Dextroamphetamine (Monograph)
Brand names: Dexedrine, DextroStat
Drug class: Amphetamines
VA class: CN801
CAS number: 51-63-8
Warning
FDA drug safety communication (5/11/2023):
To address continuing concerns of misuse, abuse, addiction, and overdose of prescription stimulants, FDA is requiring updates to the Boxed Warning and other information to ensure the prescribing information is consistent across the entire class of these drugs.
The current prescribing information in some prescription stimulants does not provide up to date warnings about the harms of misuse and abuse, particularly when these drugs are shared with individuals for whom they are not prescribed. An FDA review found that most individuals who misuse prescription stimulants obtain their drugs from family members or peers, and that such sharing of prescription stimulants was a major contributor to nonmedical use and addiction.
Updates will include information that patients should never share their prescription stimulants with anyone, and the Boxed Warning information will describe the risks of misuse, abuse, addiction, and overdose consistently across all medicines in the class. The Boxed Warning will also advise healthcare professionals to monitor patients closely for signs and symptoms of misuse, abuse, and addiction.
Warning
- Abuse Potential
-
Amphetamines have a high potential for abuse.
-
Administration of amphetamines for prolonged periods of time may lead to drug dependence.
-
Particular attention should be paid to the possibility of individuals obtaining amphetamines for nontherapeutic use or distribution to others, and the drugs should be prescribed or dispensed sparingly.
-
The possibility that family members may abuse the patient’s medication should be considered.
- Sudden Death and Serious Cardiovascular Events
-
Possible sudden death and serious cardiovascular events, particularly in individuals who abuse amphetamines. (See Sudden Death and Serious Cardiovascular Events under Cautions.)
Introduction
Dextrorotatory isomer of amphetamine; noncatechol, sympathomimetic amine with CNS-stimulating activity.
Uses for Dextroamphetamine
Attention Deficit Hyperactivity Disorder
Used as an adjunct to psychological, educational, social, and other remedial measures in the treatment of attention deficit hyperactivity disorder (ADHD) (hyperkinetic disorder, hyperkinetic syndrome of childhood, minimal brain dysfunction).
Can be used for ADHD in pediatric (children, adolescents) as well as adult patients.
Almost all studies comparing behavioral therapy versus stimulants alone have shown a much stronger therapeutic effect from stimulants than from behavioral therapy, and stimulants (e.g., amphetamines, methylphenidate) remain the drugs of choice for the management of ADHD.
Drug therapy is not indicated in all patients with ADHD, and such therapy should be considered only after a complete evaluation including medical history has been performed.
Use should depend on age, adequate diagnosis (based on medical, special psychological, educational, and social resources), and the clinician’s assessment of the severity and duration of symptoms and should not depend solely on one or more behavioral characteristics.
Not recommended for ADHD symptoms associated with acute stress reactions.
Narcolepsy
Used as a stimulant to reduce daytime sleepiness in the management of narcolepsy.
Amphetamines remain the mainstay of treatment for narcolepsy based on a long record of clinical experience.
Tolerance to the clinical effects may develop with long-term therapy, particularly at high dosages.
Exogenous Obesity
Has been used as an adjunct to caloric restriction and behavioral modification in the short-term treatment of exogenous obesity† [off-label]. However, because of the limited efficacy (short-lived) and risk of abuse, such use no longer is included in the FDA-approved labeling and is discouraged.
The anorexigenic effect appears to be temporary, seldom lasting more than a few weeks, and tolerance may occur.
Obesity usually is a chronic disease, and short-term or intermittent therapy with anorexigenic drugs is unlikely to maintain a long-term benefit.
Dextroamphetamine Dosage and Administration
Administration
Oral Administration
When used as an anorexigenic, the dose is given 30–60 minutes before meals.
Conventional Tablets (Adderall, Dexedrine, and Generic Equivalents)
Administer initial dose on awakening; when administered in divided doses, additional doses are given at intervals of 4–6 hours. Because of potential for insomnia, avoid administering in the late evening.
Extended-release Capsules (Dexedrine Spansules and Generic Equivalents)
Administer initial dose on awakening. Because of potential for insomnia, avoid administering in the late evening.
Fixed-combination Extended-release Capsules (Adderall XR)
Administer on awakening. Because of potential for insomnia, avoid administering in the afternoon.
Administer capsules with or without food; capsules may be swallowed intact or the entire contents of a capsule(s) may be sprinkled on a small amount of applesauce immediately prior to administration. Do not subdivide the capsule contents. Do not chew or crush the pellets contained in the capsules and do not store the sprinkle/food mixture for later use.
