HYDROcodone (Analgesic) (Monograph)
Drug class: Opioid Agonists
VA class: CN101
CAS number: 34195-34-1
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for hydrocodone to ensure that the benefits outweigh the risks. The REMS may apply to one or more preparations of hydrocodone and consists of the following: medication guide and elements to assure safe use. See https://www.accessdata.fda.gov/scripts/cder/rems/.
-
FDA drug safety communication (4/13/2023): As part of its ongoing efforts to address the nation’s opioid crisis, FDA is requiring several updates to the prescribing information of opioid pain medicines. The changes are being made to provide additional guidance for safe use of these drugs while also recognizing the important benefits when used appropriately. The changes apply to both immediate-release (IR) and extended-release/long-acting preparations (ER/LA).
-
Updates to the IR opioids state that these drugs should not be used for an extended period unless the pain remains severe enough to require an opioid pain medicine and alternative treatment options are insufficient, and that many acute pain conditions treated in the outpatient setting require no more than a few days of an opioid pain medicine.
-
Updates to the ER/LA opioids recommend that these drugs be reserved for severe and persistent pain requiring an extended period of treatment with a daily opioid pain medicine and for which alternative treatment options are inadequate.
-
A new warning is being added about opioid-induced hyperalgesia (OIH) for both IR and ER/LA opioid pain medicines. This includes information describing the symptoms that differentiate OIH from opioid tolerance and withdrawal.
-
Information in the boxed warning for all IR and ER/LA opioid pain medicines will be updated and reordered to elevate the importance of warnings concerning life-threatening respiratory depression, and risks associated with using opioid pain medicines in conjunction with benzodiazepines or other medicines that depress the central nervous system (CNS).
-
Other changes will also be required in various other sections of the prescribing information to educate clinicians, patients, and caregivers about the risks of these drugs.
Introduction
Hydrocodone bitartrate is a phenanthrene-derivative opiate agonist that is used as an analgesic and antitussive agent.
Uses for HYDROcodone (Analgesic)
Extended-release hydrocodone bitartrate is used for the relief of pain that is severe enough to require long-term, daily, around-the-clock use of an opiate analgesic. Because of the risks of addiction, abuse, and misuse associated with opiates, even at recommended dosages, and because of the greater risks of overdose and death associated with extended-release opiate formulations, extended-release hydrocodone bitartrate should be reserved for use in patients for whom alternative treatment options (e.g., nonopiate analgesics or immediate-release opiates) are inadequate or not tolerated. Extended-release hydrocodone bitartrate is not indicated for use on an as-needed (“prn”) basis.
Efficacy of hydrocodone bitartrate extended-release capsules (Zohydro ER) was established in patients with moderate to severe chronic low back pain requiring chronic opiate therapy; the currently prescribed opiate was switched to the extended-release hydrocodone bitartrate capsules and the dosage was titrated to a stable level (up to 100 mg twice daily) during an initial open-label phase of the study; over a subsequent 12-week, randomized, placebo-controlled withdrawal phase, hydrocodone was associated with reductions in pain intensity compared with placebo.
Efficacy of extended-release tablets of hydrocodone bitartrate (Hysingla ER) also was established in patients with moderate to severe chronic low back pain. The currently prescribed opiate and/or nonopiate analgesic(s) were switched to extended-release hydrocodone bitartrate tablets and the dosage was titrated to a stable level (20–120 mg once daily) during an initial open-label phase of the study; over a subsequent 12-week, randomized, placebo-controlled withdrawal phase, hydrocodone provided greater analgesia compared with placebo.
Hydrocodone bitartrate in fixed combination with acetaminophen is used for the relief of moderate to moderately severe pain.
Hydrocodone bitartrate in fixed combination with ibuprofen is used short term (generally for less than 10 days) for the relief of acute pain. Efficacy was established in single-dose studies in patients with postoperative (abdominal, gynecologic, orthopedic) pain. Hydrocodone bitartrate in fixed combination with ibuprofen is not indicated for the management of pain associated with such chronic conditions as osteoarthritis or rheumatoid arthritis.
For further information on the role of opiate analgesics in the management of acute or chronic pain, see Uses: Pain, in the Opiate Agonists General Statement 28:08.08.
For use of hydrocodone as an antitussive agent, see 48:08.
HYDROcodone (Analgesic) Dosage and Administration
Administration
Hydrocodone bitartrate is administered orally. Patients receiving hydrocodone should avoid alcohol; concomitant use may result in profound sedation, respiratory depression, coma, or death.
Hydrocodone bitartrate extended-release capsules are administered twice daily (every 12 hours). The extended-release capsules must be taken whole; crushing, breaking, cutting, chewing, or dissolving the capsules will result in uncontrolled delivery of hydrocodone and can result in overdosage and death. Patients should be advised that they must not consume alcoholic beverages or take prescription or nonprescription preparations containing alcohol during therapy, since concomitant ingestion of alcohol with hydrocodone bitartrate extended-release capsules may result in increased plasma concentrations of the drug and a potentially fatal overdose. (See Drug Interactions: Alcohol.)
Hydrocodone bitartrate extended-release tablets are administered once daily (every 24 hours) without regard to meals. Multiple tablets of lower-dose strengths that provide the desired total daily dosage can be taken as a once-daily dose. If a dose is missed, the next dose should be taken at the scheduled time on the following day. The extended-release tablets must be taken whole, one tablet at a time, with enough water to ensure complete swallowing of the tablet immediately after it is placed in the mouth. The tablets should not be wet (e.g., soaked, licked) before they are placed in the mouth for swallowing, since wetting the tablets results in formation of a gelatinous mass that may be difficult to swallow. (See Cautions.) Crushing, chewing, or dissolving the tablets will result in uncontrolled delivery of hydrocodone and can result in overdosage and death.
