Glyburide (Monograph)
Brand name: Glynase
Drug class: Sulfonylureas
Introduction
Antidiabetic agent; sulfonylurea.1 3 4
Uses for Glyburide
Type 2 Diabetes Mellitus
Used as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus.1 3 4 49 50 51 52 53 54 55 56 57 58 158
Used as monotherapy or in combination with one or more other oral antidiabetic agents or insulin as an adjunct to diet and exercise in patients who do not achieve adequate glycemic control with diet, exercise, and oral antidiabetic agent monotherapy.1 124 158 162 165 166 169 170 195 198 200 201 202 203 707 708
Commercially available as a single entity preparation and in fixed combination with metformin hydrochloride.1 124 158
Guidelines from the American Diabetes Association (ADA) and other experts generally recommend that use of sulfonylureas for the treatment of type 2 diabetes mellitus be limited or discontinued due to increased risk of weight gain and hypoglycemia.707 708 Sulfonylureas may be considered in patients with access or cost barriers to other antidiabetic regimens.707 708 When used, these guidelines recommend the lowest possible dosage.707 708 When selecting a treatment regimen for diabetes, consider factors such as cardiovascular and renal comorbidities, drug efficacy and adverse effects, hypoglycemia risk, presence of overweight or obesity, cost, access, and patient preferences.707 708 Weight management should be included as a distinct treatment goal and other healthy lifestyle behaviors should also be considered.707 708
Should notbe used for type 1 diabetes mellitus or diabetic ketoacidosis; such use contraindicated.1 124
Glyburide Dosage and Administration
General
Patient Monitoring
-
Monitor with regular clinical and laboratory evaluations, including blood and/or urine glucose determinations, to determine the minimum effective dosage and to detect primary failure (inadequate lowering of blood glucose concentration at maximum recommended dosage) or secondary failure (loss of control of blood glucose concentration following an initial period of effectiveness ) to the drug.1 124
-
Periodic HbA1cdeterminations are the principal means of assessing long-term glycemic control.1 124 158 Following initiation of therapy, determination of HbA1c at intervals of approximately 3 months is useful for assessing continued response to therapy.707 708
Dispensing and Administration Precautions
-
Based on the Institute for Safe Medication Practices (ISMP), glyburide is a high-alert medication that has a heightened risk of causing significant patient harm when used in error.709
-
The ISMP includes glyBURIDE and glipiZIDE on the ISMP List of Confused Drug Names, and recommends special safeguards to ensure the accuracy of prescriptions for these drugs.710
-
The 2023 American Geriatrics Society (AGS) Beers Criteria for Potentially Inappropriate Medication (PIM) Use in Older Adults includes all sulfonylureas on the list of PIMs that are best avoided by older adults in most circumstances or under specific situations, such as certain diseases, conditions, or care settings.999 The criteria are intended to apply to adults ≥65 years of age in all ambulatory, acute, and institutional settings of care, except hospice and end-of-life care settings.999 The Beers Criteria Expert Panel specifically recommends to avoid sulfonylureas as first- or second-line monotherapy or add-on therapy unless there are substantial barriers to the use of safer and more effective agents; if a sulfonylurea is used, choose short-acting agents (e.g., glipizide) over long-acting agents (e.g., glyburide, glimepiride).999
Administration
Oral Administration
Administer conventional or micronized formulations once daily with breakfast or first main meal.1 3 124 May administer in 2 divided doses in some patients (i.e., those receiving >10 mg daily [as conventional formulations]1 or >6 mg daily [as micronized glyburide]).124
Micronized formulations arenotbioequivalent with conventional formulations; retitrate dosage when transferring patients from micronized to conventional formulations, or vice versa.124
Patients who do not adhere to prescribed dietary and drug regimens are more likely to have unsatisfactory response to therapy.1 124 In patients usually well controlled by dietary management alone, short-term therapy may be sufficient during periods of transient loss of glycemic control.1 124
Administer fixed combination with metformin hydrochloride once or twice daily with meals.158 See full prescribing information for additional administration instructions.158
Administer glyburide at least 4 hours prior to colesevelam when drugs given concomitantly.1 124
Dosage
Adults
Type 2 Diabetes Mellitus
Initial Dosage in Previously Untreated Patients
OralConventional formulations: Initially, 2.5–5 mg daily.1
Micronized formulations: Initially, 1.5 –3 mg daily.124
Fixed combination with metformin hydrochloride: Initially, 1.25 mg of glyburide and 250 mg of metformin hydrochloride once or twice daily.158
Initial Dosage in Patients Transferred from Other Oral Antidiabetic Agents
OralConventional formulations: Initially, 2.5–5 mg daily.1
Micronized formulations: Initially, 1.5–3 mg daily.124
May discontinue most other oral hypoglycemic agents immediately.1 3 124 Initial or loading dose of glyburide is notnecessary.1 124
Fixed combination with metformin hydrochloride: Initially, glyburide 2.5 mg/metformin hydrochloride 500 mg or glyburide 5 mg/metformin hydrochloride 500 mg twice daily in patients not adequately controlled on monotherapy with glyburide (or another sulfonylurea) or metformin.158 For patients previously receiving combination therapy with glyburide (or another sulfonylurea) and metformin, initial dosage should not exceed previous individual dosages of glyburide (or equivalent dosage of another sulfonylurea) and metformin.158
Initial Dosage in Patients Transferred from Insulin
OralConventional formulations: Initially, 2.5–5 mg once daily (if insulin dosage is <20 units daily) or 5 mg once daily (if insulin dosage is 20–40 units daily); may discontinue insulin immediately.1 If insulin dosage is >40 units daily, reduce insulin dosage by 50% and initiate glyburide at 5 mg daily; withdraw insulin gradually and increase glyburide dosage in increments of 1.25–2.5 mg daily every 2–10 days.1
Micronized formulations: Initially, 1.5–3 mg once daily (if insulin dosage is <20 units daily) or 3 mg once daily (if insulin dosage is 20–40 units daily); may discontinue insulin immediately.124 If insulin dosage is >40 units daily, reduce insulin dosage by 50% and initiate glyburide at 3 mg daily; withdraw insulin gradually and increase glyburide dosage in increments of 0.75–1.5 mg daily every 2–10 days.124
