nelfinavir, ritonavir, saquinavir) |
Substantial increase in plasma concentrations and AUC of saxagliptin expected with concomitant potent CYP3A4/5 inhibitors |
Limit saxagliptin dosage to 2.5 mg daily |
|
Hormonal contraceptives |
Ethinyl estradiol/norgestimate: No appreciable effect on ethinyl estradiol or norgestimate pharmacokinetics |
No dosage adjustment required |
|
Macrolide antibiotics (e.g., clarithromycin) |
Substantial increase in plasma concentrations and AUC of saxagliptin expected with concomitant potent CYP3A4/5 inhibitors |
Limit saxagliptin dosage to 2.5 mg daily |
|
Metformin |
Decreased peak concentration of saxagliptin; no effect on saxagliptin AUC or metformin pharmacokinetics |
No dosage adjustment required |
|
Nefazodone |
Substantial increase in plasma concentrations and AUC of saxagliptin expected with concomitant potent CYP3A4/5 inhibitors |
Limit saxagliptin dosage to 2.5 mg daily |
|
Omeprazole |
Saxagliptin pharmacokinetics not substantially altered |
No dosage adjustment required |
|
Pioglitazone |
Increased peak concentration of pioglitazone; AUC not appreciably altered |
No dosage adjustment required |
|
Rifampin |
Decreased peak concentration and AUC of saxagliptin |
No dosage adjustment required |
|
Simvastatin |
Increased peak concentration and AUC of saxagliptin |
No dosage adjustment required |
|
Sulfonylureas (e.g., glyburide) |
Glyburide: Increased peak concentrations of glyburide and saxagliptin |
May need to decrease sulfonylurea dosage to reduce risk of hypoglycemia |
sAXagliptin Pharmacokinetics
Absorption
Bioavailability
Estimated oral bioavailability is 67%.
Onset
Rapidly absorbed following oral administration; peak plasma concentrations generally attained in 2 hours following administration of recommended doses.
Food
Food does not appear to affect absorption.
Distribution
Extent
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
Negligible.
Elimination
Metabolism
Metabolized principally via CYP3A4 and CYP3A5 to active metabolite 5-hydroxysaxagliptin.
Elimination Route
Saxagliptin and its metabolites excreted in urine and feces.
Half-life
2.5 hours.
Special Populations
Hepatic impairment increases peak concentrations and AUC of saxagliptin by ≤8 and ≤77%, respectively, and increases peak concentrations and AUC of active metabolite by ≤59 and ≤33%, respectively. Not considered clinically important.
Moderate or severe renal impairment increases AUC of saxagliptin and its active metabolite by twofold.
Removed by hemodialysis.
Pharmacokinetics in pediatric patients not elucidated.
Stability
Storage
Oral
Tablets
Saxagliptin, fixed combination of saxagliptin and dapagliflozin, and fixed combination of saxagliptin and extended-release metformin: 20–25°C (may be exposed to 15–30°C).
Actions
-
Inhibits dipeptidyl peptidase-4 (DPP-4), an enzyme that inactivates incretin hormones glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP).
-
More selective for inhibition of DPP-4 than for DPP-8 or DDP-9.
-
Increases circulating concentrations of GIP and GLP-1 in a glucose-dependent manner.
-
GIP and GLP-1 stimulate insulin synthesis and release from pancreatic β-cells in a glucose-dependent manner (i.e., when glucose concentrations are normal or elevated).
-
GLP-1 also decreases glucagon secretion from pancreatic α-cells in a glucose-dependent manner, leading to reduced hepatic glucose production.
-
Lowers fasting plasma glucose concentrations and reduces glucose excursions following glucose load or meal in patients with type 2 diabetes mellitus.
-
Saxagliptin usually not associated with hypoglycemia or substantial changes in body weight.
Advice to Patients
-
When saxagliptin is used in fixed combination with other drugs, importance of informing patients of important cautionary information about the concomitant agent(s).
-
Importance of patients reading patient medication guide before initiating therapy and each time drug is dispensed.
-
Importance of informing patients of the potential risks and benefits of saxagliptin and of alternative therapies. Importance of not using saxagliptin in patients with type 1 diabetes mellitus or diabetic ketoacidosis.
-
Importance of informing patients about possibility of acute pancreatitis, which may be severe or fatal, with saxagliptin therapy. Importance of patients informing clinicians about a history of pancreatitis, gallstones, alcoholism, or high triglyceride levels. Importance of informing patients about signs and symptoms of pancreatitis, including persistent severe abdominal pain sometimes radiating to the back that may or may not be accompanied by vomiting; importance of patient discontinuing saxagliptin and promptly notifying clinician if such signs or symptoms are present.
-
Importance of informing patients of the possibility of severe and disabling joint pain. Advise patients to contact a clinician promptly if severe and persistent joint pain occurs; patients should not discontinue the drug without consulting their clinician.