Dosage
Hydrocodone bitartrate should be given at the lowest effective dosage and for the shortest duration of therapy consistent with the treatment goals of the patient. Reduced dosage is indicated in poor-risk and geriatric patients. If concomitant therapy with other CNS depressants is required, the lowest effective dosages and shortest possible duration of concomitant therapy should be used.
For acute pain not related to trauma or surgery, the prescribed quantity should be limited to the amount needed for the expected duration of pain severe enough to require opiate analgesia (generally 3 days or less and rarely more than 7 days). When opiate analgesics are used for the management of chronic noncancer pain, the US Centers for Disease Control and Prevention (CDC) recommends that primary care clinicians carefully reassess individual benefits and risks before prescribing dosages equivalent to 50 mg or more of morphine sulfate daily (approximately 50 mg or more of hydrocodone bitartrate daily) and avoid dosages equivalent to 90 mg or more of morphine sulfate daily (approximately 90 mg or more of hydrocodone bitartrate daily) or carefully justify their decision to titrate the dosage to such levels. Other experts recommend consulting a pain management specialist before exceeding a dosage equivalent to 80–120 mg of morphine sulfate daily. For further information on the management of opiate analgesic therapy, see Dosage and Administration: Dosage, in the Opiate Agonists General Statement 28:08.08.
Extended-release Capsules
To reduce the risk of respiratory depression in patients receiving hydrocodone bitartrate extended-release capsules, appropriate dosage selection and titration are essential. The initial dosage must be individualized, taking into account the patient's prior analgesic use and risk factors for addiction, abuse, and misuse. Patients should be monitored closely for respiratory depression, especially during the first 24–72 hours of therapy and following any increase in dosage.
For the management of severe pain requiring long-term, around-the-clock analgesia in adults who are not opiate tolerant or not currently receiving opiate analgesics, therapy with extended-release hydrocodone bitartrate capsules (Zohydro ER) should be initiated at a dosage of 10 mg every 12 hours. Use of higher initial dosages in patients who are not opiate tolerant may result in fatal respiratory depression. A single dose exceeding 40 mg, the 50-mg extended-release hydrocodone bitartrate capsules, or a total daily dosage exceeding 80 mg should be used only in patients in whom tolerance to an opiate of comparable potency has been established. Patients are considered opiate tolerant if they have been receiving at least 60 mg of oral morphine sulfate daily, 25 mcg of transdermal fentanyl per hour, 30 mg of oral oxycodone hydrochloride daily, 8 mg of oral hydromorphone hydrochloride daily, 25 mg of oral oxymorphone hydrochloride daily, or an equianalgesic dose of another opiate daily for at least 1 week.
In adults who are being transferred from other oral opiates to therapy with extended-release hydrocodone bitartrate capsules, all other around-the-clock opiate analgesics should be discontinued when therapy with the extended-release capsules is initiated. Dosage must be carefully individualized since overestimation of the initial dosage in opiate-tolerant patients can result in fatal overdosage. The manufacturer states that the conversion factors in Table 1 may be used as a guide for selecting an initial dosage of extended-release hydrocodone bitartrate capsules for patients being transferred from therapy with one of the oral opiates listed in the table. The manufacturer cautions that the doses in Table 1 are not equianalgesic doses and the table cannot be used to transfer patients from extended-release hydrocodone bitartrate capsules to another opiate, as this will result in overestimation of the dosage of the new opiate and possible fatal overdosage. For patients receiving a single opiate analgesic, the current total daily dosage of the opiate should be multiplied by the appropriate conversion factor in Table 1 to calculate the approximate daily dosage of extended-release hydrocodone bitartrate capsules; the calculated daily dosage should then be divided in half for administration every 12 hours. For patients receiving more than one opiate analgesic, the approximate daily dosage of extended-release hydrocodone bitartrate should be calculated for each opiate and then those totals should be summed to obtain the approximate total daily dosage of extended-release hydrocodone bitartrate capsules; the calculated total daily dosage should then be divided in half for administration every 12 hours. For patients receiving analgesics containing opiates and nonopiates in a fixed ratio, only the opiate component should be considered in the conversion. Calculated doses that do not correspond to an available capsule strength should always be rounded down to the nearest whole capsule.
|
Prior Oral Opiate |
Oral Dose (mg) |
Approximate Oral Conversion Factor |
|---|---|---|
|
Hydrocodone |
10 |
1 |
|
Oxycodone |
10 |
1 |
|
Methadone |
10 |
1 |
|
Oxymorphone |
5 |
2 |
|
Hydromorphone |
3.75 |
2.67 |
|
Morphine |
15 |
0.67 |
|
Codeine |
100 |
0.1 |
Following transfer from other opiate analgesics to extended-release hydrocodone bitartrate, patients should be monitored for manifestations of opiate withdrawal and for oversedation or toxicity. Particularly close monitoring is required when patients are switched from methadone, since conversion ratios between methadone and other opiates vary widely depending on extent of prior methadone exposure and because methadone has a long half-life and tends to accumulate in plasma.