Dosage
Dosages of dextroamphetamine sulfate alone and of total amphetamine base equivalence are the same.
Dextroamphetamine sulfate extended-release capsules or fixed-combination extended-release capsules containing various salts of dextroamphetamine and amphetamine can be substituted for their respective conventional short-acting preparations if less-frequent daily dosing is desirable.
Dosage of fixed-combination preparations containing various salts of dextroamphetamine and amphetamine is expressed as total amphetamine base equivalence.
Adjust dosage according to individual response and tolerance; the smallest dose required to produce the desired response should always be used.
When possible, therapy should be interrupted occasionally to determine if there is a recurrence of behavioral symptoms sufficient to require continued treatment.
Pediatric Patients
Attention Deficit Hyperactivity Disorder
Dosage titration usually requires 2–4 weeks.
Conventional Tablets (Adderall, Dexedrine, and Generic Equivalents)
OralDosing in pediatric patients may begin with once-daily administration in the early morning, adding a noon dose if the effect does not last throughout the school day. Increasing the morning dose may extend its duration. A third dose may be added at around 4 p.m. if necessary.
Children 3–5 years of age: Initially, 2.5 mg daily; the daily dosage is increased in 2.5-mg increments at weekly intervals until the optimum response is attained.
Children ≥6 years of age: Initially, 5 mg once or twice daily; the daily dosage is increased in 5-mg increments at weekly intervals until the optimum response is attained. Total daily dosage rarely should exceed 40 mg.
Extended-release Capsules (Dexedrine Spansules and Generic Equivalents)
OralTotal daily dosage of dextroamphetamine sulfate is the same for extended-release capsules (Dexedrine Spansules) and conventional tablets (Dexedrine).
Although extended-release capsules usually are administered once daily, some patients may benefit from dividing the dosage into 2 doses daily.
Children 3–5 years of age: Dosage must be initiated and titrated with conventional tablets in this age group. Can substitute with once-daily dosing only when the total daily dose is divisible by 5 mg.
Children ≥6 years of age: Initially, 5 or 10 mg once daily; the daily dosage is increased in 5-mg increments at weekly intervals until the optimum response is attained. Total daily dosage rarely should exceed 40 mg.
Fixed-combination Extended-release Capsules (Adderall XR)
OralChildren 6–12 years of age: Initially, 10 mg once daily; daily dosage may be increased in 5- or 10-mg increments at weekly intervals to a maximum dosage of 30 mg daily. Alternatively, initiate with 5 mg once daily when lower initial dosage is appropriate.
Adolescents 13–17 years of age: Initially, 10 mg once daily. Increase to 20 mg once daily after 1 week if symptoms not adequately controlled. No evidence that dosages >20 mg daily provide any additional benefit.
When switching from fixed-combination conventional tablets (Adderall) to fixed-combination extended-release capsules (Adderall XR), the total daily dosage may remain the same but may be given once daily.
Narcolepsy
When intolerable adverse effects occur (e.g., insomnia, anorexia), dosage should be reduced.
Conventional Tablets (Adderall, Dexedrine, and Generic Equivalents)
OralChildren 6–12 years of age: Initially, 5 mg daily; daily dosage is increased in 5-mg increments at weekly intervals until the optimum response is attained.
Children ≥12 years of age: Initially, 10 mg daily; daily dosage is increased in 10-mg increments at weekly intervals until the optimum response is attained.
Maintenance: Usually, 5–60 mg daily, depending on patient age and response, given in divided doses.
Extended-release Capsules (Dexedrine Spansules and Generic Equivalents)
OralTotal daily dosage of dextroamphetamine sulfate is the same for extended-release capsules (Dexedrine Spansules) and conventional tablets (Dexedrine).
Although extended-release capsules usually are administered once daily, some patients may benefit from dividing the dosage into 2 doses daily.
Children 6–12 years of age: Initially, 5 mg once daily; daily dosage is increased in 5-mg increments at weekly intervals until the optimum response is attained.
Children ≥12 years of age: Initially, 10 mg once daily; daily dosage is increased in 10-mg increments at weekly intervals until the optimum response is attained.
Maintenance: Usually, 5–60 mg once daily, depending on patient age and response, given in divided doses.
Adults
Attention Deficit Hyperactivity Disorder
Conventional Tablets (Adderall, Dexedrine, and Generic Equivalents)
Dosage titration usually requires 2–4 weeks.
OralInitially, 5 mg once or twice daily; the daily dosage is increased in 5- to 10-mg increments at weekly intervals until the optimum response is attained. Total daily dosage rarely should exceed 40 mg.
