Pioglitazone (Monograph)
Brand names: Actos, ActoPlus Met (combination), Duetact (combination)
Drug class: Thiazolidinediones
Warning
- Heart Failure
-
Thiazolidinediones, including pioglitazone, cause or exacerbate heart failure in some patients. Monitor for signs and symptoms of heart failure (e.g., dyspnea, rapid and excessive weight gain, edema) after initiation of therapy and dosage titration. If heart failure develops, manage according to current standards of care; consider discontinuance or reduction in dosage of pioglitazone.
-
Not recommended in patients with symptomatic heart failure.
-
Initiation of pioglitazone contraindicated in patients with NYHA class III or IV heart failure.
Introduction
Antidiabetic agent; thiazolidinedione (glitazone).
Uses for Pioglitazone
Type 2 Diabetes Mellitus
Glycemic Control
Used as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
Used as monotherapy or in combination with other antidiabetic agents (e.g., metformin hydrochloride, sulfonylurea, insulin).
Commercially available as a single entity preparation and in fixed combination with metformin (Actoplus Met) or glimepiride (Duetact).
Guidelines from the American Diabetes Association (ADA) and other experts generally recommend thiazolidinediones as add-on therapy for select patients not at glycemic goal. When selecting treatment regimen, consider factors such as cardiovascular and renal comorbidities, drug efficacy and adverse effects, hypoglycemia risk, presence of overweight or obesity, cost, access, and patient preferences. Weight management should be included as a distinct treatment goal and other healthy lifestyle behaviors should also be considered.
Not used for the treatment of type 1 diabetes mellitus or diabetic ketoacidosis.
Reduction in Risk of Cardiovascular Events
Some data suggest possible protective effect of pioglitazone with regard to certain cardiovascular outcomes (e.g., death, MI, stroke) in patients with type 2 diabetes mellitus. While an increased risk of myocardial ischemic events has not been demonstrated to date, pioglitazone alone or in combination with other antidiabetic agents can cause fluid retention and other cardiovascular effects that may lead to or exacerbate heart failure. Therefore, potential risks and benefits of thiazolidinedione versus other second-line antidiabetic agents (e.g., sulfonylureas, insulin) should be carefully considered.
Pioglitazone Dosage and Administration
General
Pretreatment Screening
-
Obtain liver function tests (ALT, AST, alkaline phosphatase, total bilirubin) prior to initiation.
Patient Monitoring
-
Following initiation or dosage increases, patients should be carefully monitored for adverse effects related to fluid retention such as weight gain, edema, and congestive heart failure.
-
Fasting plasma glucose (FPG) concentrations should be monitored periodically to determine response. Periodic HbA1c determinations should also be performed; HbA1c is a better indicator of long-term glycemic control than FPG concentrations alone.
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) includes Actos (pioglitazone) and Actonel (risedronate) on the ISMP List of Confused Drug Names, and recommends special safeguards to ensure the accuracy of prescriptions for these drugs.
Administration
Oral Administration
Administer orally.
Commercially available as single-entity tablets and in fixed combination with glimepiride (Duetact) or immediate-release metformin hydrochloride (Actoplus Met).
Pioglitazone: Administer once daily without regard to meals.
Fixed combination of pioglitazone and metformin hydrochloride: Administer with meals to reduce the GI effects of metformin component.
Fixed combination of pioglitazone and glimepiride: Administer once daily with the first main meal.
If a dose of pioglitazone is missed on one day, the dose should not be doubled the following day.
Dosage
Available as pioglitazone hydrochloride; dosage expressed in terms of pioglitazone.
Adults
Type 2 Diabetes Mellitus
Pioglitazone
OralInitially, 15 or 30 mg once daily in patients without heart failure; use lower initial dosages in patients with NYHA class I or II heart failure.
If response inadequate, increase dosage in increments of 15 mg based on glycemic response as determined by HbA1c up to maximum of 45 mg daily.