In adults who are being transferred from transdermal fentanyl to extended-release hydrocodone bitartrate capsules, therapy with the extended-release capsules can be initiated 18 hours following removal of the transdermal fentanyl system at a conservative hydrocodone bitartrate dosage of approximately 10 mg every 12 hours for each 25 mcg/hour of transdermal fentanyl. Patients should be monitored closely, as there is limited experience with this conversion.
Dosage of extended-release hydrocodone bitartrate capsules should be adjusted gradually, every 3–7 days in increments of 10 mg every 12 hours, to provide adequate analgesia and to minimize adverse effects. If discontinuance of therapy is required, gradual tapering of the dosage every 2–4 days is recommended to avoid manifestations associated with abrupt withdrawal. Patients should be monitored closely for manifestations of withdrawal, which may indicate the need for slower tapering. In a phase 3 clinical trial, dosage of extended-release hydrocodone bitartrate capsules in patients reassigned to receive placebo was tapered according to the schedule in Table 2; dosages exceeding 100 mg twice daily were not evaluated in the clinical trial.
|
Stable Dosage at Time of Taper Initiation |
Taper Schedule |
|---|---|
|
20–30 mg every 12 hours |
10 mg every 12 hours for 2 days, then discontinue on day 3 |
|
40–70 mg every 12 hours |
40 mg every 12 hours for 2 days, 20 mg every 12 hours for 2 days, 10 mg every 12 hours for 2 days, then discontinue on day 7 |
|
80–100 mg every 12 hours |
80 mg every 12 hours for 2 days, 60 mg every 12 hours for 2 days, 40 mg every 12 hours for 2 days, 20 mg every 12 hours for 2 days, 10 mg every 12 hours for 2 days, then discontinue on day 11 |
Extended-release Tablets
To reduce the risk of respiratory depression in patients receiving hydrocodone bitartrate extended-release tablets, appropriate dosage selection and titration are essential. The initial dosage must be individualized, taking into account the patient's prior analgesic use and risk factors for addiction, abuse, and misuse. Patients should be monitored closely for respiratory depression, especially during the first 24–72 hours of therapy and following any increase in dosage.
For the management of severe pain requiring long-term, around-the-clock analgesia in adults who are not opiate tolerant or not currently receiving opiate analgesics, therapy with extended-release hydrocodone bitartrate tablets (Hysingla ER) should be initiated at a dosage of 20 mg every 24 hours. Use of higher initial dosages in patients who are not opiate tolerant may result in fatal respiratory depression. Dosages of 80 mg or more daily should be used only in opiate-tolerant patients. Patients are considered opiate tolerant if they have been receiving at least 60 mg of oral morphine sulfate daily, 25 mcg of transdermal fentanyl per hour, 30 mg of oral oxycodone hydrochloride daily, 8 mg of oral hydromorphone hydrochloride daily, 25 mg of oral oxymorphone hydrochloride daily, or an equianalgesic dose of another opiate daily for at least 1 week.
Patients being transferred from other oral hydrocodone-containing formulations to the extended-release tablets should receive the same total daily dosage of hydrocodone bitartrate administered once daily.
In adults who are being transferred from other oral opiates to therapy with extended-release hydrocodone bitartrate tablets, all other around-the-clock opiate analgesics should be discontinued when therapy with the extended-release tablets is initiated. Dosage must be carefully individualized since overestimation of the initial dosage in opiate-tolerant patients can result in fatal overdosage. The conversion factors in Table 3 may be used as a guide for selecting an initial dosage of extended-release hydrocodone bitartrate tablets for patients being transferred from therapy with one of the oral opiates listed in the table. The manufacturer cautions that the doses in Table 3 are not equianalgesic doses and the table cannot be used to transfer patients from extended-release hydrocodone bitartrate tablets to another opiate, as this will result in overestimation of the dosage of the new opiate and possible fatal overdosage. For patients receiving a single opiate analgesic, the current total daily dosage of the opiate should be multiplied by the appropriate conversion factor in Table 3 to calculate the approximate daily dosage of oral hydrocodone bitartrate; for patients receiving more than one opiate analgesic, the approximate daily dosage of oral hydrocodone bitartrate should be calculated for each opiate and then those totals should be summed to obtain the approximate daily dosage of oral hydrocodone bitartrate. Initial oral hydrocodone bitartrate dosages calculated using the conversion factors in Table 3 should be reduced by 25% to account for interpatient variability in the relative potency of different opiates. For patients receiving analgesics containing opiates and nonopiates in a fixed ratio, only the opiate component should be considered in the conversion. Calculated doses that do not correspond to an available tablet strength should always be rounded down to the nearest whole tablet. If the calculated dose is less than 20 mg, therapy should be initiated at a dosage of 20 mg once daily.
|
Prior Oral Opiate |
Oral Dose (mg) |
Approximate Oral Conversion Factor |
|---|---|---|
|
Codeine |
133 |
0.15 |
|
Hydromorphone |
5 |
4 |
|
Methadone |
13.3 |
1.5 |
|
Morphine |
40 |
0.5 |
|
Oxycodone |
20 |
1 |
|
Oxymorphone |
10 |
2 |
|
Tramadol |
200 |
0.1 |
Following transfer from other opiate analgesics to extended-release hydrocodone bitartrate, patients should be monitored for manifestations of opiate withdrawal and for oversedation or toxicity. Particularly close monitoring is required when patients are switched from methadone, since conversion ratios between methadone and other opiates vary widely depending on extent of prior methadone exposure and because methadone has a long half-life and tends to accumulate in plasma.