Titration and Maintenance Dosage
OralConventional formulations: Increase dosage in increments of ≤2.5 mg at weekly intervals.1 Usual maintenance dosage is 1.25–20 mg daily.1 Maximum recommended dosage is 20 mg daily.1
Micronized formulations: Increase dosage in increments of ≤1.5 mg at weekly intervals.124 Usual maintenance dosage is 0.75–12 mg daily.124 Maximum recommended dosage is 12 mg daily.124
Fixed combination with metformin hydrochloride: Titrate dosage gradually based on glycemic control and tolerability up to a maximum daily dosage of 20 mg of glyburide and 2 g of metformin hydrochloride.158
Special Populations
Hepatic Impairment
Conventional formulations: Initially, 1.25 mg daily.1 Dosage should be conservative to avoid hypoglycemic reactions.1
Micronized formulations: Initially, 0.75 mg daily.124 Dosage should be conservative to avoid hypoglycemic reactions.124
Fixed combination with metformin hydrochloride: Use not recommended.158
Renal Impairment
Conventional formulations: Initially, 1.25 mg daily.1 Dosage should be conservative to avoid hypoglycemic reactions.1
Micronized formulations: Initially, 0.75 mg daily.124 Dosage should be conservative to avoid hypoglycemic reactions.124
Fixed combination with metformin hydrochloride: Do not initiate if eGFR 30—45 mL/minute per 1.73 m2.158 In patients already taking and eGFR falls below 45 mL/minute per 1.73 m2, assess benefits and risks of continuing therapy.158 Discontinue if eGFR <30 mL/minute per 1.73 m2.158
Geriatric Patients
Conventional formulations: Initially, 1.25 mg daily1
Micronized formulations: Initially, 0.75 mg daily.124
Fixed combination with metformin hydrochloride: Use a lower dosage when initiating or increasing therapy.158
Other Special Populations
Cautious dosing recommended in debilitated or malnourished patients or in patients with adrenal or pituitary insufficiency.1 124 158
Conventional formulations: Initially, 1.25 mg daily1
Micronized formulations: Initially, 0.75 mg daily.124
Cautions for Glyburide
Contraindications
-
Known hypersensitivity to glyburide or any ingredient in the formulation.1 124
-
Diabetic ketoacidosis with or without coma.1 124 Diabetic ketoacidosis should be treated with insulin.1 124
Warnings/Precautions
Increased Risk of Cardiovascular Mortality
Administration of oral antidiabetic agents reported to be associated with increased cardiovascular mortality compared to treatment with diet alone or diet with insulin therapy.1 124 158
Warning based on study conducted by University Group Diabetes Program (UGDP), a long-term prospective clinical trial that reported patients treated for 5—8 years with tolbutamide (1.5 g per day) had a rate of cardiovascular mortality 2.5 times that of patients treated with diet alone.1 63 124 Results of the UGDP study have been exhaustively analyzed; there has been general disagreement in scientific and medical communities regarding study's validity and clinical importance.61 62 63
Although only one drug in the sulfonylurea class (tolbutamide) was included in the UGDP study, it is prudent from a safety standpoint to consider that this warning may also apply to other oral antidiabetic drugs in this class, in view of their close similarities in mode of action and chemical structure.1 124
Inform patients of potential risk and advantages of glyburide and alternative therapies.1 124
Macrovascular Outcomes
Manufacturer states that no clinical studies have conclusively established macrovascular risk reduction with glyburide or any other antidiabetic drug.1 124
Hypoglycemia
Severe,1 67 68 69 74 105 124 occasionally fatal,67 68 74 105 hypoglycemia reported. Debilitated, malnourished, or geriatric patients and patients with renal or hepatic impairment or adrenal or pituitary insufficiency may be particularly susceptible.1 105 124 158 Strenuous exercise, alcohol ingestion, insufficient caloric intake, or use in combination with other antidiabetic agents may increase risk.1 105 124 Hypoglycemia may be difficult to recognize in geriatric patients or in those receiving β-adrenergic blocking agents.1 105 124 158
Appropriate patient selection and careful attention to dosage are important to avoid glyburide-induced hypoglycemia.1 67 124
Risks, symptoms, and treatment of hypoglycemia, as well as conditions that predispose to its development, should be explained to patients and responsible family members.1 124
Loss of Glycemic Control
Possible loss of glycemic control during periods of stress (e.g., fever, trauma, infection, surgery).1 124 Temporary discontinuance of glyburide and administration of insulin may be required.1 124
Effectiveness of any antidiabetic agent, including glyburide, in lowering blood glucose to desirable level decreases in many patients over time which may be due to progression of disease severity or to diminished responsiveness to drug.1 124 Adequate dosage adjustment and adherence to dietary recommendations should be assessed before classifying patient as experiencing secondary failure to glyburide.1 124
Hemolytic Anemia
Hemolytic anemia may develop in patients with glucose 6-phosphate dehydrogenase (G6PD) deficiency who receive sulfonylureas; consider a nonsulfonylurea antidiabetic agent in patients with G6PD deficiency.1 124 158 Hemolytic anemia also reported in patients receiving glyburide who did not have known G6PD deficiency.1 124 158
Use in Fixed Combinations
When used in fixed combination with metformin hydrochloride, consider the cautions, precautions, and contraindications associated with metformin.158
Specific Populations
Pregnancy
Insufficient evidence to evaluate drug-associated risk of adverse outcomes.1 124 Reproduction studies in animals have not revealed evidence of harm.1 124
Abnormal maternal blood glucose concentrations may be associated with higher incidence of congenital abnormalities; however, use of glyburide in pregnant women is generally not recommended.1 124 Many experts recommend that insulin be used during pregnancy.1 124
Prolonged, severe hypoglycemia lasting 4—10 days reported in some neonates born to women receiving other sulfonylurea antidiabetic agents up to time of delivery.1 124 To minimize risk of neonatal hypoglycemia if glyburide used during pregnancy, manufacturer recommends drug be discontinued at least 2 weeks before expected delivery date.1 124
Lactation
Not known whether glyburide is distributed into human milk; discontinue nursing or the drug.1 124
Females and Males of Reproductive Potential
Reproduction studies in rats and rabbits have not revealed evidence of impaired fertility.1 124
Pediatric Use
