Etanercept (Monograph)
Brand name: Enbrel
Drug class: Tumor Necrosis Factor Inhibitors, Miscellaneous
Warning
- Serious Infections
-
Increased risk of serious infections involving various organ systems and sites that may require hospitalization or result in death; tuberculosis (frequently disseminated or extrapulmonary), invasive fungal infections (may be disseminated), bacterial (e.g., legionellosis, listeriosis) and viral infections, and other opportunistic infections reported.
-
Evaluate patients for latent tuberculosis infection prior to and periodically during etanercept therapy; if indicated, initiate appropriate antimycobacterial regimen prior to initiating etanercept therapy.
-
Closely monitor patients for infection, including active tuberculosis in those with a negative tuberculin skin test, during and after treatment. Discontinue etanercept if serious infection or sepsis occurs.
- Malignancy
-
Lymphoma and other malignancies (some fatal) reported in children and adolescents receiving TNF blocking agents.
Introduction
Tumor necrosis factor (TNF) inhibitor and biologic disease-modifying antirheumatic drug (DMARD); a recombinant soluble dimeric fusion protein.
Uses for Etanercept
Rheumatoid Arthritis
Used to manage the signs and symptoms of rheumatoid arthritis, to induce a major clinical response, to improve physical function, and to inhibit progression of structural damage in adults with moderate to severe disease.
Can be used alone or in combination with methotrexate.
Disease-modifying treatments for rheumatoid arthritis include conventional DMARDs (e.g., hydroxychloroquine, leflunomide, methotrexate, sulfasalazine), biologic DMARDs (e.g., TNF blocking agents, abatacept, tocilizumab, sarilumab, rituximab), and/or targeted synthetic DMARDs (e.g., Janus kinase inhibitors).
Guidelines generally support use of TNF blocking agents as add-on therapy to methotrexate in patients who do not meet treatment goals with methotrexate alone.
Specific agents for rheumatoid arthritis are selected according to current disease activity, prior therapies used, and presence of comorbidities.
Polyarticular Juvenile Idiopathic Arthritis
Used to manage the signs and symptoms of moderate to severe active polyarticular juvenile idiopathic arthritis in pediatric patients ≥2 years of age.
Drugs used for treatment of juvenile idiopathic arthritis include NSAIAs, systemic and intra-articular corticosteroids, conventional DMARDs (e.g., methotrexate, sulfasalazine, hydroxychloroquine, leflunomide), and biologic DMARDs (e.g., TNF blocking agents, abatacept, tocilizumab, rituximab).
Guidelines generally support use of TNF blocking agents as add-on therapy in patients with moderate to high disease activity despite the use of methotrexate.
Specific agents for juvenile idiopathic arthritis treatment are selected according to presence of certain risk factors (e.g., positive anti-cyclic citrullinated peptide antibodies, positive rheumatoid factor, joint damage), level of disease activity, involvement of specific joints, presence of certain comorbidities (e.g., uveitis), and prior therapies.
Psoriatic Arthritis
Used alone or in combination with methotrexate to manage the signs and symptoms of active psoriatic arthritis in adults, to improve physical function and to inhibit progression of structural damage.
Disease-modifying treatments for psoriatic arthritis include oral small molecules (OSMs; e.g., methotrexate, sulfasalazine, cyclosporine, leflunomide, apremilast), biologic DMARDs (e.g., TNF blocking agents, secukinumab, ixekizumab, ustekinumab, brodalumab, abatacept), and/or targeted synthetic DMARDs (e.g., tofacitinib).
Guidelines generally support use of TNF blocking agents as first-line treatment in patients with active psoriatic arthritis.
Recommendations for the use and selection of disease-modifying therapies in psoriatic arthritis vary based on the presence of certain disease characteristics (e.g., psoriatic spondylitis/axial disease, enthesitis) and comorbidities (e.g., inflammatory bowel disease, diabetes).
Ankylosing Spondylitis
Used to manage the signs and symptoms of active ankylosing spondylitis in adults.