Pioglitazone/Immediate-release Metformin Hydrochloride Fixed-combination Therapy
OralBase initial dosage of fixed combination on patient's existing dosage of pioglitazone and/or immediate-release metformin hydrochloride and available strengths of the fixed combination.
Patients not currently receiving either pioglitazone or metformin hydrochloride:Initially, pioglitazone 15 mg/metformin hydrochloride 850 mg once daily.
Patients receiving metformin hydrochloride monotherapy: Initially, pioglitazone 15 mg/metformin hydrochloride 850 mg once or twice daily depending on the patient's existing metformin dosage.
Patients receiving pioglitazone monotherapy: Initially, pioglitazone 15 mg/metformin hydrochloride 850 mg once daily.
Patients switching from combined therapy with separate pioglitazone and metformin preparations: Usual initial dosage of the fixed combination is the same as the patient's existing dosage of the individual drugs.
Gradually titrate dosage based on adequacy of therapeutic response and tolerability while not exceeding pioglitazone 45 mg and metformin hydrochloride 2.55 g per day. Total daily dosages of 2.55 g of metformin hydrochloride may be taken in divided doses 3 times daily to reduce adverse GI effects.
Pioglitazone/Glimepiride Fixed-combination Therapy
OralBase initial dosage of fixed combination on patient's existing dosage of pioglitazone and/or sulfonylurea (e.g., glimepiride).
Patients receiving glimepiride monotherapy: Initially, 30 mg of pioglitazone and 2 or 4 mg of glimepiride once daily.
Patients receiving pioglitazone monotherapy: Initially, 30 mg of pioglitazone and 2 mg of glimepiride once daily.
Patients switching from combined therapy with separate pioglitazone and glimepiride preparations: Usual initial dosage of the fixed combination is as close as possible to the patient's existing dosage of the individual drugs. Therapy may be initiated with 2 or 4 mg of glimepiride and 30 mg of pioglitazone once daily.
Patients switching from monotherapy with a sulfonylurea other than glimepiride (e.g., glyburide, glipizide) or from combined therapy with pioglitazone plus a sulfonylurea other than glimepiride: Initially, 30 mg of pioglitazone and 2 mg of glimepiride once daily. Observe patients for hypoglycemia for 1–2 weeks following transition from a sulfonylurea due to potential overlapping hypoglycemic effect.
Gradually titrate dosage based on adequacy of therapeutic response and tolerability while not exceeding pioglitazone 45 mg and glimepiride 8 mg per day.
Dosage Modifications for Drug Interactions
If hypoglycemia occurs during combination therapy with an insulin secretagogue (e.g., sulfonylurea), decrease dosage of the insulin secretagogue. If hypoglycemia occurs with concomitant pioglitazone and insulin therapy, reduce dosage of insulin by 10–25%; further adjustments to insulin dosage should be individualized according to glycemic response.
Initiation or discontinuance of a CYP2C8 inducer during pioglitazone therapy may necessitate changes in antidiabetic therapy; dosage of pioglitazone should not exceed 45 mg daily.
If a potent CYP2C8 inhibitor is used concomitantly, a maximum daily pioglitazone dosage of 15 mg is recommended.
Special Populations
Hepatic Impairment
Pioglitazone Monotherapy
No dosage adjustment necessary; initiate with caution in hepatic impairment.
Pioglitazone/Immediate-release Metformin Hydrochloride Fixed-combination Therapy
Not recommended in patients with hepatic impairment.
Pioglitazone/Glimepiride Fixed-combination Therapy
Use caution when initiating and increasing dosage; individuals with hepatic impairment may be particularly sensitive to hypoglycemic effects of glimepiride.
Renal Impairment
Pioglitazone Monotherapy
No dosage adjustment necessary.
Pioglitazone/Immediate-release Metformin Hydrochloride Fixed-combination Therapy
eGFR 30–45 mL/minute per 1.73 m2: Do not initiate; assess benefits and risks of continued treatment in patients already receiving pioglitazone in fixed combination with immediate-release metformin hydrochloride.
eGFR <30 mL/minute per 1.73 m2 : Use contraindicated; discontinue in patients already receiving pioglitazone in fixed combination with immediate-release metformin.