Safety and efficacy not established.1 124
Geriatric Use
Increased risk of hypoglycemia; hypoglycemia may be difficult to recognize.1 105 124 Cautious dosing recommended.1 124 158
Hepatic Impairment
Increased risk of hypoglycemia.1 105 124 Cautious dosing recommended.1 124 158
Renal Impairment
Increased risk of hypoglycemia.1 105 124 Cautious dosing recommended.1 124 158
Common Adverse Effects
With conventional and micronized formulations: nausea, epigastric fullness, heartburn.1 3 62
With fixed-combination glyburide/metformin hydrochloride: diarrhea, headache, nausea/vomiting, abdominal pain, dizziness.158
Drug Interactions
When using fixed-combination preparation containing metformin hydrochloride, also consider the drug interactions associated with metformin.158
Drugs Affecting Hepatic Microsomal Enzymes
Glyburide principally metabolized by CYP2C9.711 712 Consider potential interactions with CYP2C9 inducers or inhibitors.711 712
Protein-bound Drugs
Potential pharmacokinetic interaction and possible potentiation of hypoglycemic effects when used concomitantly with other highly protein-bound drugs.1 37 38 39 40 60 62 124
Observe for adverse effects when glyburide therapy is initiated or discontinued and vice versa.1 124
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Observe carefully for glycemic effects or loss of glycemic control when an ACE inhibitor is initiated or discontinued37 38 39 40 62 |
|
|
Alcohol |
Possible rare disulfiram-like reactions87 |
|
|
Anticoagulants, oral (e.g., coumarins) |
Possible displacement from plasma proteins and potentiation of hypoglycemic effects1 37 38 39 40 62 124 |
Observe carefully for adverse effects when oral anticoagulants are initiated or discontinued1 124 |
|
Antifungal agents, azole (i.e., fluconazole, miconazole) |
Increased glyburide concentrations; possible hypoglycemia1 124 158 211 |
|
|
β-Adrenergic blocking agents |
Impaired glucose tolerance60 62 or potentiation of hypoglycemic effects60 62 |
If concomitant therapy is necessary, a β1-selective adrenergic blocking agent may be preferred62 |
|
Bosentan |
Increased risk of elevated serum aminotransferase concentrations233 |
|
|
Calcium-channel blocking agents |
Observe carefully for loss of glycemic control or for hypoglycemia when calcium-channel blocking agents are initiated or discontinued1 124 158 |
|
|
Chloramphenicol |
Observe carefully for glycemic effects or loss of glycemic control when chloramphenicol is initiated or discontinued1 124 158 |
|
|
Clarithromycin |
Observe carefully for glycemic effects or loss of glycemic control when clarithromycin is initiated or discontinued37 38 39 40 62 |
|
|
Colesevelam |
Reductions in glyburide AUC and peak plasma concentration with concomitant administration1 124 |
|
|
Contraceptives, oral |
Observe carefully for loss of glycemic control when oral contraceptives are initiated or discontinued1 124 158 |
|
|
Corticosteroids |
Observe carefully for loss of glycemic control when corticosteroids are initiated or discontinued1 124 158 |
|
|
Disopyramide |
Observe carefully for glycemic effects or loss of glycemic control when disopyramide is initiated or discontinued37 38 39 40 62 |
|
|
Diuretics (e.g., thiazides) |
Observe carefully for loss of glycemic control when diuretics are initiated or discontinued1 124 158 |
|
|
Estrogens |
Observe carefully for loss of glycemic control when estrogens are initiated or discontinued1 124 158 |
|
|
Fluoroquinolone anti-infectives (e.g., ciprofloxacin) |
Observe carefully for glycemic effects or loss of glycemic control when fluoroquinolone anti-infectives are initiated or discontinued1 124 158 |
|
|
Fluoxetine |
Observe carefully for glycemic effects or loss of glycemic control when fluoxetine is initiated or discontinued37 38 39 40 62 |
|
|
Hydantoins |
Possible displacement from plasma protein and potentiation of hypoglycemic effects37 38 39 40 62 |
|
|
Isoniazid |
Observe carefully for loss of glycemic control when isoniazid is initiated or discontinued1 124 158 |
|
|
MAO inhibitors |
Observe closely for glycemic effects or loss of glycemic control when MAO inhibitors are initiated or discontinued1 124 158 |
|
|
Metformin |
Highly variable decreases in AUC and peak plasma concentrations of glyburide (certain preparations) with concomitant single-dose metformin in patients with type 2 diabetes mellitus; no changes in metformin pharmacokinetics or pharmacodynamics1 124 |
|
|
Niacin |
Observe carefully for loss of glycemic control when niacin is initiated or discontinued1 124 158 |
|
|
NSAIAs |
Possible displacement from plasma proteins and potentiation of hypoglycemic effects1 37 38 39 40 62 124 |
Observe carefully for loss of glycemic control when NSAIAs are initiated or discontinued1 124 |
|
Phenothiazines |
Observe carefully for loss of glycemic control when phenothiazines are initiated or discontinued1 124 158 |
|
|
Phenytoin |
Observe carefully for loss of glycemic control when phenytoin is initiated or discontinued1 124 158 |
|
|
Probenecid |
Observe closely for loss of glycemic control when probenecid is initiated or discontinued1 124 158 |
|
|
Rifampin |
May exacerbate diabetes mellitus62 |
Observe carefully for loss of glycemic control when rifampin is initiated or discontinued1 124 158 |
|
Sulfonamides |
Possible displacement from plasma proteins and potentiation of hypoglycemic effects1 37 38 39 40 62 124 |
Observe carefully for adverse effects when sulfonamides are initiated or discontinued1 124 |
|
Sympathomimetic agents |
Observe carefully for loss of glycemic control when sympathomimetic agents are initiated or discontinued1 124 158 |
|
|
Thyroid agents |
Observe carefully for loss of glycemic control when thyroid agents are initiated or discontinued1 124 158 |
|
|
Topiramate |
Reductions in AUC and peak plasma concentrations of glyburide and active metabolites 4-trans-hydroxyglyburide (M1) and 3-cis hydroxyglyburide (M2)1 124 |
Glyburide Pharmacokinetics
Absorption
Bioavailability
Almost completely absorbed following oral administration.4 23 24
Conventional and micronized glyburide preparations not bioequivalent.124
Onset
Hypoglycemic action generally begins within 45–60 minutes and is maximal within 1.5–3 hours.4 27 32 49
Duration
In single-dose studies in fasting healthy individuals, the degree and duration of blood-glucose lowering is proportional to glyburide dose and AUC.1 124
In nonfasting diabetic patients, the hypoglycemic action may persist for up to 24 hours.1 33 124
Food
Food does not affect rate or extent of absorption.27 28
Special Populations
In patients with renal1 27 124 or hepatic1 124 impairment, serum concentrations may be increased.