Treatments for ankylosing spondylitis include NSAIAs, conventional DMARDs (e.g., methotrexate, sulfasalazine), biologic DMARDs (e.g., TNF blocking agents, secukinumab, ixekizumab), and/or targeted synthetic DMARDs (e.g., tofacitinib).
Guidelines generally support use of TNF blocking agents for treatment of ankylosing spondylitis in patients with active disease despite treatment with NSAIAs.
Recommendations for treatment selection in ankylosing spondylitis vary based the presence of certain comorbidities (e.g., iritis, inflammatory bowel disease).
Plaque Psoriasis
Used to manage moderate to severe chronic plaque psoriasis in adults who are candidates for systemic therapy or phototherapy.
Guidelines generally support use of TNF blocking agents in adults with moderate to severe psoriasis, either as monotherapy or in combination with topical, oral, or phototherapy. Recommendations for use and selection of psoriasis therapies vary based on patient age, disease characteristics (e.g., severity, location, presence of psoriatic arthritis), and comorbidities (e.g., inflammatory bowel disease).
Used to manage moderate to severe chronic plaque psoriasis in pediatric patients ≥4 years of age who are candidates for systemic therapy or phototherapy. Guidelines support the use of etanercept for moderate to severe psoriasis in pediatric patients ≥6 years of age.
Juvenile Psoriatic Arthritis
Used for the treatment of active juvenile psoriatic arthritis in pediatric patients ≥2 years of age.
Nonradiographic Axial Spondyloarthritis
May be useful for the management of nonradiographic axial spondyloarthritis† [off-label].
Acute Graft Versus Host Disease
Has been used for the management of acute graft versus host disease† [off-label].
Granulomatosis with Polyangiitis
Has been investigated for the management of granulomatosis with polyangiitis† [off-label] (previously designated an orphan drug by FDA for this use). However, use with standard immunosuppressive agents has been associated with an increased incidence of solid malignant tumors without added clinical benefit. Therefore, use in this condition not recommended.
Inflammatory Bowel Disease
Not effective in the treatment of inflammatory bowel disease† [off-label].
Etanercept Dosage and Administration
General
Pretreatment Screening
-
Evaluate all patients for active and latent tuberculosis prior to initiating therapy.
-
Complete all age-appropriate vaccinations as recommended by current immunization guidelines prior to treatment.
-
Screen at-risk patients for hepatitis B virus (HBV) infection before initiating therapy.
-
Do not initiate therapy in patients with an active infection, including clinically important localized infections.
Patient Monitoring
-
Periodically test all patients for active and latent tuberculosis during therapy.
-
Monitor closely for signs or symptoms of infection (e.g., fever, malaise, weight loss, sweats, cough, dyspnea, pulmonary infiltrates, serious systemic illness including shock) during and after treatment.
-
Perform periodic dermatologic evaluations in all patients at increased risk for skin cancer.
-
Evaluate and monitor chronic carriers of HBV during treatment and for up to several months following treatment.
Dispensing and Administration Precautions
-
To avoid medication errors, the Institute for Safe Medication Practices (ISMP) recommends that prescribers communicate both the brand and generic names for etanercept on the prescription order form.
Other General Considerations
-
Methotrexate, glucocorticoids, salicylates, nonsteroidal anti-inflammatory agents (NSAIAs), and analgesics may be continued in adults receiving etanercept for the management of rheumatoid arthritis, ankylosing spondylitis, or psoriatic arthritis.
-
Glucocorticoids, NSAIAs, and analgesics may be continued in pediatric patients with polyarticular juvenile idiopathic arthritis receiving etanercept.
Administration
Administer by sub-Q injection.
