Exalgo Dosage
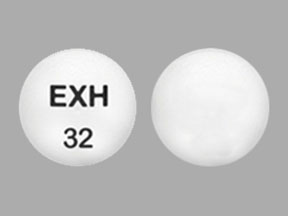
Generic name: HYDROMORPHONE HYDROCHLORIDE 8mg
Dosage form: tablet, extended release
Drug class: Opioids (narcotic analgesics)
Medically reviewed by Drugs.com. Last updated on Jun 19, 2025.
2.1 Important Dosage and Administration Information
To avoid medication errors, prescribers and pharmacists must be aware that hydromorphone is available as both immediate-release 8 mg tablets and extended-release 8 mg tablets.
EXALGO should be prescribed only by healthcare professionals who are knowledgeable in the use of potent opioids for the management of chronic pain.
Due to the risk of respiratory depression, EXALGO is only indicated for use in patients who are already opioid-tolerant. Discontinue or taper all other extended-release opioids when beginning EXALGO therapy. As EXALGO is only for use in opioid-tolerant patients, do not begin any patient on EXALGO as the first opioid.
Patients who are opioid-tolerant are those receiving, for one week or longer, at least 60 mg of oral morphine per day, at least 25 mcg transdermal fentanyl per hour, at least 30 mg of oral oxycodone per day, at least 8 mg of oral hydromorphone per day, at least 25 mg oral oxymorphone per day, at least
60 mg oral hydrocodone per day, or an equianalgesic dose of another opioid.
- Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals.
- Initiate the dosing regimen for each patient individually, taking into account the patient's prior analgesic treatment experience and risk factors for addiction, abuse, and misuse.
- Monitor patients closely for respiratory depression, especially within the first 24 to 72 hours of initiating therapy and following dosage increases with EXALGO and adjust the dosage accordingly.
Instruct patients to swallow EXALGO tablets whole. Crushing, chewing, or dissolving EXALGO tablets will result in uncontrolled delivery of hydromorphone and can lead to overdose or death.
2.2 Initial Dosage
Conversion from Other Oral Hydromorphone Formulations to EXALGO
Patients receiving oral immediate-release hydromorphone may be converted to EXALGO by administering a starting dose equivalent to the patient’s total daily oral hydromorphone dose, taken once daily.
Conversion from Other Oral Opioids to EXALGO
Discontinue all other around-the-clock opioid drugs when EXALGO therapy is initiated.
There is substantial inter-patient variability in the relative potency of different opioid drugs and opioid formulations. Therefore, a conservative approach is advised when determining the total daily dosage of EXALGO. It is safer to underestimate a patient’s 24-hour oral hydromorphone dosage and provide rescue medication (e.g., immediate-release opioid) than to overestimate the 24-hour oral hydromorphone dosage and manage an adverse reaction due to overdose.
In an EXALGO clinical trial with an open-label titration period, patients were converted from their prior opioid to EXALGO using the Table 1 as a guide for the initial EXALGO dose. The recommended starting dose of EXALGO is 50% of the calculated estimate of daily hydromorphone requirement. Calculate the estimated daily hydromorphone requirement using Table 1.
Consider the following when using the information in Table 1:
-
This is not a table of equianalgesic doses.
-
The conversion factors in this table are only for the conversion from one of the listed oral opioid analgesics to EXALGO.
-
The table cannot be used to convert from EXALGO to another opioid. Doing so will result in an overestimation of the dose of the new opioid and may result in fatal overdose.
Table 1.
Conversion Factors to EXALGO
|
Prior Oral Opioid |
Approximate Oral Conversion Factor |
|
Hydromorphone |
1 |
|
Codeine |
0.06 |
|
Hydrocodone |
0.4 |
|
Methadone |
0.6 |
|
Morphine |
0.2 |
|
Oxycodone |
0.4 |
|
Oxymorphone |
0.6 |
To calculate the estimated EXALGO dose using Table 1:
- For patients on a single opioid, sum the current total daily dose of the opioid and then multiply the total daily dose by the conversion factor to calculate the approximate oral hydromorphone daily dose.
- For patients on a regimen of more than one opioid, calculate the approximate oral hydromorphone dose for each opioid and sum the totals to obtain the approximate total hydromorphone daily dose.
- For patients on a regimen of fixed-ratio opioid/non-opioid analgesic products, use only the opioid component of these products in the conversion.
Always round the dose down, if necessary, to the appropriate EXALGO strength(s) available.
Example conversion from a single opioid to EXALGO:
Step 1: Sum the total daily dose of the opioid
- 30 mg of oxycodone 2 times daily = 60 mg total daily dose of oxycodone
Step 2: Calculate the approximate equivalent dose of oral hydromorphone based on the total daily dose of the current opioid using Table 1
- 60 mg total daily dose of oxycodone x Conversion Factor of 0.4 = 24 mg of oral hydromorphone daily
Step 3: Calculate the approximate starting dose of EXALGO to be given every 24 hours, which is 50% of the calculated oral hydromorphone dose. Round down, if necessary, to the appropriate EXALGO tablet strengths available.
- 50% of 24 mg results in an initial dose of 12 mg of EXALGO once daily
- Adjust individually for each patient
Close observation and frequent titration are warranted until pain management is stable on the new opioid. Monitor patients for signs and symptoms of opioid withdrawal or for signs of over-sedation/toxicity after converting patients to EXALGO.
Conversion from Transdermal Fentanyl to EXALGO
Eighteen hours following the removal of the transdermal fentanyl patch, EXALGO treatment can be initiated. To calculate the 24-hour EXALGO dose, use a conversion factor of 25 mcg/hr fentanyl transdermal patch to 12 mg of EXALGO. Then reduce the EXALGO dose by 50%.