Distribution
Extent
Distributed in substantial amounts into bile.1 3 25 26 36 124
Appears to cross the placenta.81 Not known if distributed into breast milk.1 124
Plasma Protein Binding
>97% (for major metabolite 4-trans-hydroxyglyburide).25
Elimination
Metabolism
Appears to be completely metabolized, 25 26 31 36 probably in the liver.31
Elimination Route
Excreted as metabolites in urine and feces in approximately equal proportions.1 23 25 26 30 31 47 124
Minimally removed by hemodialysis.42
Half-life
1.4–1.8 hours (for glyburide)24 27 29 41 97 or approximately 10 hours (for glyburide and metabolites).25 30 31 32 124
Special Populations
In patients with severe renal impairment, clearance may be decreased and half-life prolonged.42 43
Stability
Storage
Oral
Conventional or Micronized Preparations
Store at 20–25°C in tightly closed container; consult specific labeling.1 124
Actions
-
Stimulates secretion of endogenous insulin from beta cells of the pancreas.1 3 4 8 9 10 11 12 Lowers blood glucose concentration in diabetic and nondiabetic individuals.3 4 8 9 10 11
-
During prolonged administration, extrapancreatic effects (e.g., enhanced peripheral sensitivity to insulin, reduction of basal hepatic glucose production) contribute to the hypoglycemic action.4 8 9 10 11 12 15 16 17 110 111 112 121
Advice to Patients
-
Advise patients of the potential risks and advantages of glyburide and of alternative therapy.1
-
Inform patients of the importance of regular clinical and laboratory evaluations, including urine and/or fasting blood glucose determinations.1 124
-
Advise patients of the importance of adhering to dietary instructions and regular physical activity.1 124
-
Inform patients and responsible family members of the risk of hypoglycemia, the symptoms and treatment of hypoglycemic reactions, and conditions that predispose to the development of hypoglycemic reactions.1
-
Inform patients of primary and secondary failure to oral sulfonylurea antidiabetic agents.1
-
When glyburide is used in fixed combination with other drugs (i.e., metformin hydrochloride), inform patients of other important cautionary information about the concomitant agent(s).1 124 158
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.1
-
Advise patients to inform their clinician if they are or plan to become pregnant or plan to breast-feed.1
-
Inform patients of other important precautionary information.1
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
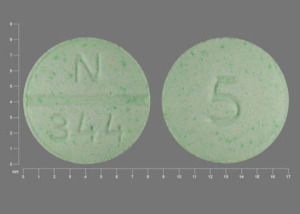
Oral |
Tablets |
1.25 mg* |
glyBURIDE Tablets |
|
|
2.5 mg* |
glyBURIDE Tablets |
|||
|
5 mg* |
glyBURIDE Tablets |
|||
|
Tablets (micronized) |
1.5 mg* |
glyBURIDE Micronized Tablets |
||
|
Glynase PresTab (scored) |
Pfizer |
|||
|
3 mg* |
glyBURIDE Micronized Tablets |
|||
|
Glynase PresTab (scored) |
Pfizer |
|||
|
6 mg* |
glyBURIDE Micronized Tablets |
|||
|
Glynase PresTab (scored) |
Pfizer |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
1.25 mg with Metformin Hydrochloride 250 mg* |
Glyburide with Metformin Hydrochloride Tablets |
|
|
2.5 mg with Metformin Hydrochloride 500 mg* |
Glyburide with Metformin Hydrochloride Tablets |
|||
|
5 mg with Metformin Hydrochloride 500 mg* |
Glyburide with Metformin Hydrochloride Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Avet Pharmaceuticals Inc. Glyburide tablets prescribing information. East Brunswick, NJ; 2024 Jul.
3. Anon. Glibenclamide: a review. Drugs. 1971; 1:116-40. https://pubmed.ncbi.nlm.nih.gov/5004340
4. Jackson JE, Bressler R. Clinical pharmacology of sulphonylurea hypoglycaemic agents: part 1. Drugs. 1981; 22:211-45. https://pubmed.ncbi.nlm.nih.gov/7021124
7. Hadju VP, Kohler KF, Schmidt FH et al. Physikalisch-chemische und analytische Unter suchungen an HB 419. (German; with English abstract) Arzneim-Forsch. 1969; 19:1381-6.
8. Skillman TG, Feldman JM. The pharmacology of sulfonylureas. Am J Med. 1981; 70:361-72. https://pubmed.ncbi.nlm.nih.gov/6781341
9. Kolterman OG, Gray RS, Shapiro G et al. The acute and chronic effects of sulfonylurea therapy in type II diabetic subjects. Diabetes. 1984; 33:346-54. https://pubmed.ncbi.nlm.nih.gov/6423429
10. Duckworth WC, Solomon SS, Kitabchi AE. Effect of chronic sulfonylurea therapy on plasma insulin and proinsulin levels. J Clin Endocrinol Metab. 1972; 35:585-91. https://pubmed.ncbi.nlm.nih.gov/5052977
11. Feldman JM, Lebovitz HE. Endocrine and metabolic effects of glybenclamide: evidence for an extrapancreatic mechanism of action. Diabetes. 1971; 20:745-55.
12. DeFronzo RA, Ferrannini E, Koivisto V. New concepts in the pathogenesis and treatment of noninsulin-dependent diabetes mellitus. Am J Med. 1983; 74(Suppl 1A):52-81. https://pubmed.ncbi.nlm.nih.gov/6337486
13. Lockwood DH, Maloff BL, Nowak SM et al. Extrapancreatic effects of sulfonylureas: potentiation of insulin action through post-binding mechanisms. Am J Med. 1983; 74(Suppl 1A):102-8. https://pubmed.ncbi.nlm.nih.gov/6401922
14. Brogden RN, Heel RC, Pakes GE et al. Glipizide: a review of its pharmacological properties and therapeutic use. Drugs. 1979; 18:329-53. https://pubmed.ncbi.nlm.nih.gov/389600
15. Kolterman OG, Prince MJ, Olefsky JM. Insulin resistance in noninsulin-dependent diabetes mellitus: impact of sulfonylurea agents in vivo and in vitro. Am J Med. 1983; 74(Suppl 1A):82-101. https://pubmed.ncbi.nlm.nih.gov/6401923
16. Beck-Nielsen H, Pedersen O, Lindskov HO. Increased insulin sensitivity and cellular insulin binding in obese diabetics following treatment with glibenclamide. Acta Endocrinol. 1979; 90:451-62. https://pubmed.ncbi.nlm.nih.gov/106617
17. Hjollund E, Richelsen B, Beck-Nielsen H et al. The effect of glibenclamide on insulin receptors in normal man: comparative studies of insulin binding to monocytes and erythrocytes. J Clin Endocrinol Metab. 1983; 57:1257-62. https://pubmed.ncbi.nlm.nih.gov/6415086
18. Moses AM, Howanitz J, Miller M. Diuretic action of three sulfonylurea drugs. Ann Intern Med. 1973; 78:541-4. https://pubmed.ncbi.nlm.nih.gov/4632790
19. Rado JP, Borbély L, Szende L et al. Investigation of the diuretic effect of glibenclamide in healthy subjects and in patients with pituitary and nephrogenic diabetes insipidus. Horm Metab Res. 1974; 6:289-92. https://pubmed.ncbi.nlm.nih.gov/4213198
20. Rado JP, Szende L. Inhibition of clofibrate-induced antidiuresis by glybenclamide in patients with pituitary diabetes insipidus. J Clin Pharmacol. 1974; 14:290-5. https://pubmed.ncbi.nlm.nih.gov/4208361
23. Rupp W, Christ O, Fulberth W. Untersuchungen zur Bioavailability von Glibenclamid. (German; with English abstract) Arzneim-Forsch. 1972; 22:471-3.
24. Ings RMJ, Lawrence JR, McDonald A et al. Glibenclamide pharmacokinetics in healthy volunteers: evidence for zero-order drug absorption. Br J Clin Pharmacol. 1982; 13:264-5P.
25. Christ OE, Heptner W, Rupp W. Investigations on absorption, excretion and metabolism in man after administration of14C-labelled HB 419. Horm Metab Res Suppl Ser. 1969; 1:51-4.
26. Rupp VW, Christ O, Heptner W. Resorption, Ausscheidung and Metabolismus nach intravenoser und oraler Gabe von HB 419-14C an Menschen. (German; with English abstract) Arzneim-Forsch. 1969; 19:1428-34.
