Glyburide (Monograph)
Brand name: Glynase
Drug class: Sulfonylureas
Introduction
Antidiabetic agent; sulfonylurea.
Uses for Glyburide
Type 2 Diabetes Mellitus
Used as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus.
Used as monotherapy or in combination with one or more other oral antidiabetic agents or insulin as an adjunct to diet and exercise in patients who do not achieve adequate glycemic control with diet, exercise, and oral antidiabetic agent monotherapy.
Commercially available as a single entity preparation and in fixed combination with metformin hydrochloride.
Guidelines from the American Diabetes Association (ADA) and other experts generally recommend that use of sulfonylureas for the treatment of type 2 diabetes mellitus be limited or discontinued due to increased risk of weight gain and hypoglycemia. Sulfonylureas may be considered in patients with access or cost barriers to other antidiabetic regimens. When used, these guidelines recommend the lowest possible dosage. When selecting a treatment regimen for diabetes, consider factors such as cardiovascular and renal comorbidities, drug efficacy and adverse effects, hypoglycemia risk, presence of overweight or obesity, cost, access, and patient preferences. Weight management should be included as a distinct treatment goal and other healthy lifestyle behaviors should also be considered.
Should notbe used for type 1 diabetes mellitus or diabetic ketoacidosis; such use contraindicated.
Glyburide Dosage and Administration
General
Patient Monitoring
-
Monitor with regular clinical and laboratory evaluations, including blood and/or urine glucose determinations, to determine the minimum effective dosage and to detect primary failure (inadequate lowering of blood glucose concentration at maximum recommended dosage) or secondary failure (loss of control of blood glucose concentration following an initial period of effectiveness ) to the drug.
-
Periodic HbA1cdeterminations are the principal means of assessing long-term glycemic control. Following initiation of therapy, determination of HbA1c at intervals of approximately 3 months is useful for assessing continued response to therapy.
Dispensing and Administration Precautions
-
Based on the Institute for Safe Medication Practices (ISMP), glyburide is a high-alert medication that has a heightened risk of causing significant patient harm when used in error.
-
The ISMP includes glyBURIDE and glipiZIDE on the ISMP List of Confused Drug Names, and recommends special safeguards to ensure the accuracy of prescriptions for these drugs.
-
The 2023 American Geriatrics Society (AGS) Beers Criteria for Potentially Inappropriate Medication (PIM) Use in Older Adults includes all sulfonylureas on the list of PIMs that are best avoided by older adults in most circumstances or under specific situations, such as certain diseases, conditions, or care settings. The criteria are intended to apply to adults ≥65 years of age in all ambulatory, acute, and institutional settings of care, except hospice and end-of-life care settings. The Beers Criteria Expert Panel specifically recommends to avoid sulfonylureas as first- or second-line monotherapy or add-on therapy unless there are substantial barriers to the use of safer and more effective agents; if a sulfonylurea is used, choose short-acting agents (e.g., glipizide) over long-acting agents (e.g., glyburide, glimepiride).
Administration
Oral Administration
Administer conventional or micronized formulations once daily with breakfast or first main meal. May administer in 2 divided doses in some patients (i.e., those receiving >10 mg daily [as conventional formulations] or >6 mg daily [as micronized glyburide]).
Micronized formulations arenotbioequivalent with conventional formulations; retitrate dosage when transferring patients from micronized to conventional formulations, or vice versa.
Patients who do not adhere to prescribed dietary and drug regimens are more likely to have unsatisfactory response to therapy. In patients usually well controlled by dietary management alone, short-term therapy may be sufficient during periods of transient loss of glycemic control.
Administer fixed combination with metformin hydrochloride once or twice daily with meals. See full prescribing information for additional administration instructions.
Administer glyburide at least 4 hours prior to colesevelam when drugs given concomitantly.
Dosage
Adults
Type 2 Diabetes Mellitus
Initial Dosage in Previously Untreated Patients
OralConventional formulations: Initially, 2.5–5 mg daily.
Micronized formulations: Initially, 1.5 –3 mg daily.
Fixed combination with metformin hydrochloride: Initially, 1.25 mg of glyburide and 250 mg of metformin hydrochloride once or twice daily.