Sub-Q Administration
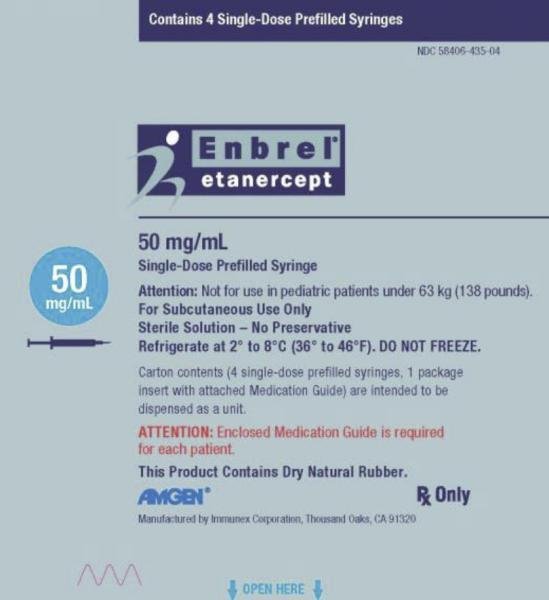
Administer a 50-mg dose as a single injection using the 50 mg/mL prefilled syringe, prefilled autoinjector, or prefilled cartridge, or as 2 injections using the 25 mg/0.5 mL prefilled syringe given on the same day once a week or on 2 different days 3–4 days apart. A 50-mg dose can also be obtained using two 25-mg single-dose vials or two 25-mg multidose vials of lyophilized etanercept, when the multidose vials are reconstituted and administered as recommended.
Administer sub-Q injections into the thighs, abdomen, or upper arm. Rotate injection sites. Do not inject into areas where skin is tender, bruised, red, or hard, or into scars, stretch marks, or psoriatic lesions.
For greater patient comfort, allow etanercept prefilled syringe to reach room temperature for about 15–30 minutes prior to administration; allow single-dose vial to reach room temperature for ≥30 minutes prior to administration. Allow single-dose prefilled cartridges and the prefilled auto-injector to reach room temperature for ≥30 minutes prior to administration.
Do not remove the needle cover from the prefilled syringe or prefilled auto-injector until immediately before administration. Do not remove the purple cap from the single-use prefilled cartridge until the cartridge is inside the reusable autoinjector, immediately prior to administration; do not leave the purple cap off for >5 minutes prior to injection.
When preparing a dose of etanercept from a single-dose vial of etanercept solution, use a 1-mL Luer-Lock syringe and a 22-gauge needle with Luer-Lock connection to withdraw the dose from the vial; use a 27-gauge needle with Luer-Lock connection to administer the dose. If 2 vials are required to administer the total prescribed etanercept dose, use the same syringe for each vial. Single-dose vials do not contain preservatives; discard any unused portion. Solution may contain small, white, proteinaceous particulates; do not administer if discolored or cloudy, or if foreign particulate matter is present.
Intended for use under the guidance and supervision of a clinician, but may be self-administered if the clinician determines that the patient and/or their caregiver is competent to prepare and safely administer the drug. The initial self-administered dose should be made under the supervision of a healthcare professional.
Reconstitution (25-mg Multiple-dose Vial)
For greater patient comfort, allow dose tray containing etanercept lyophilized powder and diluent to reach room temperature (about 15–30 minutes) prior to administration.
Reconstitute lyophilized powder by adding 1 mL of bacteriostatic water for injection (containing 0.9% benzyl alcohol) provided by the manufacturer to a 25-mg vial to provide a solution containing 25 mg/mL.
During reconstitution, very slowly add the diluent to the vial and gently swirl the contents to minimize foaming during dissolution; some foaming will occur.
May use vial adapter supplied by manufacturer to facilitate reconstitution and withdrawal of dose if only one dose will be withdrawn from the vial. If multiple doses will be withdrawn from the vial, use a syringe with a 25-gauge needle for reconstitution and withdrawal of dose from vial. Use a 27-gauge needle to administer the dose.
Avoid shaking and excessive or vigorous agitation of the vial to avoid excessive foaming.
The final volume in the vial will be about 1 mL.
Dissolution usually takes less than 10 minutes.
Do not filter solutions during preparation or administration.
Do not mix contents of one vial with, or transfer contents of one vial into, contents of another vial. Do not mix with other drugs.