Extended-release Capsules (Dexedrine Spansules and Generic Equivalents)
OralTotal daily dosage of dextroamphetamine sulfate is the same for extended-release capsules (Dexedrine Spansules) and conventional tablets (Dexedrine).
Although extended-release capsules usually are administered once daily, some patients may benefit from dividing the dosage into 2 doses daily.
Initially, 5 or 10 mg once daily; the daily dosage is increased in 5-mg increments at weekly intervals until the optimum response is attained. Total daily dosage rarely should exceed 40 mg.
Fixed-combination Extended-release Capsules (Adderall XR)
Oral20 mg once daily as initial therapy or when switching from other drugs. No evidence that dosages >20 mg daily provide any additional benefit.
When switching from fixed-combination conventional tablets (Adderall) to fixed-combination extended-release capsules (Adderall XR), the total daily dosage may remain the same but may be given once daily.
Narcolepsy
When intolerable adverse effects occur (e.g., insomnia, anorexia), dosage should be reduced.
Conventional Tablets (Adderall, Dexedrine, and Generic Equivalents)
OralInitially, 10 mg daily; daily dosage is increased in 10-mg increments at weekly intervals until the optimum response is attained.
Maintenance: Usually, 5–60 mg daily, depending on response, given in divided doses.
Prescribing Limits
Pediatric Patients
Attention Deficit Hyperactivity Disorder
Excessive dosage can cause pediatric patients to become overfocused on the medication or to appear dull or overly restricted. Rarely, psychotic reactions, mood disturbances, or hallucinations can occur.
Conventional Tablets (Adderall, Dexedrine, and Generic Equivalents)
OralDosage rarely should exceed a total daily dosage of 40 mg. Individual doses rarely should exceed 10 mg each in children <25 kg.
Extended-release Capsules (Dexedrine Spansules and Generic Equivalents)
OralDosage rarely should exceed a total daily dosage of 40 mg. Individual doses rarely should exceed 10 mg each in children <25 kg.
Fixed-combination Extended-release Capsules (Adderall XR)
OralChildren 6–12 years of age: Dosages >30 mg daily have not been studied systematically.
Adolescents 13–17 years of age: Dosages up to 40 mg daily in individuals weighing ≤75 kg or 60 mg daily in those weighing >75 kg have been used in clinical studies; however, no evidence that dosages >20 mg daily provide any additional benefit.
Long-term use (>3 weeks in children or >4 weeks in adolescents) has not been studied systematically. If used for long-term therapy, periodically reevaluate the usefulness of the drug.
Adults
Attention Deficit Hyperactivity Disorder
Conventional Tablets (Adderall, Dexedrine, and Generic Equivalents)
OralDosages up to 0.9 mg/kg daily but rarely exceeding 40 mg daily. Such higher doses may be more likely in adults than in school-aged children because of increased dosing frequency to cover a longer work day.
Tolerance is more likely with relatively high dosages.
Extended-release Capsules (Dexedrine Spansules and Generic Equivalents)
OralDosages up to 0.9 mg/kg daily but rarely exceeding 40 mg daily. Such higher doses may be more likely in adults than in school-aged children because of increased dosing frequency to cover a longer work day.
Tolerance is more likely with relatively high dosages.
Fixed-combination Extended-release Capsules (Adderall XR)
OralDosages up to 60 mg daily have been evaluated in clinical studies; however, no evidence that dosages >20 mg daily provide any additional benefit.
Long-term use (>4 weeks) has not been studied systematically. If used for long-term therapy, periodically reevaluate the usefulness of the drug.
Special Populations
Hepatic Impairment
No specific hepatic dosage recommendations.
Renal Impairment
No specific renal dosage recommendations.
Geriatric Patients
No specific geriatric dosage recommendations.
Cautions for Dextroamphetamine
Contraindications
-
Contraindicated in patients with hypersensitivity or idiosyncrasy to the sympathomimetic amines, symptomatic cardiovascular disease, hyperthyroidism, moderate to severe hypertension, glaucoma, or advanced arteriosclerosis; within 14 days of MAO inhibitor therapy; and in agitated patients.
-
Although amphetamines generally should not be used in patients with a history of drug abuse, some experts state that this is not an absolute contraindication, provided the patient can be monitored more carefully than would otherwise be indicated.
Warnings/Precautions
Warnings
Sudden Death and Serious Cardiovascular Events
Sudden unexplained death, stroke, and MI reported in adults with ADHD receiving usual dosages of stimulants; sudden death also reported in children and adolescents with structural cardiac abnormalities or other serious cardiac conditions receiving usual dosages of the drugs.