For example:
Step 1: Identify the dose of transdermal fentanyl.
- 75 mg of transdermal fentanyl
Step 2: Use the conversion factor of 25 mcg/hr fentanyl transdermal patch to 12 mg of EXALGO.
-
75 mg of transdermal fentanyl: 36 mg total daily dose of EXALGO
Step 3: Calculate the approximate starting dose of EXALGO to be given every 24 hours, which is 50% of the converted dose. Round down, if necessary, to the appropriate EXALGO tablet strengths available.
-
50% of 36 mg results in an initial dose of 18 mg, which would be rounded down to
16 mg of EXALGO once daily -
Adjust individually for each patient
Conversion from Methadone to EXALGO
Close monitoring is of particular importance when converting from methadone to other opioid agonists. The ratio between methadone and other opioid agonists may vary widely as a function of previous dose exposure. Methadone has a long half-life and can accumulate in the plasma.
2.3 Titration and Maintenance of Therapy
Individually titrate EXALGO to a dose that provides adequate analgesia and minimizes adverse reactions. Continually reevaluate patients receiving EXALGO to assess the maintenance of pain control and the relative incidence of adverse reactions, as well as monitoring for the development of addiction, abuse, or misuse. Frequent communication is important among the prescriber, other members of the healthcare team, the patient, and the caregiver/family during periods of changing analgesic requirements, including initial titration. During chronic therapy, periodically reassess the continued need for opioid analgesics.
Plasma levels of EXALGO are sustained for 18 to 24 hours. Dosage adjustments of EXALGO may be made in increments of 4 to 8 mg every 3 to 4 days as needed to achieve adequate analgesia.
Patients who experience breakthrough pain may require a dose increase of EXALGO, or may need rescue medication with an appropriate dose of an immediate-release analgesic. If the level of pain increases after dose stabilization, attempt to identify the source of increased pain before increasing the EXALGO dose.
If unacceptable opioid-related adverse reactions are observed, the subsequent doses may be reduced. Adjust the dose to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
2.4 Safe Reduction or Discontinuation of EXALGO
Do not abruptly discontinue EXALGO in patients who may be physically dependent on opioids. Rapid discontinuation of opioid analgesics in patients who are physically dependent on opioids has resulted in serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse. Patients may also attempt to treat their pain or withdrawal symptoms with illicit opioids, such as heroin, and other substances.
When a decision has been made to decrease the dose or discontinue therapy in an opioid-dependent patient taking EXALGO, there are a variety of factors that should be considered, including the dose of EXALGO the patient has been taking, the duration of treatment, the type of pain being treated, and the physical and psychological attributes of the patient. It is important to ensure ongoing care of the patient and to agree on an appropriate tapering schedule and follow-up plan so that patient and provider goals and expectations are clear and realistic. When opioid analgesics are being discontinued due to a suspected substance use disorder, evaluate and treat the patient, or refer for evaluation and treatment of the substance use disorder. Treatment should include evidence-based approaches, such as medication assisted treatment of opioid use disorder. Complex patients with comorbid pain and substance use disorders may benefit from referral to a specialist.
There are no standard opioid tapering schedules that are suitable for all patients. Good clinical practice dictates a patient-specific plan to taper the dose of the opioid gradually. For patients on EXALGO who are physically opioid-dependent, initiate the taper by a small enough increment (e.g., no greater than 10% to 25% of the total daily dose) to avoid withdrawal symptoms, and proceed with dose-lowering at an interval of every 2 to 4 weeks. Patients who have been taking opioids for briefer periods of time may tolerate a more rapid taper.
It may be necessary to provide the patient with lower dosage strengths to accomplish a successful taper. Reassess the patient frequently to manage pain and withdrawal symptoms, should they emerge. Common withdrawal symptoms include restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. If withdrawal symptoms arise, it may be necessary to pause the taper for a period of time or raise the dose of the opioid analgesic to the previous dose, and then proceed with a slower taper. In addition, monitor patients for any changes in mood, emergence of suicidal thoughts, or use of other substances.
When managing patients taking opioid analgesics, particularly those who have been treated for a long duration and/or with high doses for chronic pain, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper. A multimodal approach to pain management may optimize the treatment of chronic pain, as well as assist with the successful tapering of the opioid analgesic.
2.5 Dosage Modifications in Patients with Moderate Hepatic Impairment
Start patients with moderate hepatic impairment on 25% of the EXALGO dose that would be prescribed for patients with normal hepatic function. Closely monitor patients with moderate hepatic impairment for respiratory and central nervous system depression during initiation of therapy with EXALGO and during dose titration. Use of alternate analgesics is recommended for patients with severe hepatic impairment.
2.6 Dosage Modifications in Patients with Renal Impairment
Start patients with moderate renal impairment on 50% of the EXALGO dose that would be prescribed for patients with normal renal function. Closely monitor patients with renal impairment for respiratory and central nervous system depression during initiation of therapy with EXALGO and during dose titration. As EXALGO is only intended for once daily administration, consider use of an alternate analgesic that may permit more flexibility with the dosing interval in patients with severe renal impairment.
Frequently asked questions
More about Exalgo (hydromorphone)
- Check interactions
- Compare alternatives
- Reviews (32)
- Drug images
- Latest FDA alerts (12)
- Side effects
- During pregnancy
- FDA approval history
- Drug class: Opioids (narcotic analgesics)
- Breastfeeding
Patient resources
Other brands
Dilaudid, Dilaudid-HP, Palladone
Professional resources
Other brands
Dilaudid, Dilaudid-HP, Palladone
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.