Preparation Considerations
To achieve pediatric doses other than 25 mg or 50 mg, use the single-dose vial or reconstituted lyophilized powder in a multiple-dose vial.
Do not use 25-mg/0.5 mL prefilled syringe in pediatric patients weighing <31 kg. Do not use 50-mg/mL prefilled syringe, prefilled single-dose auto-injector, or prefilled single-dose auto-injector cartridge in pediatric patients weighing <63 kg.
Dosage
Pediatric Patients
Polyarticular Juvenile Idiopathic Arthritis
Sub-Q
Pediatric patients 2–17 years of age: 0.8 mg/kg (maximum 50 mg) once weekly in patients <63 kg; 50 mg once weekly in patients ≥63 kg.
Plaque Psoriasis
Sub-Q
Pediatric patients 4–17 years of age: 0.8 mg/kg (maximum 50 mg) once weekly in patients <63 kg; 50 mg once weekly in patients ≥63 kg.
Juvenile Psoriatic Arthritis
Sub-Q
Pediatric patients 2–17 years of age: 0.8 mg/kg (maximum 50 mg) once weekly in patients <63 kg; 50 mg once weekly in patients ≥63 kg.
Adults
Rheumatoid Arthritis
Sub-Q
50 mg once weekly.
Psoriatic Arthritis
Sub-Q
50 mg once weekly.
Ankylosing Spondylitis
Sub-Q
50 mg once weekly.
Psoriasis
Sub-Q
Initially, 50 mg twice weekly for 3 months. Initial dosages of 25 mg or 50 mg once weekly also have been effective; a dose-related effect observed.
Maintenance dosage: 50 mg once weekly.
Special Populations
Hepatic Impairment
No specific dosage recommendations at this time.
Renal Impairment
No specific dosage recommendations at this time.
Geriatric Patients
No specific dosage recommendations at this time; however, use caution since there is an increased incidence of infections among the geriatric population.
Patients with Diabetes
May need to reduce anti-diabetic medication in some patients as hypoglycemia reported following initiation of etanercept in patients with diabetes.
Cautions for Etanercept
Contraindications
-
Sepsis.
Warnings/Precautions
Warnings
Serious Infections
Increased risk of serious infections involving various organ systems, possibly resulting in hospitalization or death (see Boxed Warning). Opportunistic infections caused by bacterial, mycobacterial, invasive fungal, viral, parasitic, or other opportunistic organisms (e.g., aspergillosis, blastomycosis, candidiasis, coccidioidomycosis, histoplasmosis, legionellosis, listeriosis, pneumocystosis, tuberculosis) reported, particularly in patients receiving concomitant therapy with immunosuppressive agents (e.g., methotrexate, corticosteroids). Infections frequently are disseminated.
Increased incidence of serious infections observed with concomitant use of a TNF blocking agent and anakinra or abatacept. Concomitant use of etanercept and abatacept or anakinra not recommended.
Patients >65 years of age, with comorbid conditions, and/or receiving concomitant therapy with immunosuppressive agents (e.g., corticosteroids, methotrexate) may be at increased risk of infection.
Do not initiate etanercept in patients with active infections, including clinically important localized infections. Consider potential risks and benefits of the drug prior to initiating therapy in patients with a history of chronic, recurring, or opportunistic infections; patients with underlying conditions that may predispose them to infections; and patients who have been exposed to tuberculosis or who have resided or traveled in regions where tuberculosis or mycoses such as histoplasmosis, coccidioidomycosis, and blastomycosis are endemic.
Closely monitor patients during and after etanercept therapy for signs or symptoms of infection (e.g., fever, malaise, weight loss, sweats, cough, dyspnea, pulmonary infiltrates, serious systemic illness including shock), including the possible development of tuberculosis in patients who tested negative for latent tuberculosis prior to initiating therapy.
If new infection occurs during therapy, perform thorough diagnostic evaluation (appropriate for immunocompromised patient), initiate appropriate anti-infective therapy, and closely monitor patient. Discontinue etanercept if serious infection or sepsis develops.