Pioglitazone/Glimepiride Fixed-combination Therapy
Use caution when initiating and increasing dosage; individuals with renal impairment may be particularly sensitive to the hypoglycemic effects of glimepiride.
Geriatric Patients
Pioglitazone Monotherapy
No dosage adjustment necessary.
Pioglitazone/Immediate-release Metformin Hydrochloride Fixed-combination Therapy
Conservative initial and maintenance dosages recommended, as aging is associated with reduced renal function.
Pioglitazone/Glimepiride Fixed-combination Therapy
Conservative initial and maintenance dosages recommended; geriatric individuals may be particularly sensitive to the hypoglycemic effects of glimepiride.
Patients with Heart Failure
NYHA class III or IV heart failure: Use contraindicated.
Pioglitazone Monotherapy
NYHA class I or II heart failure: Initially, 15 mg once daily. Increase dosage, if needed, up to maximum of 45 mg daily based on HbA1c concentrations. Monitor carefully for weight gain, edema, or other manifestations of heart failure exacerbation following initiation and dosage increase.
Pioglitazone/Immediate-release Metformin Hydrochloride Fixed-combination Therapy
NYHA class I or II heart failure: Initially, pioglitazone 15 mg/immediate-release metformin hydrochloride 500 mg or pioglitazone 15 mg/immediate-release metformin hydrochloride 850 mg once daily. Monitor carefully for weight gain, edema, or other manifestations of heart failure exacerbation following initiation and dosage increase.
Pioglitazone/Glimepiride Fixed-combination Therapy
Systolic dysfunction: Initially, pioglitazone 15 mg once daily as monotherapy; safely titrate dosage to 30 mg once daily as monotherapy before initiating the fixed combination of glimepiride 2 mg and pioglitazone 30 mg. If subsequent dosage adjustment is necessary with the fixed-combination preparation, monitor closely for weight gain, edema, or other manifestations of heart failure exacerbation.
Debilitated or Malnourished Patients
Pioglitazone/Glimepiride Fixed-combination Therapy
Use caution when initiating or increasing dosage; these individuals are particularly susceptible to hypoglycemic effects.
Patients with Adrenal or Pituitary Insufficiency
Pioglitazone/Glimepiride Fixed-combination Therapy
Use caution when initiating or increasing dosage; these individuals are particularly susceptible to hypoglycemic effects.
Cautions for Pioglitazone
Contraindications
-
Initiation of therapy in patients with established NYHA class III or IV heart failure.
-
Known serious hypersensitivity to pioglitazone or any ingredient in the formulation.
Warnings/Precautions
Warnings
Heart Failure
Dose-related fluid retention associated with use of pioglitazone, alone or in combination with other antidiabetic agents, may lead to or exacerbate heart failure (see Boxed Warning.). Fluid retention most common when used in combination with insulin. Heart failure reported during postmarketing experience in pioglitazone-treated patients who did or did not have previously known heart disease and who did or did not receive concomitant insulin therapy.
Monitor for signs and symptoms of heart failure (e.g., dyspnea, rapid weight gain, edema, unexplained cough, or fatigue), especially during initiation of therapy and dosage titration.
If heart failure develops, manage according to current standards of care. Consider dosage reduction or discontinuance of pioglitazone.
Other Warnings and Precautions
Hypoglycemia
Concomitant use of insulin or other antidiabetic drugs (e.g., insulin secretagogues) increases risk for hypoglycemia. May need to reduce dosage of concomitant antidiabetic agent to decrease risk of hypoglycemia.
Hepatic Effects
No evidence of drug-induced hepatotoxicity in controlled clinical trial database to date. However, hepatic failure with or without fatalities reported during postmarketing experience.
Obtain liver function tests (serum ALT and AST, alkaline phosphatase, total bilirubin) and assess patient prior to initiation of therapy; if tests abnormal, initiate pioglitazone with caution.