27. Sartor G, Melander A, Scherstén B et al. Serum glibenclamide in diabetic patients, and influence of food on the kinetics and effects of glibenclamide. Diabetologia. 1980; 18:17-22. https://pubmed.ncbi.nlm.nih.gov/6767639
28. Sartor G, Lundquist I, Melander A et al. Improved effect of glibenclamide on administration before breakfast. Eur J Clin Pharmacol. 1982; 21:403-8. https://pubmed.ncbi.nlm.nih.gov/6804245
29. Sartor G, Melander A, Scherstén B et al. Comparative single-dose kinetics and effects of four sulfonylureas in healthy volunteers. Acta Med Scand. 1980; 208:301-7. https://pubmed.ncbi.nlm.nih.gov/6778079
30. Fucella LM, Tamassia V, Valzelli G. Metabolism and kinetics of the hypoglycemic agent glipizide in man—comparison with glibenclamide. J Clin Pharmacol. 1973; 13:68-75.
31. Balant L, Fabre J, Zahnd GR. Comparison of the pharmacokinetics of glipizide and glibenclamide in man. Eur J Clin Pharmacol. 1975; 8:63-9. https://pubmed.ncbi.nlm.nih.gov/823030
32. Ko H, Royer ME, Molony BA. Relationships between circulating glyburide/metabolite concentrations, serum glucose lowering, and dose of glyburide in man. In: Rifkin H, ed. Micronase (glyburide): pharmacological and clinical evaluation. Amsterdam: Excerpta Medica; 1975:20-30.
33. Groop L, Harno K. Diurnal pattern of plasma insulin and blood glucose during glibenclamide and glipizide therapy in elderly diabetics. Acta Endocrinol Suppl. 1980; 239:44-52.
34. Balant L, Zahnd GR, Weber F et al. Behaviour of glibenclamide on repeated administration to diabetic patients. Eur J Clin Pharmacol. 1977; 11:19-25. https://pubmed.ncbi.nlm.nih.gov/401739
36. Kaiser DG, Forist AA. A review of glyburide metabolism in man and laboratory animals. In: Rifkin H, ed. Micronase (glyburide): pharmacological and clinical evaluation. Amsterdam: Excerpta Medica; 1975:31-43.
37. Crooks MJ, Brown KF. The binding of sulphonylureas to serum albumin. J Pharm Pharmacol. 1974; 26:304-11. https://pubmed.ncbi.nlm.nih.gov/4153105
38. Hsu P, Ma JKH, Luzzi LA. Interactions of sulfonylureas with plasma proteins. J Pharm Sci. 1974; 63:570-3. https://pubmed.ncbi.nlm.nih.gov/4208196
39. Brown KF, Crooks MJ. Binding of sulfonylureas to serum albumin. II. The influence of salt and buffer compositions on tolbutamide and glyburide. Can J Pharm Sci. 1974; 9:75-7.
40. Brown KF, Crooks MJ. Displacement of tolbutamide, glibenclamide and chlorpropramide from serum albumin by anionic drugs. Biochem Pharmacol. 1976; 25:1175-8. https://pubmed.ncbi.nlm.nih.gov/820348
41. Morrison PJ, Rogers HJ, Spector RG et al. Effect of pirprofen on glibenclamide kinetics and response. Br J Clin Pharmacol. 1982; 14:123-6. https://pubmed.ncbi.nlm.nih.gov/6809024
42. Raehl CL, Goersch WA, Craig WA et al. The pharmacokinetics of14C-glyburide (Micronase) in patients with reduced renal function. In: Official Program and Abstracts of Papers presented before the APhA Academy of Pharmaceutical Sciences. Washington, DC: American Pharmaceutical Association; 1983; 13(2):205. Abstract.
43. Balant L, Zahnd G, Petitpierre B et al. Influence of renal failure on the pharmacokinetics and hypoglycemic effect of sulfonylureas. Diabetologia. 1973; 9:59.
44. Balant L, Fabre J, Loutan L et al. Does 4-trans-hydroxy-glibenclamide show hypoglycemic activity? Arzneim-Forsch. 1979; 29:162-3.
45. Rado JP, Borbély L. Inhibition of the antidiuretic effect of 1-deamino-8d-arginine vasopressin (DDAVP) by glibenclamide in water-loaded healthy subjects. Endokrinologie. 1975; 66:88-93. https://pubmed.ncbi.nlm.nih.gov/817889
46. Rado JP, Szende L, Marosi J. Influence of glyburide on the antidiuretic response induced by 1-deamino-8-d-arginine vasopressin (DDAVP) in patients with pituitary diabetes insipidus. Metabolism. 1974; 23:1057-63. https://pubmed.ncbi.nlm.nih.gov/4214480
47. Anderson J, Stephenson RJ, Tomlinson RWS et al. Studies with14C-labelled glibenclamide. Postguard Med J. 1970; 46(Dec Suppl):42-5.
48. Larner J. Mediators of postreceptor action of insulin. Am J Med. 1983; 74(Suppl 1A):38-51. https://pubmed.ncbi.nlm.nih.gov/6297300
49. Davidson M, Lewis AAG, de Mowbray RR. Metabolic and clinical effects of glibenclamide. Lancet. 1970; 1:57-61. https://pubmed.ncbi.nlm.nih.gov/4188623
50. Johnson BF, Bhatia CK, Rzeszotarski WJ et al. Preliminary clinical evaluation of glybenclamide in treatment of diabetes mellitus. Diabetes. 1970; 19:579-84. https://pubmed.ncbi.nlm.nih.gov/4915447
51. Clarke BF, Campbell IW. Long-term comparative trial of glibenclamide and chlorpropamide in diet-failed, maturity-onset diabetics. Lancet. 1975; 1:246-8. https://pubmed.ncbi.nlm.nih.gov/8667857
52. Hamblin JJ, Ismay G, Good MS et al. A comparative study of glibenclamide and chlorpropamide (preliminary report). Postgrad Med J. 1970; 46(Dec Suppl):92-4. https://pubmed.ncbi.nlm.nih.gov/5416512
53. Mogensen EF, Worm J, Mikkelsen BO. Clinical comparison between glibornuride (Glutril) and glibenclamide in maturity-onset diabetes: a controlled double-blind trial. Curr Ther Res. 1976; 19:599-64.
54. Blohmé G, Waldenstrom J. Glibenclamide and glipizide in maturity onset diabetes. Acta Med Scand. 1979; 206:263-7. https://pubmed.ncbi.nlm.nih.gov/116480
55. Frederiksen PK, Mogensen EF. A clinical comparison between glipizide (Glibenese) and glibenclamide (Daonil) in the treatment of maturity onset diabetes: a controlled doudle-blind cross-over study. Curr Ther Res. 1982; 32:1-7.
56. Allen GS. The comparative effectiveness of glyburide and tolazamide in patients with mild diabetes. In: Rifkin H, ed. Micronase (glyburide): pharmacological and clinical evaluation. Amsterdam: Excerpta Medica; 1975:150-6.