Epidemiologic data suggest a possible association between use of stimulants and sudden unexplained death in healthy children and adolescents. FDA unable to conclude that these data affect evaluation of overall risk and benefit of stimulants used to treat ADHD in children and adolescents. FDA is conducting an ongoing safety review of amphetamines and other stimulants to evaluate possible link between use of these agents and sudden death in children. Pediatric patients with ADHD and their parents should avoid discontinuing the child’s use of such stimulants before consulting a clinician.
Thoroughly review medical history (including evaluation for family history of sudden death or ventricular arrhythmia) and perform physical examination in all children, adolescents, and adults being considered for stimulant therapy; if initial findings suggest presence of cardiac disease, perform further cardiac evaluation (e.g., ECG, echocardiogram).
In general, avoid use of CNS stimulants in patients with known serious structural cardiac abnormalities, cardiomyopathy, serious heart rhythm abnormalities, CAD, or other serious cardiac conditions. (See Contraindications under Cautions.)
Patients who develop exertional chest pain, unexplained syncope, or other manifestations suggestive of cardiac disease during stimulant therapy should undergo prompt cardiac evaluation.
Effects on BP and Heart Rate
Possible modest increases in average BP (i.e., by about 2–4 mm Hg) and heart rate (i.e., by about 3–6 bpm); larger increases may occur. Modest increases not expected to have short-term sequelae; however, monitor all patients for larger changes in BP and heart rate.
Caution advised in patients with underlying medical conditions that might be affected by increases in BP or heart rate (e.g., hypertension, heart failure, recent MI, ventricular arrhythmia).
Exacerbation or Precipitation of Psychotic Symptoms
May exacerbate symptoms of behavior disturbance and thought disorder in patients with preexisting psychotic disorder.
Psychotic symptoms (e.g., hallucinations, delusional thinking) may occur with usual dosages in children and adolescents without prior history of psychotic illness. If psychotic symptoms occur, consider causal relationship to stimulants, and discontinue therapy as appropriate.
Precipitation of Manic Symptoms
May precipitate mixed or manic episodes in ADHD patients with comorbid bipolar disorder; use with caution in these patients. Prior to initiating therapy, carefully screen patients with ADHD and comorbid depressive symptoms to identify risk for bipolar disorder; screening should include a detailed psychiatric history (e.g., family history of suicide, bipolar disorder, or depression).
Manic symptoms may occur with usual dosages in children and adolescents without prior history of mania. If manic symptoms occur, consider causal relationship to stimulants, and discontinue therapy as appropriate.
Aggression
Aggressive behavior and hostility (frequently observed in children and adolescents with ADHD) reported in patients receiving drug therapy for ADHD. No systematic evidence that stimulants cause these adverse effects; however, monitor patients beginning treatment for ADHD for onset or worsening of aggressive behavior or hostility.
Growth Suppression
Long-term (i.e., >14 months) administration expected to cause at least a temporary suppression of normal weight and/or height patterns in some children and adolescents. Dose-related weight loss reported in adolescents during first 4 weeks of therapy with fixed-combination extended-release capsules.
Manufacturers recommend monitoring growth during treatment; patients not growing or gaining weight as expected may require temporary discontinuance of treatment. However, AAP states that studies of stimulants in children found little or no decrease in expected height, with any decrease in growth early in treatment being compensated for later on.
Seizures
Possible lowering of seizure threshold in patients with history of seizures, in those with prior EEG abnormalities but no history of seizures, and, very rarely, in those without history of seizures and with no prior evidence of EEG abnormalities. If seizures occur, discontinue therapy.
Visual Effects
Visual disturbances (difficulty with accommodation, blurred vision) reported with stimulants.
Sensitivity Reactions
Tartrazine Sensitivity
Some commercially available preparations of dextroamphetamine (e.g., DextroStat, Dexedrine tablets) contain the dye tartrazine (FD&C yellow No. 5), which may cause allergic reactions including bronchial asthma in susceptible individuals. Incidence of tartrazine sensitivity is low, but it frequently occurs in patients who are sensitive to aspirin.
General Precautions
Least amount of amphetamine feasible should be prescribed or dispensed at one time in order to minimize possible overdosage.
Tics
Amphetamines reported to exacerbate motor and phonic tics and Tourette’s syndrome. However, a history of tics or their development during therapy is not an absolute contraindication to continued use. Several controlled studies have not found stimulants to worsen or precipitate tics or Tourette’s syndrome. Nevertheless, evaluate for presence of tics and Tourette’s syndrome in children and their families prior to initiating stimulant therapy.