Evaluate all patients for active or latent tuberculosis and for risk factors for tuberculosis prior to and periodically during therapy. When indicated, initiate appropriate antimycobacterial regimen for treatment of latent tuberculosis infection prior to etanercept therapy. Also consider antimycobacterial therapy prior to etanercept therapy for individuals with a history of latent or active tuberculosis in whom an adequate course of antimycobacterial treatment cannot be confirmed and for individuals with a negative tuberculin skin test who have risk factors for tuberculosis. Consultation with a tuberculosis specialist is recommended when deciding whether to initiate antimycobacterial therapy.
Reactivation of latent tuberculosis reported in patients receiving etanercept, although data suggest that risk is lower with etanercept than with TNF-blocking monoclonal antibodies.
Monitor all patients, including those with negative tuberculin skin tests, for active tuberculosis. Strongly consider tuberculosis in patients who develop new infections while receiving etanercept, especially if they previously have traveled to countries where tuberculosis is highly prevalent or have been in close contact with an individual with active tuberculosis.
Failure to recognize invasive fungal infections has led to delays in appropriate treatment. Consider empiric antifungal therapy in patients at risk for invasive fungal infections who develop severe systemic illness. Whenever feasible, consult specialist in fungal infections when making decisions regarding initiation and duration of antifungal therapy.
When deciding whether to reinitiate TNF blocking agent therapy following resolution of an invasive fungal infection, reevaluate risks and benefits, particularly in patients who reside in regions where mycoses are endemic. Whenever feasible, consult specialist in fungal infections.
Malignancies
Cases of lymphoma and other malignancies (some fatal) reported in children, adolescents, and adults receiving TNF blocking agents; patients receiving other immunosuppressive agents (e.g., azathioprine, methotrexate) concomitantly may be at increased risk (see Boxed Warning). Malignancies included lymphomas (e.g., Hodgkin disease, non-Hodgkin lymphoma, hepatosplenic T-cell lymphoma) and various other malignancies (e.g., leukemia, melanoma, solid organ cancers, leiomyosarcoma, hepatic malignancies, renal cell carcinoma).
FDA has concluded that there is an increased risk of malignancy with TNF blocking agents; however, the strength of the association is not fully characterized.
Solid noncutaneous malignant tumors reported in patients with granulomatosis with polyangiitis receiving etanercept and cyclophosphamide.
Consider possibility of and monitor for occurrence of malignancies during and following treatment with TNF blocking agents.
Consider periodic dermatologic examinations in all patients at increased risk.
Carefully consider risks and benefits of TNF blocking agents, especially in adolescents and young adults and especially in the treatment of Crohn disease or ulcerative colitis; etanercept is not effective in the management of inflammatory bowel disease.
Other Warnings and Precautions
Neurologic Reactions
New onset or exacerbation of CNS demyelinating disorders (some presenting with mental status changes and some associated with permanent disability) and peripheral nervous system demyelinating disorders reported rarely with etanercept or other TNF blocking agents.
Multiple sclerosis, transverse myelitis, optic neuritis, Guillain-Barré syndrome, peripheral demyelinating neuropathies, and new onset or exacerbation of seizure disorders reported in patients receiving etanercept.
Exercise caution when considering etanercept therapy in patients with preexisting or recent-onset central or peripheral nervous system demyelinating disorders.
New Onset or Worsening of Heart Failure
Worsening CHF (with and without identifiable precipitating factors) and, rarely, new-onset CHF (including in patients without known cardiovascular disease) reported, sometimes in patients <50 years of age. Use with caution and monitor carefully in patients with heart failure.
One study evaluating etanercept for treatment of CHF suggested higher mortality rate in etanercept-treated patients versus placebo recipients.
Hematologic Reactions
Possible pancytopenia including aplastic anemia, sometimes with fatal outcome. Use with caution in patients with a history of substantial hematologic abnormalities. Consider discontinuance in patients with confirmed hematologic abnormalities.