In adults who are being transferred from transdermal fentanyl to extended-release hydrocodone bitartrate tablets, therapy with the extended-release tablets can be initiated 18 hours following removal of the transdermal fentanyl system at a conservative hydrocodone bitartrate dosage of approximately 20 mg every 24 hours for each 25 mcg/hour of transdermal fentanyl. Patients should be monitored closely, as there is limited experience with this conversion.
Adults receiving transdermal buprenorphine at a dosage of 20 mg or less per hour should be switched to extended-release hydrocodone bitartrate tablets at a dosage of 20 mg every 24 hours. Patients should be monitored closely, as there is limited experience with this conversion.
Dosage of extended-release hydrocodone bitartrate tablets should be adjusted gradually, every 3–5 days in increments of 10–20 mg every 24 hours, to provide adequate analgesia and to minimize adverse effects. If discontinuance of therapy is required, gradual tapering of the dosage every 2–4 days is recommended to avoid manifestations associated with abrupt withdrawal. As the dosage is tapered, each new dose should be at least 50% of the prior dose; once the dosage has been reduced to 20 mg daily for 2–4 days, therapy can be discontinued.
Immediate-release Fixed-combination Preparations
The usual adult dosage of hydrocodone bitartrate when used in fixed combination with acetaminophen for relief of moderate to moderately severe pain is 5–10 mg every 4–6 hours as necessary. When used in fixed combination with ibuprofen for relief of acute pain, the usual adult dosage of hydrocodone bitartrate is 2.5–10 mg every 4–6 hours as needed, generally given for no longer than 10 days; the manufacturers state that the total daily dosage should not exceed 5 tablets (each providing from 2.5–10 mg of hydrocodone bitartrate and 200 mg of ibuprofen). Dosage should be adjusted according to the severity of the pain and the response and tolerance of the patient. When opiate analgesics are administered in fixed combination with nonopiate analgesics, the opiate dosage may be limited by the nonopiate component. Because commercially available preparations contain hydrocodone bitartrate and nonopiate analgesics in various fixed ratios and because these nonopiate analgesics also are available in many other prescription and OTC preparations, care should be taken to ensure that therapy is not duplicated and that dosage of the nonopiate drug does not exceed maximum recommended dosages.
Dosage in Renal and Hepatic Impairment
No adjustment of initial hydrocodone bitartrate dosage is required in patients with mild or moderate hepatic impairment. Because of the potential for increased drug exposure, the manufacturer states that therapy with hydrocodone bitartrate extended-release capsules should be initiated at a dosage of 10 mg every 12 hours in patients with severe hepatic impairment. The manufacturer of hydrocodone bitartrate extended-release tablets states that dosage of this formulation should be reduced by 50% in patients with severe hepatic impairment. Patients with severe hepatic impairment should be monitored closely for adverse effects (e.g., respiratory depression, sedation).
Because of the potential for increased drug exposure, the manufacturer states that therapy with hydrocodone bitartrate extended-release capsules should be initiated at a low dose in patients with renal impairment. The manufacturer of hydrocodone bitartrate extended-release tablets states that dosage of this formulation should be reduced by 50% in patients with moderate or severe renal impairment (including end-stage renal disease); the manufacturer states that the extended-release tablets may be used without dosage adjustment in patients with mild renal impairment. Patients with renal impairment should be monitored closely for adverse effects (e.g., respiratory depression, sedation).
Cautions for HYDROcodone (Analgesic)
Hydrocodone bitartrate shares the toxic potentials of the opiate agonists, and the usual precautions of opiate agonist therapy should be observed. (See Cautions in the Opiate Agonists General Statement 28:08.08.) For further information on cautions, precautions, and contraindications associated with the use of hydrocodone, see also Cautions in Hydrocodone Bitartrate 48:08. When hydrocodone is used as a fixed-combination preparation that includes acetaminophen or ibuprofen, the cautions, precautions, and contraindications associated with these drugs must be considered in addition to those associated with hydrocodone.
Because some patients have reported difficulty in swallowing hydrocodone bitartrate extended-release tablets, the tablets should be administered one at a time with enough water to ensure that each tablet is completely swallowed immediately after it is placed in the mouth; the extended-release tablets should not be wet (e.g., soaked, licked) before they are placed in the mouth for swallowing. Choking, dysphagia, and esophageal obstruction (in at least one case requiring medical intervention to remove the tablet) have been reported. Patients with underlying GI disorders (e.g., esophageal or colon cancer) associated with a narrow GI lumen are at greater risk of developing these complications. Use of an alternative analgesic should be considered for patients who have difficulty swallowing and in those at risk for underlying GI disorders associated with a narrow GI lumen. Because the extended-release tablets gradually form a gelatinous mass when exposed to fluids, pediatric patients may be at increased risk of esophageal obstruction, dysphagia, and choking because of their smaller GI lumen if they ingest the tablets.
Prolongation of the corrected QT (QTc) interval was observed in healthy individuals receiving hydrocodone bitartrate 160 mg daily (as extended-release tablets). This observation should be considered when making decisions regarding patient monitoring (e.g., periodic monitoring of ECGs and electrolyte concentrations) when hydrocodone bitartrate extended-release tablets are used in patients with congestive heart failure, bradyarrhythmias, or electrolyte abnormalities or in those who are receiving drugs that are known to prolong the QTc interval. The manufacturer states that use of the extended-release tablets should be avoided in patients with congenital long QT syndrome. If prolongation of the QTc interval occurs, reduction of hydrocodone bitartrate dosage by 33–50% or use of an alternative analgesic should be considered.