Specific Populations
Pregnancy
Category C.
Risk of prematurity, low birth weight, and withdrawal symptoms (e.g., dysphoria, lassitude, agitation) in infants born to dependent women.
Lactation
Distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Not recommended for ADHD in children <3 years of age.
Aggressive behavior, hostility, and psychotic (e.g., hallucinations, delusional thinking) or manic symptoms reported in children and adolescents receiving stimulants for management of ADHD. (See Warnings under Cautions.)
Sudden death reported in children and adolescents with structural cardiac abnormalities or other serious cardiac conditions receiving usual dosages of stimulants. Epidemiologic data also suggest a possible association between use of stimulants and sudden death in healthy children and adolescents. (See Sudden Death and Serious Cardiovascular Events under Cautions.)
Long-term administration expected to cause at least a temporary suppression of normal weight and/or height patterns in some children and adolescents. (See Growth Suppression under Cautions.)
Hepatic Impairment
Possible inhibition of drug elimination, resulting in prolonged exposure.
Renal Impairment
Possible inhibition of drug elimination, resulting in prolonged exposure.
Common Adverse Effects
Most commonly abdominal pain (stomachache), loss of appetite, insomnia.
Also, palpitations, tachycardia, elevation of BP, overstimulation, restlessness, dizziness, euphoria, dyskinesia, dysphoria, tremor, headache, dryness of mouth, taste aberration, diarrhea, constipation, abdominal bloating, impotence, changes in libido.
Isolated reports of cardiomyopathy associated with chronic amphetamine use.
Anorexia and weight loss may occur as undesirable effects when amphetamines are used for other than the anorectic effect.
Drug Interactions
Inhibits MAO.
Amphetamine or metabolites modestly inhibit CYP2D6, 1A2, and 3A4 in vitro. In vivo effects on metabolism of drugs metabolized by CYP isoenzymes not known.
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Acidifying agents, GI (ascorbic acid, glutamic acid hydrochloride, reserpine) |
Decreases absorption, serum concentrations, and efficacy of amphetamines |
|
|
Acidifying agents, urinary (ammonium chloride, sodium acid phosphate) |
Increases urinary excretion and decreases serum concentrations and efficacy of amphetamines |
|
|
Adrenergic blockers |
Potential inhibition of adrenergic blockade |
|
|
Alkalinizing agents, GI (antacids, sodium bicarbonate) |
Increases absorption and serum concentrations and potentiates the effects of amphetamines |
Avoid concomitant use |
|
Alkalinizing agents, urinary (acetazolamide and some thiazides) |
Decreases urinary excretion and increases serum concentrations and potentiates the effects of amphetamines |
|
|
Antidepressants, tricyclic (desipramine, protriptyline) |
Enhanced activity of tricyclic antidepressants; desipramine or protriptyline cause striking and sustained increases in the concentration of dextroamphetamine in the brain; cardiovascular effects can be potentiated |
|
|
Antihistamines |
May counteract the sedative effects of antihistamines |
|
|
Antihypertensives |
May antagonize the hypotensive effects of antihypertensives |
|
|
Chlorpromazine |
Inhibits the central stimulant effects of amphetamines by blocking dopamine and norepinephrine receptors |
Can be used to treat amphetamine poisoning |
|
Ethosuximide |
Intestinal absorption may be delayed by amphetamines |
|
|
Haloperidol |
Inhibits the central stimulant effects of amphetamines by blocking dopamine receptors |
|
|
Lithium carbonate |
May inhibit the anorectic and stimulatory effects of amphetamine |
|
|
MAO inhibitors |
Slow the metabolism of amphetamines, increasing their effect on the release of norepinephrine and other monoamines leading to headaches and other signs of hypertensive crisis Toxic neurologic effects, hypertensive crisis, and malignant hyperpyrexia can occur, sometimes with fatal results |
Amphetamines contraindicated in patients currently or recently (within 14 days) receiving MAO inhibitor |
|
Meperidine |
Amphetamines potentiate the analgesic effect of meperidine |
|
|
Methenamine |
Acidifying agents used with methenamine increase urinary excretion and decrease efficacy of amphetamines |
|
|
Norepinephrine |
Amphetamines enhance the adrenergic effects of norepinephrine |
|
|
Phenobarbital |
Amphetamines may delay absorption of phenobarbital; concomitant use may produce a synergistic anticonvulsant action |
|
|
Phenytoin |
Amphetamines may delay absorption of phenytoin; concomitant use may produce a synergistic anticonvulsant action |
|
|
Propoxyphene |
In propoxyphene overdosage, amphetamine CNS stimulation is potentiated and fatal convulsions can occur |
|
|
Sympathomimetic agents |
Enhanced activity of sympathomimetic agents |
|
|
Test, plasma corticosteroids |
Can elevate plasma corticosteroid concentrations; this increase is greatest in the evening |
|
|
Test, urinary steroids |
May interfere with urinary steroid determinations |
|
|
Veratrum alkaloids |
Amphetamines inhibit the hypotensive effect of veratrum |
Dextroamphetamine Pharmacokinetics
Absorption
Bioavailability
Similar for dextroamphetamine sulfate extended-release capsules versus immediate-release tablets.