57. Bryan JB, Inchaustegui HJ. Clinical impressions of Micronase (glyburide) in a private practice. In: Rifkin H, ed. Micronase (glyburide): pharmacological and clinical evaluation. Amsterdam: Excerpta Medica; 1975:225-34.
58. Murphey AT, Peskin H. Glyburide compared to previous therapy or tolbutamide. In: Rifkin H, ed. Micronase (glyburide): pharmacological and clinical evaluation. Amsterdam: Excerpta Medica; 1975:204-10.
60. Koda-Kimble MA. Diabetes mellitus. In: Koda-Kimble MA, Young LY, eds. Applied therapeutics: the clinical use of drugs. 5th ed. Vancouver, WA: Applied Therapeutics, Inc.; 1992:72–1-53.
61. Scientific Advisory Panel of the Executive Committee, American Diabetes Association. Policy statement: the UGDP controversy. Diabetes. 1979; 28:168-70.
62. Jackson JE, Bressler R. Clinical pharmacology of sulphonylurea hypoglycaemic agents: part 2. Drugs. 1981; 22:295-320. https://pubmed.ncbi.nlm.nih.gov/7030708
63. Food and Drug Administration. Labeling for oral hypoglycemic drugs of the sulfonylurea class. [Docket No. 75N-0062] Fed Regist. 1984; 49:14303-31.
66. Krans HMJ. Insulin, glucagon and oral hypoglycaemic drugs. In: Dukes MNG, ed. Side effects of drugs. Annual 2. New York: Elsevier/North Holland Inc; 1978:345.
67. Seltzer HS. Severe drug-induced hypoglycemia: a review. Compr Ther. 1979; 5(4):21-9. https://pubmed.ncbi.nlm.nih.gov/445986
68. Gottesburen H, Gerdes H, Littman KP et al. Severe hypoglycemia after glibenclamide. Lancet. 1970; 2:576.
69. Howard FM. Hypoglycemia in diabetics treated with Micronase (glyburide). In: Rifkin H, ed. Micronase (glyburide): pharmacological and clinical evaluation. Amsterdam: Excerpta Medica: 1975:164-71.
70. Krans HMJ. Insulin, glucagon and oral hypoglycaemic drugs. In: Dukes MNG, ed. Side effects of drugs. Annual 1. New York: Elsevier/North Holland Inc; 1977:319.
71. Sillence DO, Court JM. Glibenclamide-induced hypoglycaemia. Br Med J. 1975; 3:490-1. https://pubmed.ncbi.nlm.nih.gov/808247
72. Kullavanijaya P. Recovery from overdose with glibenclamide. Br Med J. 1970; 4:53-4. https://pubmed.ncbi.nlm.nih.gov/5470446
73. Krans HMJ. Insulin, glucagon and oral hypoglycaemic drugs. In: Dukes MNG, ed. Side effects of drugs. Annual 3. New York: Elsevier/North Holland Inc; 1979:347.
74. Krans HMJ. Insulin, glucagon and oral hypoglycaemic drugs. In: Dukes MNG, ed. Side effects of drugs. Annual 4. New York: Elsevier/North Holland Inc; 1980:303.
76. Krans HMJ. Insulin, glucagon and oral hypoglycaemic drugs. In: Dukes MNG, ed. Side effects of drugs. Annual 7. New York: Elsevier/North Holland Inc.; 1983:409.
77. Pannekoek JH. Insulin, glucagon and oral hypoglycaemic drugs. In: Dukes MNG, ed. Meyler’s side effects of drugs. 8th ed. Amsterdam: Excerpta Medica; 1975:914-5.
78. Sketris I, Wheeler D, York S. Hypoglycemic coma induced by inadvertent administration of glyburide. Drug Intell Clin Pharm. 1984; 18:142-3. https://pubmed.ncbi.nlm.nih.gov/6421558
79. Walfish PG, Kashyap RP, Greenstein S. Sulfonylurea-induced factitious hypoglycemia in a nondiabetic nurse. Can Med Assoc J. 1975; 112:71-2. https://pubmed.ncbi.nlm.nih.gov/803250
81. Coetzee EJ, Jackson WPU. Pregnancy in established non-insulin-dependent diabetics: a five-and-a-half year study at Groote Schuur Hospital. S Afr Med J. 1980; 58:795-802. https://pubmed.ncbi.nlm.nih.gov/6777880
87. Wardle EN, Richardson GO. Alcohol and glibenclamide. Br Med J. 1971; 3:309.
88. Zaman R, Kendall MJ, Biggs PI. The effect of acebutolol and propranolol on the hypoglycaemic action of glibenclamide. Br J Clin Pharmacol. 1982; 13:507-12. https://pubmed.ncbi.nlm.nih.gov/6802160
89. Hausmann L, Goebel KM. Atenolol in orally treated diabetic patients. Drugs. 1983; 25(Suppl 2):71-3.
90. De Marinis L, Barbarino A. Calcium antagonists and hormone release. I. Effects of verapamil on insulin release in normal subjects and patients with islet-cell tumor. Metabolism. 1980; 29:599-604. https://pubmed.ncbi.nlm.nih.gov/6247604
91. O’sullivan DJ, Cashman WF. Blood glucose variations and clinical experience with glibenclamide in diabetes mellitus. Br Med J. 1970; 2:572-4. https://pubmed.ncbi.nlm.nih.gov/5526612
92. Molony BA, Crim JA, Hearron AE Jr. Micronase (glyburide): a comparison of single and divided daily dose treatment schedules. In: Rifkin H, ed. Micronase (glyburide): pharmacological and clinical evaluation. Amsterdam: Excerpta Medica; 1975:248-53.
93. Owens DR, Wragg KG, Shetty KT et al. Glibenclamide, acute-long-term response in m.o. diabetics. Horm Metab Res. 1979; 11:411-2. https://pubmed.ncbi.nlm.nih.gov/112018
95. Huupponen R, Viikari J, Saarimaa H. Chlorpropamide and glibenclamide serum concentrations in hospitalized patients. Ann Clin Res. 1982; 14:119-22. https://pubmed.ncbi.nlm.nih.gov/6814340
97. Rogers HJ, Spector RG, Morrison PJ et al. Pharmacokinetics of intravenous glibenclamide investigated by a high performance liquid chromatographic assay. Diabetologia. 1982; 23:37-40. https://pubmed.ncbi.nlm.nih.gov/6811355
98. Fabre J, Balant L, Loutan L et al. Hypoglycemic activity of the main metabolite of glibenclamide: influence of renal insufficiency. Kidney Int. 1978; 13:435.
99. Loutan L, Samimi H, Balant L et al. Metabolites of hypoglycemic sulfonylureas in renal insufficiency. Experiences with glibenclamide. (German) Schweiz Med Wochenschr. 1978; 108:1782-6.