Initial Dosage in Patients Transferred from Other Oral Antidiabetic Agents
OralConventional formulations: Initially, 2.5–5 mg daily.
Micronized formulations: Initially, 1.5–3 mg daily.
May discontinue most other oral hypoglycemic agents immediately. Initial or loading dose of glyburide is notnecessary.
Fixed combination with metformin hydrochloride: Initially, glyburide 2.5 mg/metformin hydrochloride 500 mg or glyburide 5 mg/metformin hydrochloride 500 mg twice daily in patients not adequately controlled on monotherapy with glyburide (or another sulfonylurea) or metformin. For patients previously receiving combination therapy with glyburide (or another sulfonylurea) and metformin, initial dosage should not exceed previous individual dosages of glyburide (or equivalent dosage of another sulfonylurea) and metformin.
Initial Dosage in Patients Transferred from Insulin
OralConventional formulations: Initially, 2.5–5 mg once daily (if insulin dosage is <20 units daily) or 5 mg once daily (if insulin dosage is 20–40 units daily); may discontinue insulin immediately. If insulin dosage is >40 units daily, reduce insulin dosage by 50% and initiate glyburide at 5 mg daily; withdraw insulin gradually and increase glyburide dosage in increments of 1.25–2.5 mg daily every 2–10 days.
Micronized formulations: Initially, 1.5–3 mg once daily (if insulin dosage is <20 units daily) or 3 mg once daily (if insulin dosage is 20–40 units daily); may discontinue insulin immediately. If insulin dosage is >40 units daily, reduce insulin dosage by 50% and initiate glyburide at 3 mg daily; withdraw insulin gradually and increase glyburide dosage in increments of 0.75–1.5 mg daily every 2–10 days.
Titration and Maintenance Dosage
OralConventional formulations: Increase dosage in increments of ≤2.5 mg at weekly intervals. Usual maintenance dosage is 1.25–20 mg daily. Maximum recommended dosage is 20 mg daily.
Micronized formulations: Increase dosage in increments of ≤1.5 mg at weekly intervals. Usual maintenance dosage is 0.75–12 mg daily. Maximum recommended dosage is 12 mg daily.
Fixed combination with metformin hydrochloride: Titrate dosage gradually based on glycemic control and tolerability up to a maximum daily dosage of 20 mg of glyburide and 2 g of metformin hydrochloride.
Special Populations
Hepatic Impairment
Conventional formulations: Initially, 1.25 mg daily. Dosage should be conservative to avoid hypoglycemic reactions.
Micronized formulations: Initially, 0.75 mg daily. Dosage should be conservative to avoid hypoglycemic reactions.
Fixed combination with metformin hydrochloride: Use not recommended.
Renal Impairment
Conventional formulations: Initially, 1.25 mg daily. Dosage should be conservative to avoid hypoglycemic reactions.
Micronized formulations: Initially, 0.75 mg daily. Dosage should be conservative to avoid hypoglycemic reactions.
Fixed combination with metformin hydrochloride: Do not initiate if eGFR 30—45 mL/minute per 1.73 m2. In patients already taking and eGFR falls below 45 mL/minute per 1.73 m2, assess benefits and risks of continuing therapy. Discontinue if eGFR <30 mL/minute per 1.73 m2.
Geriatric Patients
Conventional formulations: Initially, 1.25 mg daily
Micronized formulations: Initially, 0.75 mg daily.
Fixed combination with metformin hydrochloride: Use a lower dosage when initiating or increasing therapy.
Other Special Populations
Cautious dosing recommended in debilitated or malnourished patients or in patients with adrenal or pituitary insufficiency.
Conventional formulations: Initially, 1.25 mg daily
Micronized formulations: Initially, 0.75 mg daily.
Cautions for Glyburide
Contraindications
-
Known hypersensitivity to glyburide or any ingredient in the formulation.
-
Diabetic ketoacidosis with or without coma. Diabetic ketoacidosis should be treated with insulin.
-
Type 1 diabetes mellitus.
-
Concomitant bosentan therapy.
Warnings/Precautions
Increased Risk of Cardiovascular Mortality
Administration of oral antidiabetic agents reported to be associated with increased cardiovascular mortality compared to treatment with diet alone or diet with insulin therapy.