Plasma concentration-time profiles for fixed combinations containing various salts of dextroamphetamine and amphetamine are similar for single 20-mg extended-release dose versus two 10-mg immediate-release doses given 4 hours apart.
Peak plasma concentration and AUC of amphetamines decrease with increasing body weight in individuals receiving fixed-combination extended-release capsules (Adderall XR).
Duration
Therapeutic effects persist for 4–24 hours.
Food
Food does not affect the rate or extent of absorption of dextroamphetamine sulfate from the extended-release capsules (e.g., Dexedrine Spansules).
Food does not affect the extent of absorption of the fixed-combination extended-release preparation (Adderall XR), but prolongs Tmax by 2.5 hours (for d-amphetamine) and 2.1 hours (for l-amphetamine). Opening the capsule and sprinkling the contents on applesauce results in comparable absorption to the intact capsule taken in the fasted state.
Plasma Concentrations
Tmax, immediate-release dextroamphetamine sulfate: About 3 hours.
Tmax, extended-release dextroamphetamine sulfate: About 8 hours.
Tmax, immediate-release fixed combinations containing various salts of dextroamphetamine and amphetamine: About 3 hours.
Tmax, extended-release fixed combinations containing various salts of dextroamphetamine and amphetamine: About 7 hours.
Therapeutic plasma concentrations are 5–10 mcg/dL.
Distribution
Extent
Distributed widely throughout body, with high levels in the brain.
Apparently crosses the placenta since withdrawal manifestations have occurred in neonates.
Distributed into milk in concentrations 3–7 times maternal blood concentrations.
Volume of distribution increases with increasing body weight in individuals receiving fixed-combination extended-release capsules.
Elimination
Metabolism
Metabolized to several active metabolites.
Enzymes involved in metabolism not clearly defined; however, CYP2D6 is involved with formation of at least one metabolite. Because CYP2D6 is genetically polymorphic, potential variability in metabolism among patients exists.
Elimination Route
With normal urinary pH, excreted in urine as unchanged drug (approximately 30–40%) and metabolites (approximately 50%). Changes in urinary pH may alter excretion; urinary recovery of unchanged drug reported to range from 1–75%, depending on urinary pH. (See Specific Drugs and Laboratory Tests under Interactions.)
Clearance increases with increasing body weight in individuals receiving fixed-combination extended-release capsules. On a mg/kg basis, however, children have higher clearance than adolescents or adults.
Half-life
Children 6–12 years of age: 9 hours (for d-amphetamine) or 11 hours (for l-amphetamine).
Adolescents 13–17 years of age: 11 hours (for d-amphetamine) or 13–14 hours (for l-amphetamine).
Adults: 10 hours (for d-amphetamine) or 13 hours (for l-amphetamine).
Elimination half-life increases with increasing body weight in individuals receiving fixed-combination extended-release capsules.
Stability
Storage
Oral
Conventional Tablets
Tight, light-resistant containers at 15–30°C.
Extended-release Capsules
Tight, light-resistant containers at 20–25°C.
Fixed-combination Conventional Tablets and Extended-release Capsules
Tight, light-resistant containers at 25°C (may be exposed to 15–30°C).
Actions
-
Amphetamines are sympathomimetic amines with CNS stimulant activity.
-
May block the reuptake of norepinephrine and dopamine into the presynaptic neuron and increase the release of these monoamines into the extraneural space.
-
Pharmacologic actions of amphetamines are qualitatively similar to those of ephedrine and include CNS and respiratory stimulation and sympathomimetic activity including pressor response, mydriasis, bronchodilation, and contraction of the urinary bladder sphincter.
-
On a weight basis, dextroamphetamine has a stronger CNS action and a lesser activity on the peripheral nervous system than does the racemic amphetamine. The CNS stimulating effect of dextroamphetamine is approximately twice that of amphetamine.