HBV Reactivation
Reactivation of HBV infection reported in patients previously infected with the virus. Death reported in a few individuals. Use of multiple immunosuppressive agents may contribute to HBV reactivation.
Screen at-risk patients prior to initiation of therapy. Evaluate and monitor patients with prior HBV infection before, during, and for up to several months after therapy. Safety and efficacy of concomitant antiviral therapy for prevention of HBV reactivation not established.
Discontinue etanercept and initiate appropriate treatment (e.g., antiviral therapy) if HBV reactivation occurs. Not known whether etanercept can be readministered once control of a reactivated HBV infection is achieved; caution advised in this situation.
Allergic Reactions
Possible allergic reactions. If serious allergic reaction or anaphylaxis occurs, immediately discontinue etanercept and initiate appropriate therapy.
Immunization
Patients may receive inactivated vaccines. No data available on secondary transmission of infection with live vaccines in etanercept-treated patients. Avoid concurrent administration of live vaccines wtih etanercept.
Review vaccination status and administer all age-appropriate vaccines included in current immunization guidelines, if possible, prior to initiating the drug.
Consider risks and benefits of administering live or live-attenuated vaccines to infants exposed to the drug in utero.
Autoimmunity
Possible formation of autoimmune antibodies. Lupus-like syndrome or autoimmune hepatitis reported rarely; may resolve upon discontinuance of the drug. If manifestations suggestive of lupus-like syndrome or autoimmune hepatitis develop, discontinue etanercept and carefully evaluate patient.
Nonneutralizing antibodies to etanercept may develop. Long-term immunogenicity remains to be determined.
Patients with Granulomatosis with Polyangiitis Receiving Immunosuppressants
Concurrent use of etanercept with immunosuppressive agents in patients with granulomatosis with polyangiitis not recommended. Increased incidence of non-cutaneous solid malignancies without improved clincial outcomes seen with the combination as compared to standard therapy alone.
Increased Mortality in Patients with Moderate to Severe Alcoholic Hepatitis
Use in patients with moderate to severe alcoholic hepatitis associated with higher mortality rate following 6 months of use; use with caution in such patients.
Specific Populations
Pregnancy
Available studies do not reliably establish an association between etanercept and major birth defects.
In a pregnancy registry cohort study, 9.4% of women in the etanercept-exposed cohort delivered a live-born infant with a major birth defect, compared with 3.5% of women with rheumatic diseases or psoriasis not exposed to the drug. In another study in pregnant women with chronic inflammatory disease, 7% of women in the etanercept-exposed cohort delivered a live-born infant with a major birth defect, compared with 4.7% of women not exposed to the drug. However, no pattern of major birth defects was observed in either study.
No fetal harm or malformations observed in animal studies.
Limited data suggest etanercept crosses placenta in small amounts. Clinical implications of in utero exposure are unknown.
Lactation
Limited data indicate etanercept is distributed into human milk in low concentrations and is minimally absorbed by breast-fed infants. No data regarding effects of etanercept on breast-fed infants or on milk production. Consider benefits of breast-feeding, importance of etanercept to the woman, and potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Pediatric Use
Used for management of polyarticular juvenile idiopathic arthritis in pediatric patients ≥2 years of age. Safety and efficacy for this indication not established in pediatric patients <2 years of age.
Used for management of juvenile psoriatic arthritis in pediatric patients ≥2 years of age. Safety and efficacy for this indication not established in pediatric patients <2 years of age.
Used for management of plaque psoriasis in pediatric patients ≥4 years of age. Safety and efficacy for this indication not established in pediatric patients <4 years of age.
Consider risks and benefits of administering live or live-attenuated vaccines to infants who were exposed to etanercept in utero.
Varicella infection associated with aseptic meningitis reported. If a varicella-susceptible pediatric patient has a clinically important exposure to varicella while receiving etanercept, discontinue the drug temporarily and consider use of varicella-zoster immune globulin.
Malignancies, some fatal, reported in children, adolescents, and young adults who received TNF blocking agents.
Inflammatory bowel disease reported rarely in patients with juvenile idiopathic arthritis receiving etanercept; the drug is not effective in the management of inflammatory bowel disease.