-
Importance of informing patients about possibility of heart failure with saxagliptin therapy. Importance of clinicians asking patients about a history of heart failure or renal impairment prior to initiating saxagliptin therapy. Importance of informing patients about signs and symptoms of heart failure (e.g., shortness of breath, weight gain, edema); importance of patients immediately contacting a clinician if manifestations of heart failure occur.
-
Importance of informing clinician if hypoglycemia occurs, particularly if concomitant therapy with a sulfonylurea antidiabetic agent (i.e., insulin secretagogue) or insulin is used; a lower dosage of the sulfonylurea or insulin may be required in such cases.
-
Importance of informing patients about the importance of adherence to dietary instructions, regular physical activity, periodic blood glucose monitoring and HbA1c testing, recognition and management of hypoglycemia and hyperglycemia, and assessment of diabetes complications.
-
Importance of seeking medical advice promptly during periods of stress such as fever, trauma, infection, or surgery as medication requirements may change.
Importance of informing patients that response to all diabetic therapies should be monitored by periodic measurements of blood glucose and HbA1c, with a goal of decreasing these levels toward the normal range.
-
Importance of informing patients of the potential need to adjust their dosage based on changes in renal function over time.
-
Importance of informing clinician if any unusual symptom develops or if any existing symptom persists or worsens.
-
Risk of serious allergic (hypersensitivity) reactions, such as angioedema, anaphylaxis, and exfoliative skin conditions. If signs or symptoms of such reactions occur (e.g., rash, skin flaking or peeling, hives, swelling of the skin, swelling of the face, lips, tongue, and throat that may cause difficulty in breathing or swallowing), importance of discontinuing saxagliptin-containing therapy and informing clinician promptly.
-
Importance of informing patients that bullous pemphigoid may occur with the use of a DPP-4 inhibitor. Advise patients to promptly inform clinician if skin blisters or erosion (breakdown of outer layer of skin) occurs.
-
Importance of advising patient not to split, cut, or chew tablets of saxagliptin or the fixed combination of saxagliptin and dapagliflozin. Importance of swallowing tablets of the fixed combination of saxagliptin and extended-release metformin whole and not cutting, crushing, or chewing them. Importance of advising patients receiving the fixed combination of saxagliptin and extended-release metformin that occasionally the inactive components of the tablet may remain intact and be passed in the stool as a soft, hydrated mass resembling the original tablet.
-
Importance of taking saxagliptin exactly as directed by clinician. Importance of informing patients that if they miss a dose of saxagliptin or the fixed combination of saxagliptin and dapagliflozin, they should take the dose as soon as it is remembered, unless it is almost time for the next dose. In that case, the missed dose should be skipped and the next dose taken at the regular time; patients should not take 2 doses at the same time unless instructed to do so by their clinician. Importance of informing patients that if they miss a dose of the fixed combination of saxagliptin and metformin hydrochloride, they should take the next dose as prescribed unless otherwise instructed by their clinician; patients should be instructed not to take an extra dose the next day.
-
Importance of women informing their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses (e.g., allergies, kidney disease).
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
2.5 mg (of saxagliptin) |
Onglyza |
AstraZeneca |
|
5 mg (of saxagliptin) |
Onglyza |
AstraZeneca |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, extended-release |
2.5 mg (of saxagliptin) with Metformin Hydrochloride extended-release 1 g |
Kombiglyze XR |
AstraZeneca |
|
2.5 mg (of saxagliptin) with Metformin Hydrochloride extended-release 1 g and Dapagliflozin Propanediol 2.5 mg (of dapagliflozin) |
Qternmet XR |
AstraZeneca |
||
|
2.5 mg (of saxagliptin) with Metformin Hydrochloride extended-release 1 g and Dapagliflozin Propanediol 5 mg (of dapagliflozin) |
Qternmet XR |
AstraZeneca |
||
|
5 mg (of saxagliptin) with Metformin Hydrochloride extended-release 500 mg |
Kombiglyze XR |
AstraZeneca |
||
|
5 mg (of saxagliptin) with Metformin Hydrochloride extended-release 1 g |
Kombiglyze XR |
AstraZeneca |
||
|
5 mg (of saxagliptin) with Metformin Hydrochloride extended-release 1 g and Dapagliflozin Propanediol 5 mg (of dapagliflozin) |
Qternmet XR |
AstraZeneca |
||
|
5 mg (of saxagliptin) with Metformin Hydrochloride extended-release 1 g and Dapagliflozin Propanediol 10 mg (of dapagliflozin) |
Qternmet XR |
AstraZeneca |
||
|
Tablets, film-coated |
5 mg (of saxagliptin) with Dapagliflozin Propranediol 5 mg (of dapagliflozin) |
Qtern |
AstraZeneca |
|
|
5 mg (of saxagliptin) with Dapagliflozin Propranediol 10 mg (of dapagliflozin) |
Qtern |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 21, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about saxagliptin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (17)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: dipeptidyl peptidase 4 inhibitors
- Breastfeeding
- En español