103. Lebovitz HE. Clinical utility of oral hypoglycemic agents in the management of patients with noninsulin-dependent diabetes mellitus. Am J Med. 1983; 75(Suppl 5B):94-9. https://pubmed.ncbi.nlm.nih.gov/6369972
105. Asplund K, Wiholm BE, Lithner F. Glibenclamide-associated hypoglycemia: a report on 57 cases. Diabetologia. 1983; 24:412-7. https://pubmed.ncbi.nlm.nih.gov/6411511
109. Kritz H, Najemnik C, Irsigler K. Sulfinpyrazone and glibenclamide study of interaction in diabetics of type II. Wien Med Wochenschr. 1983; 133:237-43. https://pubmed.ncbi.nlm.nih.gov/6408808
110. Best JD, Judzewitsch RG, Pfeifer MA et al. The effect of chronic sulfonylurea therapy on hepatic glucose production in non-insulin-dependent diabetes. Diabetes. 1982; 31:333-8. https://pubmed.ncbi.nlm.nih.gov/6759249
111. Pfeifer MA, Halter JB, Judzewitsch RG et al. Acute and chronic effects of sulfonylurea drugs on pancreatic islet function in man. Diabetes Care. 1984; 7(Suppl 1):25-34. https://pubmed.ncbi.nlm.nih.gov/6376026
112. DeFronzo RA, Simonson DC. Oral sulfonylurea agents suppress hepatic glucose production in non-insulin-dependent diabetic individuals. Diabetes Care. 1984; 7(Suppl 1):72-80. https://pubmed.ncbi.nlm.nih.gov/6428844
114. Asmal AC, Marble A. Oral hypoglycaemic agents: an update. Drugs. 1984; 28:62-78. https://pubmed.ncbi.nlm.nih.gov/6378583
116. Lotz N, Lacher F, Bachmann W. Combination of sulfonylureas (SU) and insulin (I) in the treatment of type-II-diabetes with “secondary failure” of SU-therapy (DSF). Diabetes. 1984; 33(Suppl 1):24A.
117. Simonson DC, Castellino P, Delprato S. Effect of glyburide on glucose control and metabolism in insulin treated diabetics. Diabetes. 1984; 33(Suppl 1):38A.
118. Rost CR, Brown JL. Combined insulin-sulfonylurea therapy in noninsulin-dependent diabetes mellitus (NIDDM). Diabetes. 1984; 33(Suppl 1):87A.
119. Groop L, Harno K, Nikkila EA et al. The combination of insulin and sulfonylurea (glibenclamide) in the treatment of non-insulin dependent diabetes poorly controlled with insulin alone: evaluation of its metabolic effects. Acta Endocrinol Suppl. 1983; 257:20.
120. Bachmann W, Sieger C, Haslbeck M et al. Combination of insulin and glibenclamide (gl) in the treatment of adult-onset diabetes (Type 2). Diabetologia. 1981; 21:245.
121. Simonson DC, Ferrannini E, Bevilacqua S et al. Mechanism of improvement in glucose metabolism after chronic glyburide therapy. Diabetes. 1984; 33:838-45. https://pubmed.ncbi.nlm.nih.gov/6432610
124. Pharmacia & Upjohn Company LLC. Glynase PresTab (micronized glyburide) tablets prescribing information. New York, NY; 2023 Aug.
127. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837-53. https://pubmed.ncbi.nlm.nih.gov/9742976
128. American Diabetes Association. Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care. 1999; 22(Suppl 1):S27-31.
129. Matthews DR, Cull CA, Stratton RR et al. UKPDS 26: sulphonylurea failure in non-insulin-dependent diabetic patients over 6 years. Diabet Med. 1998; 15:297-303. https://pubmed.ncbi.nlm.nih.gov/9585394
130. Genuth P. United Kingdom prospective diabetes study results are in. J Fam Pract. 1998; 47:(Suppl 5):S27.
131. Bretzel RG, Voit K, Schatz H et al. The United Kingdom Prospective Diabetes Study (UKPDS): implications for the pharmacotherapy of type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 1998; 106:369-72. https://pubmed.ncbi.nlm.nih.gov/9831300
132. Schmitt JK, Moore JR. Hypertension secondary to chlorpropamide with amelioration by changing to insulin. Am J Hypertens. 1993; 6:317-9. https://pubmed.ncbi.nlm.nih.gov/8507452
133. Genuth S, Brownless MA, Kuller LH et al. Consensus development conference on insulin resistance: Novermber 5-6 1997. Diabetes Care. 1998; 21:310-4. https://pubmed.ncbi.nlm.nih.gov/9540000
134. Henry RR. Glucose control and insulin resistance in non-insulin-dependent diabetes mellitus. Ann Intern Med. 1996; 124:97-103. https://pubmed.ncbi.nlm.nih.gov/8554221
136. Nathan DM. Some answers, more controversy, from UKDS. Lancet. 1998; 352:832-3. https://pubmed.ncbi.nlm.nih.gov/9742972
143. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metfromin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998; 352:854-65. https://pubmed.ncbi.nlm.nih.gov/9742977
144. American Diabetes Association. The United Kingdom Prosepective Diabetes Study (UKPDS) for type 2 diabetes: what you need to know about the results of a long-term study. Washington, DC; September 15, 1998. From American Diabetes Association web site. http://www.diabetes.org
146. Watkins PJ. UKPDS: a message of hope and a need for change. Diabet Med. 1998; 15:895-6. https://pubmed.ncbi.nlm.nih.gov/9827842
147. Turner RC, Cull CA, Frighi V et al. Glycemic control with diet, sulfonlyurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirements for multiple therapies (UKPDS 49). JAMA. 1999; 281:2005-12. https://pubmed.ncbi.nlm.nih.gov/10359389
149. American Diabetes Association. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2000; 23(Suppl 1):S4-19.
158. Avet Pharmaceuticals Inc. Glyburide and metformin hydrochloride tablets prescribing information. East Brunswick, NJ; 2024 Feb.
162. Williams G. Management of non-insulin-dependent diabetes mellitus. Lancet. 1994; 343:95-100. https://pubmed.ncbi.nlm.nih.gov/7903785
165. Chow CC, Sorensen JP, Tsang LWW et al. Comparison of insulin with or without continuation of oral hypoglycemic agents in the treatment of secondary failure in NIDDM patients. Diabetes Care. 1995; 18:307-14. https://pubmed.ncbi.nlm.nih.gov/7555472
166. Zimmerman B, Espenshade J, Fujimoto W et al. The pharmacological treatment of hyperglycemia in NIDDM. Diabetes Care. 1996; 19:1510-18.