Recheck liver function promptly if manifestations suggestive of hepatic dysfunction (e.g., right upper abdominal discomfort, fatigue, anorexia, dark urine, jaundice) occur. Interrupt therapy if ALT is >3 times the upper limit of normal (ULN) in patients with symptoms of liver injury; do not restart drug in patients without another explanation for liver test abnormalities. Patients with serum ALT >3 times the reference range and serum total bilirubin >2 times the reference range without alternative etiologies are at risk for severe drug-induced liver injury; do not restart drug in such patients. May use pioglitazone with caution in patients with lesser elevations of serum ALT or bilirubin who have an alternative probable cause for such elevations.
Urinary Bladder Tumors
May be associated with increased risk of bladder cancer.
Do not use in patients with active bladder cancer; use with caution in patients with history of bladder cancer, weighing benefits of glycemic control against unknown risks of cancer recurrence.
Edema
Fluid retention reported; may lead to or exacerbate heart failure. Pioglitazone-induced edema reversible upon discontinuation of drug.
Use with caution in patients with edema and in those at risk for heart failure. Observe for manifestations of heart failure (e.g., dyspnea, rapid weight gain, edema).
Advise patients to monitor for weight gain and edema.
Fractures
Risk of bone loss and fractures in women, and possibly in men, receiving thiazolidinedione therapy.
Fractures reported more frequently in women receiving pioglitazone (5.1%) than in women receiving placebo (2.5%) in long-term study (mean 34.5 months follow-up). Effects noted after first year of treatment and persisted throughout treatment. Most fractures were nonvertebral, occurring in a distal limb (forearm, hand, wrist, foot, ankle, fibula, tibia).
In an observational study, use of pioglitazone or rosiglitazone for approximately 12–18 months associated with 2- to 3-fold increase in fractures, particularly of hip and wrist. Overall risk of fracture similar among men and women.
Consider risk of fracture, particularly in female patients. Assess and maintain bone health according to current standards of care.
Macular Edema
New-onset or worsening macular edema with decreased visual acuity reported rarely; most patients had concurrent peripheral edema. Symptoms improved in some patients following discontinuance of pioglitazone.
Regular eye examinations by ophthalmologist advised. Promptly refer patients reporting visual symptoms to ophthalmologist, regardless of other concurrent therapy or physical findings.
Macrovascular Outcomes
Evidence of macrovascular risk reduction with pioglitazone has not been conclusively demonstrated in controlled clinical trials.
Use of Fixed Combinations
When used in fixed combination with metformin hydrochloride or glimepiride, consider the cautions, precautions, and contraindications associated with the concomitant agent.
Specific Populations
Pregnancy
Insufficient evidence on use of pioglitazone in pregnant women to evaluate drug-associated risk for major birth defects or miscarriage. No adverse developmental effects observed in animal reproduction studies; however, delayed postnatal development (attributed to decreased body weight), delayed parturition, and reduced embryofetal viability were observed.
Poorly controlled diabetes mellitus during pregnancy carries risks to mother and fetus.
Lactation
No data on presence of pioglitazone in human milk, the effects on the breast-fed infant, or effects on milk production. Distributed into milk in rats. Weigh benefits of breast-feeding against potential risk of adverse effects on the breast-fed infant from pioglitazone.
Females and Males of Reproductive Potential
Discuss potential for unintended pregnancy with premenopausal women as therapy with pioglitazone may result in ovulation in some ambulatory women.
Pediatric Use
Safety and efficacy not established; use not recommended.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults.
Hepatic Impairment
Initiate with caution in patients with abnormal liver function test results. Interrupt pioglitazone therapy if ALT >3 times the ULN and investigate the cause of liver test abnormalities.
Common Adverse Effects
Most common adverse effects (≥5%): Upper respiratory tract infection, headache, sinusitis, myalgia, pharyngitis.
Drug Interactions
Metabolized principally by CYP2C8 and, to a lesser extent, by CYP3A4 and other isoenzymes (e.g., CYP1A1).