Geriatric Use
No substantial differences in safety or efficacy relative to younger adults; however, insufficient experience in geriatric patients with psoriasis to determine whether they respond differently than younger adults.
Possible increased incidence of infections in geriatric patients; use with caution.
Hepatic Impairment
Pharmacokinetics of etanercept not formally studied in patients with hepatic impairment.
Renal Impairment
Pharmacokinetics of etanercept not formally studied in patients with renal impairment.
Common Adverse Effects
Adverse effects reported in >5% of patients receiving etanercept include infections and injection site reactions.
Drug Interactions
Administered concomitantly with methotrexate, glucocorticoids, salicylates, NSAIAs, and/or analgesics in clinical studies.
Biologic Antirheumatic Agents
Use caution when switching from one biologic disease-modifying antirheumatic drug (DMARD) to another, since overlapping biologic activity may further increase the risk of infection.
Vaccines
Avoid concurrent administration of live vaccines. No data available on secondary transmission of infection by live vaccines in etanercept-treated patients.
Review vaccination status and administer all age-appropriate vaccines, if possible, prior to initiation of therapy. Consider risks and benefits of administering live or live-attenuated vaccines to infants who were exposed to etanercept in utero.
Specific Drugs
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Abatacept |
Increased incidence of infection and serious infection, without additional clinical benefit, reported with abatacept and TNF blocking agents in rheumatoid arthritis |
Concomitant use not recommended Use caution when switching from one biologic DMARD to another, since overlapping biologic activity may further increase risk of infection |
|
Anakinra |
Increased incidence of serious infections and neutropenia, without additional clinical benefit, reported in rheumatoid arthritis |
Concomitant use not recommended Use caution when switching from one biologic DMARD to another, since overlapping biologic activity may further increase risk of infection |
|
Cyclophosphamide |
Concomitant use associated with increased incidence of solid malignant tumors without additional clinical benefit |
Concomitant use not recommended |
|
Methotrexate |
Pharmacokinetic interaction unlikely Concomitant use not associated with additive toxicity |
|
|
Pneumococcal polysaccharide vaccine |
B-cell immune response adequate in etanercept-treated psoriatic arthritis patients, although titers moderately lower and twofold increases less common than in controls |
Clinical importance of observed differences not known |
|
Rituximab |
Increased risk of serious infection reported in patients who received rituximab and subsequently received a TNF blocking agent |
Use caution when switching from one biologic DMARD to another, since overlapping biologic activity may further increase risk of infection |
|
Sulfasalazine |
Decrease in neutrophil counts reported |
Clinical importance unknown |
Etanercept Pharmacokinetics
Absorption
Bioavailability
Bioavailability following sub-Q administration is approximately 60%. Peak plasma concentrations achieved within 69 hours.
Distribution
Extent
Limited data suggest etanercept crosses the placenta in small amounts.
Limited data indicate etanercept distributes into human milk in low concentrations.
Elimination
Half-life
68 hours in healthy adults; 102 hours in adults with rheumatoid arthritis.
Stability
Storage
Parenteral
Powder for Injection
2–8°C. Do not store under conditions of extreme heat or cold; do not freeze. Store in original carton to protect from light and physical damage. Do not shake.
May store individual dose trays containing etanercept powder for injection and diluent at 20–25°C for a maximum single period of 14 days, with protection from light, heat, and humidity. Following storage at room temperature, do not return to refrigerator; discard if not used within 14 days.
Store reconstituted solutions at 2–8°C; do not freeze or store at room temperature. Discard reconstituted solutions after 14 days.
Single-use Vial, Prefilled Syringe, Prefilled Auto-injector, Prefilled Auto-injector Cartridge
2–8°C. Do not store under conditions of extreme heat or cold; do not freeze. Store in original carton to protect from light and physical damage. Do not shake.