Warning based on study conducted by University Group Diabetes Program (UGDP), a long-term prospective clinical trial that reported patients treated for 5—8 years with tolbutamide (1.5 g per day) had a rate of cardiovascular mortality 2.5 times that of patients treated with diet alone. Results of the UGDP study have been exhaustively analyzed; there has been general disagreement in scientific and medical communities regarding study's validity and clinical importance.
Although only one drug in the sulfonylurea class (tolbutamide) was included in the UGDP study, it is prudent from a safety standpoint to consider that this warning may also apply to other oral antidiabetic drugs in this class, in view of their close similarities in mode of action and chemical structure.
Inform patients of potential risk and advantages of glyburide and alternative therapies.
Macrovascular Outcomes
Manufacturer states that no clinical studies have conclusively established macrovascular risk reduction with glyburide or any other antidiabetic drug.
Hypoglycemia
Severe, occasionally fatal, hypoglycemia reported. Debilitated, malnourished, or geriatric patients and patients with renal or hepatic impairment or adrenal or pituitary insufficiency may be particularly susceptible. Strenuous exercise, alcohol ingestion, insufficient caloric intake, or use in combination with other antidiabetic agents may increase risk. Hypoglycemia may be difficult to recognize in geriatric patients or in those receiving β-adrenergic blocking agents.
Appropriate patient selection and careful attention to dosage are important to avoid glyburide-induced hypoglycemia.
Risks, symptoms, and treatment of hypoglycemia, as well as conditions that predispose to its development, should be explained to patients and responsible family members.
Loss of Glycemic Control
Possible loss of glycemic control during periods of stress (e.g., fever, trauma, infection, surgery). Temporary discontinuance of glyburide and administration of insulin may be required.
Effectiveness of any antidiabetic agent, including glyburide, in lowering blood glucose to desirable level decreases in many patients over time which may be due to progression of disease severity or to diminished responsiveness to drug. Adequate dosage adjustment and adherence to dietary recommendations should be assessed before classifying patient as experiencing secondary failure to glyburide.
Hemolytic Anemia
Hemolytic anemia may develop in patients with glucose 6-phosphate dehydrogenase (G6PD) deficiency who receive sulfonylureas; consider a nonsulfonylurea antidiabetic agent in patients with G6PD deficiency. Hemolytic anemia also reported in patients receiving glyburide who did not have known G6PD deficiency.
Use in Fixed Combinations
When used in fixed combination with metformin hydrochloride, consider the cautions, precautions, and contraindications associated with metformin.
Specific Populations
Pregnancy
Insufficient evidence to evaluate drug-associated risk of adverse outcomes. Reproduction studies in animals have not revealed evidence of harm.
Abnormal maternal blood glucose concentrations may be associated with higher incidence of congenital abnormalities; however, use of glyburide in pregnant women is generally not recommended. Many experts recommend that insulin be used during pregnancy.
Prolonged, severe hypoglycemia lasting 4—10 days reported in some neonates born to women receiving other sulfonylurea antidiabetic agents up to time of delivery. To minimize risk of neonatal hypoglycemia if glyburide used during pregnancy, manufacturer recommends drug be discontinued at least 2 weeks before expected delivery date.
Lactation
Not known whether glyburide is distributed into human milk; discontinue nursing or the drug.
Females and Males of Reproductive Potential
Reproduction studies in rats and rabbits have not revealed evidence of impaired fertility.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
Increased risk of hypoglycemia; hypoglycemia may be difficult to recognize. Cautious dosing recommended.
Hepatic Impairment
Increased risk of hypoglycemia. Cautious dosing recommended.
Renal Impairment
Increased risk of hypoglycemia. Cautious dosing recommended.
Common Adverse Effects
With conventional and micronized formulations: nausea, epigastric fullness, heartburn.
With fixed-combination glyburide/metformin hydrochloride: diarrhea, headache, nausea/vomiting, abdominal pain, dizziness.
Drug Interactions
When using fixed-combination preparation containing metformin hydrochloride, also consider the drug interactions associated with metformin.
Drugs Affecting Hepatic Microsomal Enzymes
Glyburide principally metabolized by CYP2C9. Consider potential interactions with CYP2C9 inducers or inhibitors.