Weak inducer of CYP3A4.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Strong CYP2C8 inhibitors: Increase pioglitazone AUC and half-life; do not exceed maximum pioglitazone dosage of 15 mg once daily.
CYP2C8 inducers: Decreased pioglitazone AUC. Initiation or discontinuance of a CYP2C8 inducer during pioglitazone therapy may necessitate changes in antidiabetic therapy; however, do not exceed maximum recommended pioglitazone dosage of 45 mg daily.
CYP3A4 substrates: Potential pharmacokinetic interaction (reduction in peak plasma concentration and AUC of the CYP3A4 substrate).
CYP2C9 substrates: Pharmacokinetic interactions unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antidiabetic agents |
Additive effects; possible hypoglycemia |
May need to reduce dosage of other antidiabetic agents |
|
Atorvastatin |
Decreased plasma concentrations and AUC for atorvastatin and pioglitazone |
Clinical importance unknown |
|
Digoxin |
Pharmacokinetic interaction unlikely |
|
|
Fexofenadine |
Pharmacokinetic interaction unlikely |
|
|
Gemfibrozil |
Increased pioglitazone AUC and half-life |
Do not exceed maximum pioglitazone dosage of 15 mg once daily |
|
Ketoconazole |
Increased serum concentrations and AUC for pioglitazone |
|
|
Midazolam |
Decreased midazolam AUC and peak plasma concentrations |
Clinical importance unknown |
|
Nifedipine, extended-release |
Decreased peak plasma nifedipine concentrations and AUC |
Clinical importance unknown |
|
Oral contraceptives, hormonal (ethinyl estradiol/norethindrone) |
Small decreases in peak plasma ethinyl estradiol concentrations and AUC |
Clinical importance unknown |
|
Ranitidine |
Pharmacokinetic interaction unlikely |
|
|
Rifampin |
Decreased pioglitazone AUC |
May require change in antidiabetic therapy if rifampin initiated or discontinued during pioglitazone therapy, but do not exceed maximum pioglitazone dosage of 45 mg daily |
|
Theophylline |
Pharmacokinetic interaction unlikely |
|
|
Topiramate |
Reductions in AUC of pioglitazone and active metabolites with concomitant administration |
Clinical relevance unknown; however, manufacturer recommends monitoring for adequate glycemic control when concomitant therapy used |
|
Warfarin |
Pharmacokinetic or pharmacologic interaction (e.g., effect on PT) unlikely |
Pioglitazone Pharmacokinetics
Absorption
Bioavailability
Peak serum concentrations attained within 2 hours.
Bioequivalence demonstrated between fixed combination products and each agent given concurrently as separate tablets.
Food
Food delays time to peak serum concentration to 3–4 hours but does not affect extent of absorption.
Special Populations
In patients with hepatic impairment (Child-Pugh class B or C), peak pioglitazone concentration is decreased by 45%.
In geriatric patients, AUC of pioglitazone is increased; not clinically relevant.
In females, peak serum concentration and AUC are increased by 20–60%.
Distribution
Extent
Distributed into milk in rats. Not known whether the drug distributes into human milk.
Plasma Protein Binding
>99% (mainly albumin).
Elimination
Metabolism
Extensively metabolized via hydroxylation and oxidation, principally by CYP2C8 and, to a lesser extent, by CYP3A4 and other isoenzymes (e.g., CYP1A1). Major circulating active metabolites are M-III (keto derivative) and M-IV (hydroxyl derivative).
Elimination Route
Excreted in urine (15–30%) and feces, primarily as metabolites.
Half-life
3–7 hours (for pioglitazone) or 16–24 hours (for pioglitazone and metabolites).
Special Populations
In geriatric patients, terminal half-life is prolonged; not clinically relevant.
Elimination half-life unchanged in moderate (Clcr 30—50 mL/minute) and severe (Clcr <30 mL/minute) renal impairment.