Misuse and Abuse
Because of the challenges associated with providing access to an adequate array of options for management of chronic pain while simultaneously preventing prescription opiate abuse and misuse, the decision by the US Food and Drug Administration (FDA) to approve hydrocodone bitartrate extended-release capsules (Zohydro ER) was controversial, as the formulation lacks tamper-resistant features that might deter abuse and, like other extended-release opiates, some strengths contain substantial amounts of the drug (up to 50 mg ). Hydrocodone bitartrate extended-release tablets (Hysingla ER; containing up to 120 mg of the drug) are formulated with physical and chemical properties that are intended to make this dosage form more difficult to manipulate for IV or intranasal abuse and misuse, and some extended-release characteristics are retained if the tablets are physically compromised. In vitro studies indicate that exposing the tablets to water results in formation of a viscous hydrogel that resists passage through a needle; the tablets also are resistant to crushing, breaking, and dissolution by various tools and solvents. Results of clinical abuse potential studies suggest a reduced potential for intranasal abuse (compared with powdered hydrocodone bitartrate) or oral abuse by chewing the tablets (compared with hydrocodone bitartrate solution). However, the potential for IV, intranasal, and oral abuse still exists.
Modified-release (e.g., extended-release) opiates are associated with a greater risk of overdose and death because of the larger amount of drug contained in each dosage unit. Abuse or misuse of hydrocodone bitartrate extended-release dosage forms by cutting, breaking, crushing, chewing, or dissolving the capsules or tablets, snorting the contents, or injecting the dissolved contents will result in uncontrolled delivery of the drug and can result in overdosage and death. Inadvertent ingestion of even one dose of extended-release hydrocodone bitartrate capsules or tablets, especially by a child, also can result in a fatal overdose. Intake of alcohol with the extended-release capsules may result in increased peak plasma concentrations of hydrocodone and ingestion of a potentially toxic dose of the drug. (See Drug Interactions: Alcohol.) Extended-release preparations of hydrocodone bitartrate should be prescribed only by clinicians who are knowledgeable in the use of potent opiates for the management of chronic pain.
Hydrocodone in fixed combination with other analgesics (e.g., acetaminophen, nonsteroidal anti-inflammatory agents) is used widely in the management of pain. Hydrocodone also is used in antitussive preparations for the management of cough. Depending on the formulation, many of these fixed-combination analgesic and antitussive preparations previously were subject to control under the Federal Controlled Substances Act of 1970 as schedule III (C-III) drugs. However, because of increasing concerns about misuse, abuse, and diversion of these preparations, the US Department of Health and Human Services (HHS) recommended on December 16, 2013, that these preparations be rescheduled to schedule II (C-II) in response to an evidence-based analysis by FDA. This recommendation subsequently was accepted by the US Drug Enforcement Administration (DEA) and became effective October 6, 2014. Preparations containing hydrocodone in fixed combination with other analgesics have a clinically important and legitimate role in the management of moderate to moderately severe pain. Hydrocodone-containing combination preparations also have a clinically important and legitimate role in the symptomatic treatment of cough and upper respiratory symptoms associated with allergy and cold when they combine hydrocodone with other antitussives or antihistamines.
The conclusions of FDA and DEA considered a number of factors such as abuse potential, pharmacologic effects, history and current patterns of abuse, public health risk, dependence liability, and scope, duration, and significance of abuse. In recent years, hydrocodone-containing preparations have become the most frequently prescribed products in the US. In 2011, 131 million prescriptions totaling up to 8 billion or more tablets for fixed-combination hydrocodone analgesic preparations were prescribed and dispensed in the US to over 47 million patients, representing about 4 times the number of prescriptions written for fixed-combination oxycodone preparations and about 10 times the number of prescriptions for codeine-containing preparations. In 2011, approximately 5 million prescriptions were dispensed for hydrocodone-containing combination antitussives.
Data from 2012 showed that 37 million Americans had used analgesics nonmedically (misuse and abuse) in their lifetime, and that roughly 70% of these individuals reported lifetime nonmedical use of fixed-combination hydrocodone preparations. Further, hydrocodone is associated with substantial numbers of reports of overdose, suicide, abuse, and dependence. While the addition of non-opiate analgesic ingredients decreases the abuse potential and the rates of abuse for hydrocodone-containing combination analgesic preparations are lower than those for oxycodone-containing preparations, hydrocodone-containing combinations have a high potential for abuse that is considered similar to that of schedule II oxycodone-containing combination preparations. There also is evidence to suggest that individuals are taking sufficient amounts of hydrocodone to create a hazard to their health or the safety of others or the community, that there is considerable diversion from legitimate channels, and that individuals are taking the drug on their own initiative rather than on the basis of medical advice. Similar to the pattern for abuse are the risks of psychological and physical dependence, which can be severe. Considering this and other evidence, a decision to reschedule these hydrocodone-containing combination preparations to C-II was made. However, because of concerns about the impact of this scheduling change on public health, particularly access to effective pain management, FDA recommended that the impact of this action be assessed through close continued monitoring.