Protein-bound Drugs
Potential pharmacokinetic interaction and possible potentiation of hypoglycemic effects when used concomitantly with other highly protein-bound drugs.
Observe for adverse effects when glyburide therapy is initiated or discontinued and vice versa.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Potentiation of hypoglycemic effects |
Observe carefully for glycemic effects or loss of glycemic control when an ACE inhibitor is initiated or discontinued |
|
Alcohol |
Possible rare disulfiram-like reactions |
|
|
Anticoagulants, oral (e.g., coumarins) |
Possible displacement from plasma proteins and potentiation of hypoglycemic effects |
Observe carefully for adverse effects when oral anticoagulants are initiated or discontinued |
|
Antifungal agents, azole (i.e., fluconazole, miconazole) |
Increased glyburide concentrations; possible hypoglycemia |
|
|
β-Adrenergic blocking agents |
Impaired glucose tolerance or potentiation of hypoglycemic effects |
If concomitant therapy is necessary, a β1-selective adrenergic blocking agent may be preferred |
|
Bosentan |
Increased risk of elevated serum aminotransferase concentrations |
Concomitant use contraindicated |
|
Calcium-channel blocking agents |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control or for hypoglycemia when calcium-channel blocking agents are initiated or discontinued |
|
Chloramphenicol |
Potentiation of hypoglycemic effects |
Observe carefully for glycemic effects or loss of glycemic control when chloramphenicol is initiated or discontinued |
|
Clarithromycin |
Potentiation of hypoglycemic effects |
Observe carefully for glycemic effects or loss of glycemic control when clarithromycin is initiated or discontinued |
|
Colesevelam |
Reductions in glyburide AUC and peak plasma concentration with concomitant administration |
Administer glyburide ≥4 hours prior to colesevelam |
|
Contraceptives, oral |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when oral contraceptives are initiated or discontinued |
|
Corticosteroids |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when corticosteroids are initiated or discontinued |
|
Disopyramide |
Potentiation of hypoglycemic effects |
Observe carefully for glycemic effects or loss of glycemic control when disopyramide is initiated or discontinued |
|
Diuretics (e.g., thiazides) |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when diuretics are initiated or discontinued |
|
Estrogens |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when estrogens are initiated or discontinued |
|
Fluoroquinolone anti-infectives (e.g., ciprofloxacin) |
Potentiation of hypoglycemic effects |
Observe carefully for glycemic effects or loss of glycemic control when fluoroquinolone anti-infectives are initiated or discontinued |
|
Fluoxetine |
Potentiation of hypoglycemic effects |
Observe carefully for glycemic effects or loss of glycemic control when fluoxetine is initiated or discontinued |
|
Hydantoins |
Possible displacement from plasma protein and potentiation of hypoglycemic effects |
|
|
Isoniazid |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when isoniazid is initiated or discontinued |
|
MAO inhibitors |
Potentiation of hypoglycemic effects |
Observe closely for glycemic effects or loss of glycemic control when MAO inhibitors are initiated or discontinued |
|
Metformin |
Highly variable decreases in AUC and peak plasma concentrations of glyburide (certain preparations) with concomitant single-dose metformin in patients with type 2 diabetes mellitus; no changes in metformin pharmacokinetics or pharmacodynamics |
Clinical importance uncertain |
|
Niacin |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when niacin is initiated or discontinued |
|
NSAIAs |
Possible displacement from plasma proteins and potentiation of hypoglycemic effects |
Observe carefully for loss of glycemic control when NSAIAs are initiated or discontinued |
|
Phenothiazines |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when phenothiazines are initiated or discontinued |
|
Phenytoin |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when phenytoin is initiated or discontinued |
|
Probenecid |
Potentiation of hypoglycemic effects |
Observe closely for loss of glycemic control when probenecid is initiated or discontinued |
|
Rifampin |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when rifampin is initiated or discontinued |
|
Sulfonamides |
Possible displacement from plasma proteins and potentiation of hypoglycemic effects |
Observe carefully for adverse effects when sulfonamides are initiated or discontinued |
|
Sympathomimetic agents |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when sympathomimetic agents are initiated or discontinued |
|
Thyroid agents |
May exacerbate diabetes mellitus |
Observe carefully for loss of glycemic control when thyroid agents are initiated or discontinued |
|
Topiramate |
Reductions in AUC and peak plasma concentrations of glyburide and active metabolites 4-trans-hydroxyglyburide (M1) and 3-cis hydroxyglyburide (M2) Topiramate pharmacokinetics unaffected |
Glyburide Pharmacokinetics
Absorption
Bioavailability
Almost completely absorbed following oral administration.