167. Landstedt-Hallin L, Bolinder J, Adamson U et al. Comparison of bedtime NPH or preprandial regular insulin combined with glibenclamide in secondary sulfonylurea failure. Diabetes Care. 1995; 18:1183-6. https://pubmed.ncbi.nlm.nih.gov/7587856
169. Raskin P. Combination therapy in NIDDM N Engl J Med. 1992; 327:1453-4. Editorial.
170. Pugh JA, Ramirez G, Wagner ML et al. Is combination sulfonylurea and insulin therapy useful in NIDDM patients? A metaanalysis. Diabetes Care. 1992; 15:953-9. https://pubmed.ncbi.nlm.nih.gov/1387073
171. Buse J. Combining insulin and oral agents. Am J Med. 2000; 108(Suppl 6A):23S-32S. https://pubmed.ncbi.nlm.nih.gov/10764847
172. Johnson JL, Wolf SL, Kabadi UM. Efficacy of insulin and sulfonylurea combination therapy in type II diabetes: a meta-analysis of the randomized placebo-controlled trials. Arch Intern Med. 1996; 156:259-64. https://pubmed.ncbi.nlm.nih.gov/8572835
173. Yki-Jarvinen H, Dressler A, Ziemen M et al. Less nocturnal hypoglycemia and better post-dinner glucose control with bedtime insulin glargine compared with bedtime HPH insulin during insulin combination therapy in type 2 diabetes. Diabetes Care. 2000; 23:1130-6 (IDIS 451244) https://pubmed.ncbi.nlm.nih.gov/10937510
174. Trischitta V, Italia S, Mazzarino S et al. Comparison of combined therapies in treatment of secon dary failure to glyburide. Diabetes Care. 1992; 15:539-42. https://pubmed.ncbi.nlm.nih.gov/1499473
175. Florence JA, Yeager BF. Treatment of type 2 diabetes mellitus. Am Fam Physician. 1999; 59:2835-44. https://pubmed.ncbi.nlm.nih.gov/10348076
176. Bastyr EJ, Johnson ME, Trautman ME et al. Insulin lispro in the treatment of patients with type 2 diabetes mellitus after oral agent failure. Clin Ther. 1999; 21:1703-4. https://pubmed.ncbi.nlm.nih.gov/10566566
177. DeFronzo RA. Pharmacologic therapy for type 2 diabetes mellitus. Ann Intern Med. 1999; 131:281-303. https://pubmed.ncbi.nlm.nih.gov/10454950
178. Krentz AJ, Ferner RE, Bailey CJ. Comparative tolerability profiles of oral antidiabetic agents. Drug Safety. 1994; 11:223-41. https://pubmed.ncbi.nlm.nih.gov/7848543
184. Zoetica. Glycron (glyburide) micronized tablets prescribing information. Princeton, NJ; 1999 Apr.
185. American Diabetes Association. Gestational diabetes mellitus. Diabetes Care. 2002; 25(Suppl 1):S94-6.
186. Langer O, Conway DL, Berkus MD et al. A comparison of glyburide and insulin in women with gestational diabetes mellitus. N Engl J Med. 2000; 343:1134-8. https://pubmed.ncbi.nlm.nih.gov/11036118
188. Hermann LS, Scherstén B, Bitzén PO et al. Therapeutic comparison of metformin and sulfonylurea, alone and in various combinations. Diabetes Care. 1994; 17:1100-9. https://pubmed.ncbi.nlm.nih.gov/7821128
189. Hermann L. Biguanides and sulfonylureas as combination therapy in NIDDM. Diabetes Care. 1990; 13:37-41. https://pubmed.ncbi.nlm.nih.gov/2209342
193. United Kingdom prospective diabetes study group. United Kingdom prospective diabetes study (UKPDS) 16: overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes. 1995; 44:1240-58.
195. Wolffenbuttel BHR, Gomist R, Squatrito S et al. Addition of low-dose rosiglitazone to sulphonylurea therapy improves glycaemic control in type 2 diabetic patients. Diabet Med. 2000; 17:40-7. https://pubmed.ncbi.nlm.nih.gov/10691158
198. Kipnes MS, Krosnick a, Rendell MS et al. Pioglitazone hydrochloride in combination with sulfonylurea therapy improves glycemic control in patients with type 2 diabetes mellitus: a randomized, placebo-controlled study. Am J Med. 2001; 111:10-7. https://pubmed.ncbi.nlm.nih.gov/11448655
200. Chiasson J, Josse R, Hunt J et al. The efficacy of acarbose in the treatment of patients with non-insulin-dependent diabetes mellitus. Ann Intern Med. 1994; 121:929-935.
201. Coniff RF, Shapiro JA, Seaton TB et al. Multicenter, placebo-controlled trial comparing acarbose (BAY g 5421) with placebo, tolbutamide, and tolbutamide-plus-acarbose in non-insulin-dependent diabetes mellitus. Am J Med. 1995; 98:443-51. https://pubmed.ncbi.nlm.nih.gov/7733122
202. Calle-Pascual AL, Garcia-Honduvilla J, Martin-Alvarez PJ et al. Comparison between acarbose, metformin, and insulin treatment in type 2 diabetic patients with secondary failure to sulfonylurea treatment. Diabetes Metab. 1995; 21:256-60.
203. Klein W. Sulfonylurea-metformin-combination versus sulfonylurea-insulin-combination in secondary failures of sulfonylurea monotherapy. Diab Metab. 1991; 17(Suppl 1):235-40.
209. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. JAMA. 2002; 287:2563-9. https://pubmed.ncbi.nlm.nih.gov/12020338
211. Pfizer. Diflucan (fluconazole) tablets and powder for oral suspension prescribing information. New York, NY; 2024 Feb.
233. Actelion Pharmaceuticals US Inc. Tracleer (bosentan) tablets prescribing information. Titusville, NJ; 2024 Feb.
707. American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2025. Diabetes Care. 2025; 48(Suppl 1):S181-206.
708. Samson SL, Vellanki P, Blonde L et al. American Association of Clinical Endocrinology consensus statement: comprehensive type 2 diabetes management algorithm-2023. Endocr Pract. 2023; 28:305-340.
709. Institute for Safe Medication Practices (ISMP). ISMP list of high-alert medications in acute care settings (2024). https://www.ismp.org/system/files/resources/2024-01/ISMP_HighAlert_AcuteCare_List_010924_MS5760.pdf (accessed 2025 Mar 17).
710. Institute for Safe Medication Practices (ISMP). ISMP list of confused drug names (2024). https://online.ecri.org/hubfs/ISMP/Resources/ISMP_ConfusedDrugNames.pdf (accessed 2025 Mar 17).
711. Tirkkonen T, Heikkilä P, Huupponen R et al. Potential CYP2C9-mediated drug-drug interactions in hospitalized type 2 diabetes mellitus patients treated with the sulphonylureas glibenclamide, glimepiride or glipizide. J Intern Med. 2010; 268:359-66.
712. Niemi M, Backman JT, Neuvonen M et al. Effects of rifampin on the pharmacokinetics and pharmacodynamics of glyburide and glipizide. Clin Pharmacol Ther. 2001; 69: 400-6.
999. By the 2023 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023 Jul;71(7):2052-2081. doi: 10.1111/jgs.18372. Epub 2023 May 4. PMID: 37139824.
Related/similar drugs
More about glyburide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (9)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: sulfonylureas
- Breastfeeding