-
Mechanism of action on peripheral structures is thought to be a combination of release of norepinephrine from stores in adrenergic nerve terminals and a direct action on both alpha and beta receptor sites.
-
Mechanism of action involved in the central effect has not been determined. The main sites of CNS action appear to be the cerebral cortex and possibly the reticular-activating system; stimulation by an amphetamine causes an increase in motor activity, mental alertness, diminished sense of fatigue, brighter spirits, and mild euphoria.
-
Theories of dysfunction in ADHD focus on the prefrontal cortex, which controls many executive functions (e.g., planning, impulse control). Stimulants have putative effects on central dopamine and norepinephrine pathways that are crucial in frontal lobe function.
-
Produces an anorexigenic effect, leading to loss of weight. No primary effect on appetite has been demonstrated in humans and it has been postulated that anorexigenic effects are secondary to increased sympathetic activity resulting from release of norepinephrine and dopamine. May also cause a loss of acuity of smell and taste, which may contribute to the anorexigenic effect of the drugs.
Advice to Patients
-
Provide patient or caregiver with a copy of the manufacturer’s patient information (medication guide); discuss and answer questions about its contents as needed. Instruct patient or caregiver to read and understand contents of medication guide before initiating therapy and each time the prescription is refilled.
-
Advise parents with concerns about long-term effects (e.g., effects on weight) and the need for continued therapy that drug holidays can be considered in consultation with the patient’s clinician. However, the benefits versus risks of such interruptions in therapy have not been established.
-
Advise to take drug, particularly extended-release capsules, early in the day to minimize insomnia.
-
Advise not to chew or crush the pellets contained in the capsules and not to store the sprinkle/food mixture for later use.
-
Advise not to increase dosage unless instructed by their clinician.
-
Advise that appetite suppression may occur. Giving the morning dose with a meal and providing a high-caloric drink or snack late in the evening when the stimulant effects have subsided may be helpful.
-
Question about possible substance abuse, including in other family members (since they may abuse the patient’s medication supply).
-
Advise to inform clinician immediately if adverse cardiovascular (e.g., chest pain, shortness of breath, fainting) or psychiatric effects (e.g., hallucinations, delusional thinking, mania) occur.
-
Instruct about the potential for dextroamphetamine to impair patient’s ability to perform potentially hazardous activities, such as driving or operating heavy machinery.
-
Advise narcoleptic patients with severe sleepiness as a manifestation of their disease to avoid potentially dangerous activities at home and work and to not operate a motor vehicle until sleepiness is appropriately controlled by stimulant drug therapy.
-
Advise narcoleptic patients about occupational and social accommodation for disabilities associated with their disease (e.g., advise about legal guidance provided by the Americans with Disabilities Act).
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, dietary supplements, and herbal products, as well as any concomitant illnesses/conditions (e.g., cardiac/cardiovascular disease, thyroid disease, glaucoma, suicidal ideation or behaviors, mental/psychiatric disorder, seizures, hepatic or renal disease).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as schedule II (C-II) drugs.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, extended-release |
5 mg* |
Dexedrine Spansule (C-II; with povidone and propylene glycol) |
GlaxoSmithKline |
|
Dextroamphetamine Sulfate Capsules SR (C-II) |
Barr |
|||
|
10 mg* |
Dexedrine Spansule (C-II; with povidone and propylene glycol) |
GlaxoSmithKline |
||
|
Dextroamphetamine Sulfate Capsules SR (C-II) |
Barr |
|||
|
15 mg* |
Dexedrine Spansule (C-II; with povidone and propylene glycol) |
GlaxoSmithKline |
||
|
Dextroamphetamine Sulfate Capsules SR (C-II) |
Barr |
|||
|
Tablets |
5 mg* |
Dexedrine (C-II; with tartrazine, scored) |
GlaxoSmithKline |
|
|