Pregnancy, Fertility, and Lactation
Analysis of data from the National Birth Defects Prevention Study, a large population-based, case-control study, suggests that therapeutic use of opiates in pregnant women during the period of organogenesis is associated with a low absolute risk of birth defects, including heart defects, spina bifida, and gastroschisis. Oral hydrocodone bitartrate was not teratogenic in rats or rabbits at dosages or 25 or 50 mg/kg daily (equivalent to 2 or 10 times, respectively, a human dosage of 100 mg daily on a mg/m2 basis). In studies in rats, oral administration of hydrocodone bitartrate 10 mg/kg daily (approximately equivalent to a human dosage of 100 mg daily) during gestation and lactation was associated with reduced fetal viability (increase in stillborn pups and decrease in pup survival). At a dosage of 25 mg/kg daily, reduced nursing behavior and decreased pup body weight were observed; minimal maternal toxicity was observed at this dosage. In studies in rabbits, an increase in umbilical hernias, irregularly shaped bones, and delayed fetal skeletal maturation were observed at a maternally toxic dosage of 75 mg/kg daily (equivalent to 15 times a human dosage of 100 mg daily). An oral hydrocodone bitartrate dosage of 25 mg/kg daily (equivalent to approximately 5 times a human dosage of 100 mg daily) was associated with reduced fetal weights.
No effects on fertility were observed in male rats receiving hydrocodone bitartrate at dosages equivalent to 10 times a human dosage of 100 mg daily, although decreased weight of male reproductive organs was observed at dosages equivalent to 2.4 times a human dosage of 100 mg daily. Reductions in female fertility indices observed at a dosage equivalent to twice the human dosage of 100 mg daily are not thought to be clinically relevant to humans.
Hydrocodone is distributed into breast milk. The manufacturers state that a decision should be made whether to discontinue nursing or the drug, taking into account the importance of the drug to the woman. Infants exposed to hydrocodone through breast milk should be observed for excessive sedation, respiratory depression, GI effects, and altered feeding patterns. Symptoms of withdrawal can occur in opiate-dependent infants when maternal administration of opiates is discontinued or breast-feeding is stopped.
Drug Interactions
Drugs Affecting Hepatic Microsomal Enzymes
Because hydrocodone is metabolized by the cytochrome P-450 (CYP) microsomal enzyme system, principally by isoenzyme 3A4, concomitant use of hydrocodone with drugs that inhibit CYP3A4 activity may result in reduced clearance and increased plasma concentrations of the drug, possibly resulting in increased or prolonged opiate effects, including an increased risk of fatal respiratory depression. Concomitant administration of hydrocodone bitartrate (single 20-mg dose as extended-release tablets) and the potent CYP3A4 inhibitor ketoconazole (200 mg twice daily for 6 days) increased mean area under the concentration-time curve (AUC) and peak plasma concentration of hydrocodone by 135 and 78%, respectively. Conversely, concomitant use of hydrocodone with CYP3A4 inducers may result in increased clearance and decreased plasma concentrations of hydrocodone, with possible lack of efficacy or development of opiate withdrawal. If concomitant therapy with a CYP3A4 inducer is discontinued, an increase in plasma hydrocodone concentrations may occur, potentially increasing or prolonging therapeutic and adverse effects of the drug and increasing the risk of fatal overdosage. Therefore, caution should be exercised and patients who require concomitant therapy with a CYP3A4 inhibitor or inducer, or who have recently discontinued such therapy, should be monitored closely at frequent intervals, and dosage adjustments should be considered until stable drug effects are achieved.
Hydrocodone is metabolized to a lesser extent by CYP2D6; however, concomitant administration of hydrocodone bitartrate (single 20-mg dose as extended-release tablets) and the CYP2D6 inhibitor paroxetine (20 mg once daily for 12 days) did not alter systemic exposure to hydrocodone.
Alcohol
Alcohol and hydrocodone may cause additive CNS depression and may result in hypotension, profound sedation, coma, respiratory depression, and death. Patients receiving hydrocodone should be instructed to avoid alcohol, including alcoholic beverages and prescription or nonprescription preparations containing alcohol.
In addition to such additive depressant effects, concomitant use of alcohol with extended-release hydrocodone bitartrate capsules can result in increased plasma concentrations of the opiate and potentially fatal overdosage. Administration of extended-release hydrocodone bitartrate capsules (Zohydro ER) 50 mg with 40% alcohol in the fasted state increased the rate of hydrocodone absorption, increased peak plasma concentrations of the drug by an average of 2.4-fold (up to 3.9-fold in one individual), and increased the extent of absorption by an average of 1.2-fold (up to 1.7-fold in one individual).
Laxatives
Concomitant use of hydrocodone bitartrate extended-release tablets with strong laxatives that rapidly increase GI motility (e.g., lactulose) may result in decreased absorption and decreased plasma concentrations of the opiate. Patients receiving such concomitant therapy should be monitored closely for adverse events and changing analgesic requirements.
For further information about drug interactions involving opiate agonists (including hydrocodone bitartrate), see Drug Interactions in the Opiate Agonists General Statement 28:08.08.
HYDROcodone (Analgesic) Pharmacokinetics
Overall systemic exposure or bioavailability of hydrocodone bitartrate following administration as extended-release capsules (Zohydro ER) or tablets (Hysingla ER) is similar to that observed following administration of immediate-release fixed-combination preparations containing the drug in the same or similar dosage; however, peak plasma concentrations of the drug are lower with the extended-release formulations. Peak plasma concentrations of hydrocodone are attained approximately 1.3–1.7 hours after administration as an immediate-release preparation, 5 hours after administration as extended-release capsules, and 6–30 hours (median: 14–16 hours) after administration as extended-release tablets.