May store individual single-dose prefilled syringes, single-dose vials, single-dose prefilled cartridges, or single-dose prefilled auto-injectors at 20–25°C for a maximum single period of 14 days, with protection from light and heat. Following storage at room temperature, do not return to refrigerator; discard if not used within 14 days.
Keep reusable auto-injector device at room temperature (20–25°C); do not refrigerate.
Actions
-
Potent antagonist of TNF biologic activity.
-
High binding affinity for TNF and lymphotoxin-α (TNF-β); each molecule can bind to 2 TNF molecules. Prevents the binding of TNF to cell surface TNF receptors, thereby blocking the biologic activity of TNF.
-
Produced by recombinant DNA technology in a mammalian cell expression system.
Advice to Patients
-
Provide a copy of the manufacturer’s patient information (medication guide) for etanercept to all patients with each prescription of the drug. Advise patients about potential benefits and risks of etanercept. Advise patients to read the medication guide prior to initiation of therapy and each time the prescription is refilled.
-
If the patient or caregiver is to administer etanercept, provide careful instructions regarding proper dosage and administration, including proper aseptic technique, and proper disposal of needles and syringes.
-
Increased susceptibility to infection. Stress importance of seeking immediate medical attention if signs and symptoms suggestive of infection (e.g., fever, chills, flu-like symptoms, cough, burning or pain on urination) develop.
-
Risk of lymphoma, including hepatosplenic T-cell lymphoma, leukemia, or other malignancies with TNF blocking agents. Inform patients and caregivers about the increased risk of cancer development in children, adolescents, and young adults, taking into account the clinical utility of TNF blocking agents, the relative risks and benefits of these and other immunosuppressive drugs, and the risks associated with untreated disease. Stress importance of promptly informing clinicians if signs and symptoms of malignancies (e.g., unexplained weight loss; fatigue; abdominal pain; persistent fever; night sweats; easy bruising or bleeding; swollen lymph nodes in the neck, underarm, or groin; easy bruising or bleeding; hepatomegaly or splenomegaly) occur.
-
Advise patients to inform their clinician of any new or worsening medical conditions (e.g., neurologic conditions [e.g., demyelinating disorders], heart failure, autoimmune disorders [e.g., lupus-like syndrome, autoimmune hepatitis], psoriasis, cytopenias).
-
Advise patients to promptly contact a clinician if manifestations of an allergic reaction (e.g., rash, facial swelling, difficulty breathing) occur.
-
Advise patients to take the drug as prescribed and to not alter or discontinue therapy without first consulting with a clinician.
-
Advise women to inform their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses or any history of cancer, tuberculosis, HBV infection, or other chronic or recurring infections.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer's labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection, for subcutaneous use |
25 mg |
Enbrel (multi-dose vial for reconstitution supplied with diluent syringe containing 1 mL sterile bacteriostatic water for injection [with benzyl alcohol 0.9%], 27-gauge ½-inch needle, plunger, and vial adapter) |
Amgen |
|
Injection, for subcutaneous use |
25 mg/0.5 mL |
Enbrel (available as single-dose prefilled syringes and single-dose vials) |
Amgen |
|
|
50 mg/mL |
Enbrel (available as single-dose prefilled syringes and single-dose prefilled auto-injectors [SureClick]) |
Amgen |
||
|
Enbrel Mini (available as single-dose prefilled cartridges for use with the AutoTouch reusable autoinjector) |
Amgen |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Biological Products Related to etanercept
Find detailed information on biosimilars for this medication.
Frequently asked questions
- Does perispinal etanercept work for stroke recovery?
- What are the new drugs for rheumatoid arthritis (RA)?
- How long does it take for Enbrel (etanercept) to work?
- How long can Enbrel (etanercept) be left unrefrigerated?
- Can Enbrel (etanercept) be taken with antibiotics?
- Can you take Enbrel (etanercept) with a cold?
- What are the new drugs for plaque psoriasis?
- What are biologic drugs and how do they work?
- What biosimilars have been approved in the United States?
More about etanercept
- Check interactions
- Compare alternatives
- Reviews (324)
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: antirheumatics
- Breastfeeding