Conventional and micronized glyburide preparations not bioequivalent.
Onset
Hypoglycemic action generally begins within 45–60 minutes and is maximal within 1.5–3 hours.
Duration
In single-dose studies in fasting healthy individuals, the degree and duration of blood-glucose lowering is proportional to glyburide dose and AUC.
In nonfasting diabetic patients, the hypoglycemic action may persist for up to 24 hours.
Food
Food does not affect rate or extent of absorption.
Special Populations
In patients with renal or hepatic impairment, serum concentrations may be increased.
Distribution
Extent
Distributed in substantial amounts into bile.
Appears to cross the placenta. Not known if distributed into breast milk.
Plasma Protein Binding
>99% (for glyburide).
>97% (for major metabolite 4-trans-hydroxyglyburide).
Elimination
Metabolism
Appears to be completely metabolized, probably in the liver.
Elimination Route
Excreted as metabolites in urine and feces in approximately equal proportions.
Minimally removed by hemodialysis.
Half-life
1.4–1.8 hours (for glyburide) or approximately 10 hours (for glyburide and metabolites).
Special Populations
In patients with severe renal impairment, clearance may be decreased and half-life prolonged.
Stability
Storage
Oral
Conventional or Micronized Preparations
Store at 20–25°C in tightly closed container; consult specific labeling.
Actions
-
Stimulates secretion of endogenous insulin from beta cells of the pancreas. Lowers blood glucose concentration in diabetic and nondiabetic individuals.
-
During prolonged administration, extrapancreatic effects (e.g., enhanced peripheral sensitivity to insulin, reduction of basal hepatic glucose production) contribute to the hypoglycemic action.
Advice to Patients
-
Advise patients of the potential risks and advantages of glyburide and of alternative therapy.
-
Inform patients of the importance of regular clinical and laboratory evaluations, including urine and/or fasting blood glucose determinations.
-
Advise patients of the importance of adhering to dietary instructions and regular physical activity.
-
Inform patients and responsible family members of the risk of hypoglycemia, the symptoms and treatment of hypoglycemic reactions, and conditions that predispose to the development of hypoglycemic reactions.
-
Inform patients of primary and secondary failure to oral sulfonylurea antidiabetic agents.
-
When glyburide is used in fixed combination with other drugs (i.e., metformin hydrochloride), inform patients of other important cautionary information about the concomitant agent(s).
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Advise patients to inform their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
1.25 mg* |
glyBURIDE Tablets |
|
|
2.5 mg* |
glyBURIDE Tablets |
|||
|
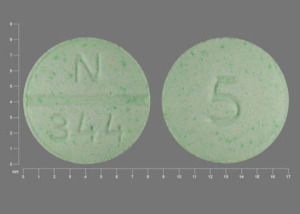
5 mg* |
glyBURIDE Tablets |
|||
|
Tablets (micronized) |
1.5 mg* |
glyBURIDE Micronized Tablets |
||
|
Glynase PresTab (scored) |
Pfizer |
|||
|
3 mg* |
glyBURIDE Micronized Tablets |
|||
|
Glynase PresTab (scored) |
Pfizer |
|||
|
6 mg* |
glyBURIDE Micronized Tablets |
|||
|
Glynase PresTab (scored) |
Pfizer |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
1.25 mg with Metformin Hydrochloride 250 mg* |
Glyburide with Metformin Hydrochloride Tablets |
|
|
2.5 mg with Metformin Hydrochloride 500 mg* |
Glyburide with Metformin Hydrochloride Tablets |
|||
|
5 mg with Metformin Hydrochloride 500 mg* |
Glyburide with Metformin Hydrochloride Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about glyburide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (9)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: sulfonylureas
- Breastfeeding