After administration of the extended-release capsules for 7 days, area under the plasma concentration-time curve (AUC) and peak concentrations of hydrocodone are approximately twofold higher than values attained on the first day of administration. At doses of up to 50 mg, the pharmacokinetics of extended-release hydrocodone bitartrate are independent of dose. Administration of the extended-release capsules with food does not substantially affect the extent of absorption, although peak plasma hydrocodone concentrations were increased by 27% following administration of a 20-mg dose of the extended-release capsules with a high-fat meal.
After single-dose administration of hydrocodone bitartrate extended-release tablets, peak concentrations and AUC of the drug increased linearly and in a slightly more than dose-proportional manner over the dose range of 20–120 mg. With once-daily dosing, peak plasma concentrations and AUC were 1.1- and 1.3-fold higher at steady state. Higher doses (80 or 120 mg versus 30 mg) produced larger fluctuations in peak-to-trough plasma concentrations of the drug. Although administration of the 120-mg extended-release tablets with a high-fat meal increased peak plasma concentrations by 54% compared with administration in the fasted state, AUC was increased by only 20% and the manufacturer states that the extended-release tablets may be administered without regard to meals.
Hydrocodone is about 36% bound to plasma proteins.
Hydrocodone is metabolized by N-demethylation, O-demethylation, and 6-keto reduction to the corresponding 6-α- and 6-β-hydroxy metabolites. Hydrocodone is metabolized principally by cytochrome P-450 (CYP) isoenzyme 3A4 to form norhydrocodone (N-demethylation) and to a lesser extent by CYP2D6 to form hydromorphone (O-demethylation). Hydrocodone also may be metabolized to a small extent by CYP2B6 and CYP2C19. Hydromorphone accounts for less than 3% of the circulating parent drug, but may contribute to the total analgesic effect of hydrocodone. Hydrocodone and its metabolites are eliminated mainly in urine; only about 6.5% of an administered dose is excreted as unchanged drug. About 99% of an administered dose is eliminated within 72 hours. The mean plasma half-life of the drug is 3.8–4.5 hours after oral administration as an immediate-release preparation and approximately 7–9 hours after oral administration as extended-release capsules or tablets.
Following oral administration of a single 20-mg dose of hydrocodone bitartrate as extended-release capsules, peak plasma concentrations of the drug were 15, 48, or 41% higher and AUC was 15, 57, or 44% higher in patients with mild, moderate, or severe renal impairment, respectively, compared with individuals with normal renal function. Following oral administration of a single 20-mg dose of hydrocodone bitartrate as extended-release capsules, peak plasma concentrations of the drug were 8–10% higher and AUC was 10 or 26% higher in patients with mild or moderate hepatic impairment, respectively, compared with individuals with normal hepatic function; pharmacokinetics of the drug were not evaluated in patients with severe hepatic impairment. Population analyses indicated that the pharmacokinetics of the drug were not substantially affected by gender or age of 65 years or older.
Following oral administration of a single 20-mg dose of hydrocodone bitartrate as extended-release tablets, peak plasma concentrations and AUC of the drug reportedly were 6 and 14% lower, respectively, in patients with mild hepatic impairment; 5 and 13% higher, respectively, in patients with moderate hepatic impairment; and 5 and 4% higher, respectively, in patients with severe hepatic impairment compared with individuals with normal hepatic function. Hepatic impairment did not substantially alter plasma protein binding of the drug. Following oral administration of a single 60-mg dose of the drug as extended-release tablets, peak plasma concentrations reportedly were 14, 23, or 11% higher and AUC was 13, 61, or 57% higher in patients with mild, moderate, or severe renal impairment, respectively, compared with individuals with normal renal function; among patients with end-stage renal disease requiring dialysis, peak plasma concentrations of the drug reportedly were decreased by 13% and AUC was increased by 4% compared with values in individuals with normal renal function.
Age (65 years or older) and gender do not appear to substantially alter exposure to hydrocodone.
Chemistry and Stability
Chemistry
Hydrocodone bitartrate is a phenanthrene-derivative opiate agonist that is used as an analgesic and antitussive agent. Hydrocodone is a hydrogenated-ketone derivative of codeine. Hydrocodone bitartrate occurs as fine, white crystals or as a crystalline powder and is soluble in water and slightly soluble in alcohol.
Stability
Hydrocodone bitartrate is affected by light. Hydrocodone bitartrate preparations should be stored in tight, light-resistant containers at 15–30°C.
Additional Information
For further information on the chemistry, pharmacology, pharmacokinetics, uses, cautions, chronic toxicity, acute toxicity, drug interactions, and dosage and administration of hydrocodone bitartrate, see the Opiate Agonists General Statement 28:08.08 and Hydrocodone Bitartrate 48:08.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Single-entity hydrocodone bitartrate preparations are subject to control under the Federal Controlled Substances Act of 1970 as schedule II (C-II) drugs; when available as a fixed-combination preparation in a concentration of 15 mg or less per dosage unit or 5 mL combined with a therapeutic amount of one or more non-opiate drugs or with a fourfold or greater quantity of isoquinolone opium alkaloid, hydrocodone previously was subject to control as a schedule III (C-III) drug. However, because of increasing concerns about misuse, abuse, and diversion, hydrocodone-containing preparations that previously were subject to control as schedule III drugs have been rescheduled and, effective October 6, 2014, are subject to control as schedule II (C-II) drugs. (See Cautions: Misuse and Abuse.)