Stability
Storage
Oral
Tablets
Tight containers at 25°C (may be exposed to 15–30°C). Protect from light, moisture, and humidity.
Actions
-
Structurally and pharmacologically related to rosiglitazone and troglitazone (no longer commercially available in the US); unrelated to other antidiabetic agents (e.g., sulfonylureas, biguanides, α-glucosidase inhibitors).
-
A peroxisome proliferator-activated receptorγ (PPARγ) agonist; increases transcription of insulin-responsive genes.
-
Increases insulin sensitivity in target tissues and decreases hepatic gluconeogenesis. Ameliorates insulin resistance associated with type 2 diabetes mellitus without increasing insulin secretion from pancreatic β cells. Does not lower glucose concentrations below euglycemia.
-
Ineffective in absence of insulin.
Advice to Patients
-
Advise patients to read the FDA-approved patient labeling (Medication Guide) provided by manufacturer before starting pioglitazone and each time prescription is refilled.
-
Inform patients of potential risks and advantages of therapy and of alternative therapies.
-
Inform patients of the importance of diet and exercise regimen adherence. Inform patients of the importance of regular monitoring (preferably self-monitoring) of blood glucose and of HbA1c.
-
Inform patients of the potential need for alterations in dosage requirements during periods of stress (e.g., fever, trauma, infection, surgery).
-
Inform patients who experience an unusually rapid increase in weight or edema or who develop shortness of breath or other symptoms of heart failure while on pioglitazone to immediately report these symptoms to their clinician.
-
Inform patients to promptly stop taking pioglitazone and seek immediate medical advice if there is unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, or dark urine as these symptoms may be due to hepatotoxicity.
-
Advise patients to promptly report any sign of macroscopic hematuria or other symptoms such as dysuria or urinary urgency that develop or increase during pioglitazone treatment as these may be due to bladder cancer.
-
Inform patients of the risk of hypoglycemia when pioglitazone is used in combination with insulin or other antidiabetic medications, the symptoms of hypoglycemia and its treatment, and conditions that predispose to its development. Provide instructions to patients and responsible family members regarding management of hypoglycemia, including recognition of symptoms, predisposing conditions, and treatment.
-
Inform female patients that treatment with pioglitazone may result in unintended pregnancy in some premenopausal anovulatory women due to its effect on ovulation.
-
Inform patients of the risk of fractures (e.g., hand, upper arm, foot), particularly in women.
-
Inform patients of the importance of regular eye examinations. Advise patients of the importance of reporting changes in vision to their clinician.
-
Advise patients to inform their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Advise patients to inform clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
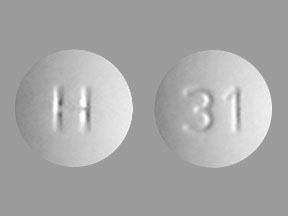
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
15 mg (of pioglitazone)* |
Actos |
Takeda |
|
Pioglitazone Hydrochloride |
||||
|
30 mg (of pioglitazone)* |
Actos |
Takeda |
||
|
Pioglitazone Hydrochloride |
||||
|
45 mg (of pioglitazone)* |
Actos |
Takeda |
||
|
Pioglitazone Hydrochloride |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
15 mg (of pioglitazone) with Metformin Hydrochloride 500 mg* |
Pioglitazone Hydrochloride with Metformin Hydrochloride |
|
|
15 mg (of pioglitazone) with Metformin Hydrochloride 850 mg* |
Actoplus Met |
Takeda |
||
|
Pioglitazone Hydrochloride with Metformin Hydrochloride |
||||
|
30 mg (of pioglitazone) with Glimepiride 2 mg* |
Duetact |
Takeda |
||
|
Pioglitazone Hydrochloride with Glimepiride |
||||
|
30 mg (of pioglitazone) with Glimepiride 4 mg* |
Duetact |
Takeda |
||
|
Pioglitazone Hydrochloride with Glimepiride |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about pioglitazone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (54)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: thiazolidinediones
- Breastfeeding
- En español