Dextroamphetamine Sulfate Tablets (C-II; scored) |
Barr |
|||
|
DextroStat (C-II, scored) |
Shire |
|||
|
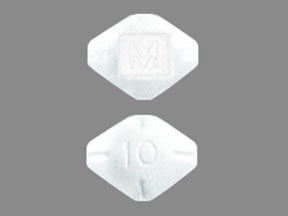
10 mg* |
Dextroamphetamine Sulfate Tablets (C-II; scored) |
Barr |
||
|
DextroStat (C-II; with tartrazine, double-scored) |
Shire |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, extended-release |
5 mg total amphetamine (as 1.25 mg with Amphetamine Sulfate 1.25 mg, Amphetamine Aspartate 1.25 mg, and Dextroamphetamine Saccharate 1.25 mg) |
Adderall XR (C-II) |
Shire |
|
10 mg total amphetamine (as 2.5 mg with Amphetamine Sulfate 2.5 mg, Amphetamine Aspartate 2.5 mg, and Dextroamphetamine Saccharate 2.5 mg) |
Adderall XR (C-II) |
Shire |
||
|
15 mg total amphetamine (as 3.75 mg with Amphetamine Sulfate 3.75 mg, Amphetamine Aspartate 3.75 mg, and Dextroamphetamine Saccharate 3.75 mg) |
Adderall XR (C-II) |
Shire |
||
|
20 mg total amphetamine (as 5 mg with Amphetamine Sulfate 5 mg, Amphetamine Aspartate 5 mg, and Dextroamphetamine Saccharate 5 mg) |
Adderall XR (C-II) |
Shire |
||
|
25 mg total amphetamine (as 6.25 mg with Amphetamine Sulfate 6.25 mg, Amphetamine Aspartate 6.25 mg, and Dextroamphetamine Saccharate 6.25 mg) |
Adderall XR (C-II) |
Shire |
||
|
30 mg total amphetamine (as 7.5 mg with Amphetamine Sulfate 7.5 mg, Amphetamine Aspartate 7.5 mg, and Dextroamphetamine Saccharate 7.5 mg) |
Adderall XR (C-II) |
Shire |
||
|
Tablets |
5 mg total amphetamine (as 1.25 mg with Amphetamine Aspartate 1.25 mg, Amphetamine Sulfate 1.25 mg, and Dextroamphetamine Saccharate 1.25 mg) |
Adderall (C-II; double-scored) |
Shire |
|
|
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, and Amphetamine Sulfate Tablets (C-II; double-scored) |
Barr |
|||
|
7.5 mg total amphetamine (as 1.875 mg with Amphetamine Aspartate 1.875 mg, Amphetamine Sulfate 1.875 mg, and Dextroamphetamine Saccharate 1.875 mg) |
Adderall (C-II; double-scored) |
Shire |
||
|
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, and Amphetamine Sulfate Tablets (C-II; double-scored) |
Barr |
|||
|
10 mg total amphetamine (as 2.5 mg with Amphetamine Aspartate 2.5 mg, Amphetamine Sulfate 2.5 mg, and Dextroamphetamine Saccharate 2.5 mg) |
Adderall (C-II; double-scored) |
Shire |
||
|
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, and Amphetamine Sulfate Tablets (C-II; double-scored) |
Barr |
|||
|
12.5 mg total amphetamine (as 3.125 mg with Amphetamine Aspartate 3.125 mg, Amphetamine Sulfate 3.125 mg, and Dextroamphetamine Saccharate 3.125 mg) |
Adderall (C-II; double-scored) |
Shire |
||
|
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, and Amphetamine Sulfate Tablets (C-II; double-scored) |
Barr |
|||
|
15 mg total amphetamine (as 3.75 mg with Amphetamine Aspartate 3.75 mg, Amphetamine Sulfate 3.75 mg, and Dextroamphetamine Saccharate 3.75 mg) |
Adderall (C-II; double-scored) |
Shire |
||
|
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, and Amphetamine Sulfate Tablets (C-II; double-scored) |
Barr |
|||
|
20 mg total amphetamine (as 5 mg with Amphetamine Aspartate 5 mg, Amphetamine Sulfate 5 mg, and Dextroamphetamine Saccharate 5 mg) |
Adderall (C-II; double-scored) |
Shire |
||
|
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, and Amphetamine Sulfate Tablets (C-II; double-scored) |
Barr |
|||
|
30 mg total amphetamine (as 7.5 mg with Amphetamine Aspartate 7.5 mg, Amphetamine Sulfate 7.5 mg, and Dextroamphetamine Saccharate 7.5 mg) |
Adderall (C-II; double-scored) |
Shire |
||
|
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate and Amphetamine Sulfate Tablets (C-II; double-scored) |
Barr |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 18, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- 'Black Beauties' capsules in the 1970's - What drug was that?
- Concerta vs Adderall - What's the difference between them?
- What pill has a half moon and 26 On same side. orange,and round?
More about dextroamphetamine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (300)
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: CNS stimulants
- Breastfeeding
- En español
Patient resources
Professional resources
- Dextroamphetamine prescribing information
- Dextroamphetamine ER (FDA)
- Dextroamphetamine Extended-Release Capsules (FDA)
- Dextroamphetamine Oral Solution (FDA)
Other brands
Dexedrine, Zenzedi, Xelstrym, Dextrostat, ProCentra