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, extended-release |
10 mg |
Zohydro ER (C-II) |
Zogenix |
|
15 mg |
Zohydro ER (C-II) |
Zogenix |
||
|
20 mg |
Zohydro ER (C-II) |
Zogenix |
||
|
30 mg |
Zohydro ER (C-II) |
Zogenix |
||
|
40 mg |
Zohydro ER (C-II) |
Zogenix |
||
|
50 mg |
Zohydro ER (C-II) |
Zogenix |
||
|
Tablets, extended-release, film-coated |
20 mg |
Hysingla ER (C-II) |
Purdue Pharma |
|
|
30 mg |
Hysingla ER (C-II) |
Purdue Pharma |
||
|
40 mg |
Hysingla ER (C-II) |
Purdue Pharma |
||
|
60 mg |
Hysingla ER (C-II) |
Purdue Pharma |
||
|
80 mg |
Hysingla ER (C-II) |
Purdue Pharma |
||
|
100 mg |
Hysingla ER (C-II) |
Purdue Pharma |
||
|
120 mg |
Hysingla ER (C-II) |
Purdue Pharma |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
2.5 mg/5 mL with Acetaminophen 108 mg/5 mL* |
HYDROcodone Bitartrate and Acetaminophen Oral Solution (C-II) |
|
|
3.3 mg/5 mL with Acetaminophen 100 mg/5 mL* |
HYDROcodone Bitartrate and Acetaminophen Oral Solution (C-II) |
|||
|
Lortab Elixir (C-II) |
ECR |
|||
|
3.3 mg/5 mL with Acetaminophen 108 mg/5 mL* |
HYDROcodone Bitartrate and Acetaminophen Oral Solution (C-II) |
|||
|
Tablets |
2.5 mg with Acetaminophen 325 mg* |
HYDROcodone Bitartrate and Acetaminophen Tablets (C-II) |
||
|
5 mg with Acetaminophen 300 mg* |
HYDROcodone Bitartrate and Acetaminophen Tablets (C-II) |
|||
|
Vicodin (C-II; scored) |
AbbVie |
|||
|
5 mg with Acetaminophen 325 mg* |
HYDROcodone Bitartrate and Acetaminophen Tablets (C-II) |
|||
|
Lortab (C-II; scored) |
UCB |
|||
|
Norco (C-II; scored) |
Actavis |
|||
|
7.5 mg with Acetaminophen 300 mg* |
HYDROcodone Bitartrate and Acetaminophen Tablets (C-II) |
|||
|
Vicodin ES (C-II; scored) |
AbbVie |
|||
|
7.5 mg with Acetaminophen 325 mg* |
HYDROcodone Bitartrate and Acetaminophen Tablets (C-II) |
|||
|
Lortab (C-II; scored) |
UCB |
|||
|
Norco (C-II; scored) |
Actavis |
|||
|
10 mg with Acetaminophen 300 mg* |
HYDROcodone Bitartrate and Acetaminophen Tablets (C-II) |
|||
|
Vicodin HP (C-II; scored) |
AbbVie |
|||
|
10 mg with Acetaminophen 325 mg* |
HYDROcodone Bitartrate and Acetaminophen Tablets (C-II) |
|||
|
Lortab (C-II; scored) |
UCB |
|||
|
Norco (C-II; scored) |
Actavis |
|||
|
Tablets, film-coated |
2.5 mg with Ibuprofen 200 mg* |
HYDROcodone Bitartrate and Ibuprofen Film-coated Tablets (C-II) |
||
|
Reprexain (C-II) |
Gemini |
|||
|
5 mg with Ibuprofen 200 mg* |
HYDROcodone Bitartrate and Ibuprofen Film-coated Tablets (C-II) |
|||
|
Reprexain (C-II) |
Gemini |
|||
|
7.5 mg with Ibuprofen 200 mg* |
HYDROcodone Bitartrate and Ibuprofen Film-coated Tablets (C-II) |
|||
|
Vicoprofen (C-II) |
AbbVie |
|||
|
10 mg with Ibuprofen 200 mg* |
HYDROcodone Bitartrate and Ibuprofen Film-coated Tablets (C-II) |
|||
|
Reprexain (C-II) |
Gemini |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 19, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Oxycodone vs Hydrocodone vs OTC Pain Relievers
- Which drugs cause opioid-induced constipation?
- What drugs cause pinpoint pupils?
- Which painkiller should you use?
- Norco vs Vicodin - How do they compare?
More about hydrocodone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (202)
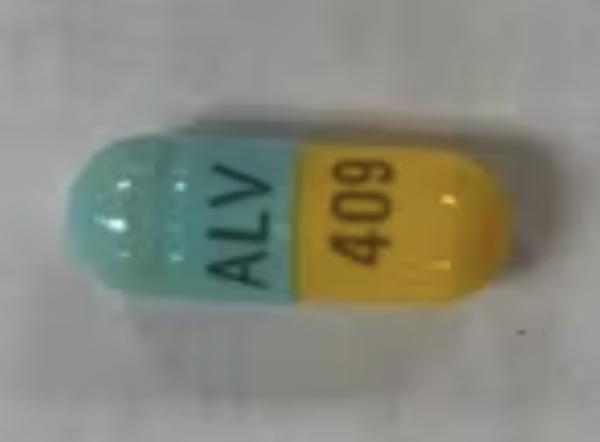
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antitussives
- Breastfeeding
- En español
Patient resources
Professional resources
- HYDROcodone Bitartrate (Antitussive) monograph
- Hydrocodone ER Capsules (FDA)
- Hydrocodone ER Tablets (FDA)