Bupivacaine / Meloxicam Dosage
Medically reviewed by Drugs.com. Last updated on Apr 2, 2024.
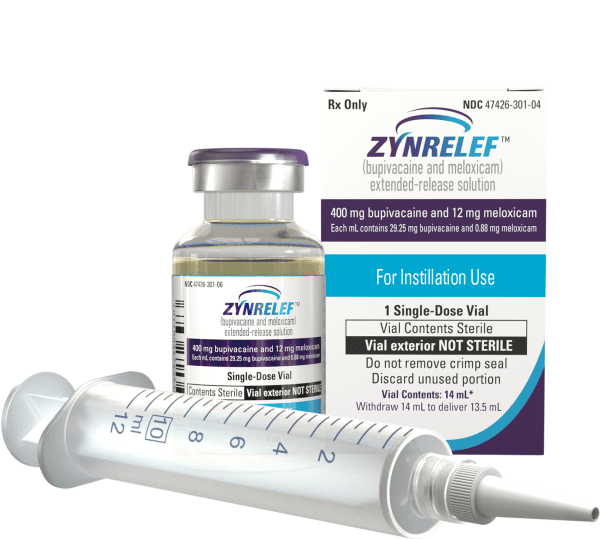
Applies to the following strengths: 400 mg-12 mg/14 mL; 200 mg-6 mg/7 mL
Usual Adult Dose for:
Additional dosage information:
Usual Adult Dose for Pain
For foot and ankle surgical procedures, such as bunionectomy: up to 2.3 mL (60 mg bupivacaine / 1.8 mg meloxicam)
For small-to-medium open abdominal surgical procedures, such as open inguinal herniorrhaphy: up to 10.5 mL (300 mg bupivacaine / 9 mg meloxicam)
For lower extremity total joint arthroplasty surgical procedures, such as total knee arthroplasty: up to 14 mL (400 mg bupivacaine / 12 mg meloxicam)
Comments:
- This drug is only intended for single-dose administration.
- Due to the potential for severe, life-threatening reactions to bupivacaine, only administer where trained personnel and equipment are available for prompt treatment of those who show evidence of neurologic or cardiac toxicity.
- The toxic effects of local anesthetics are additive; avoid use of other local anesthetics within 96 hours of use of this product.
Uses: For soft tissue or periarticular instillation to produce postsurgical analgesia for up to 72 hours after foot and ankle, small-to-medium open abdominal, and lower extremity total joint arthroplasty surgical procedures.
Limitations of Use: Safety and efficacy have not been established in highly vascular surgeries, such as intrathoracic, large multilevel spinal, and head and neck procedures.
Usual Adult Dose for Local Anesthesia
For foot and ankle surgical procedures, such as bunionectomy: up to 2.3 mL (60 mg bupivacaine / 1.8 mg meloxicam)
For small-to-medium open abdominal surgical procedures, such as open inguinal herniorrhaphy: up to 10.5 mL (300 mg bupivacaine / 9 mg meloxicam)
For lower extremity total joint arthroplasty surgical procedures, such as total knee arthroplasty: up to 14 mL (400 mg bupivacaine / 12 mg meloxicam)
Comments:
- This drug is only intended for single-dose administration.
- Due to the potential for severe, life-threatening reactions to bupivacaine, only administer where trained personnel and equipment are available for prompt treatment of those who show evidence of neurologic or cardiac toxicity.
- The toxic effects of local anesthetics are additive; avoid use of other local anesthetics within 96 hours of use of this product.
Uses: For soft tissue or periarticular instillation to produce postsurgical analgesia for up to 72 hours after foot and ankle, small-to-medium open abdominal, and lower extremity total joint arthroplasty surgical procedures.
Limitations of Use: Safety and efficacy have not been established in highly vascular surgeries, such as intrathoracic, large multilevel spinal, and head and neck procedures.
Renal Dose Adjustments
Mild to Moderate Renal Dysfunction: Dose adjustment(s) may be required; however, no specific guidelines have been suggested. Caution is recommended.
Severe Renal Dysfunction: Use is not recommended.
- Bupivacaine and meloxicam and their metabolites are renally excreted, increasing the risk of toxic reactions in patients with renal dysfunction.
- Consider a dose reduction for mild to moderate renal dysfunction.
- Patients with severe renal dysfunction may be more susceptible to amide-type local anesthetic toxicities.
- Patients with severe renal dysfunction have not been adequately studied.
Liver Dose Adjustments
Mild to Moderate Liver Dysfunction (Child-Pugh class 1 to 2): No adjustment recommended.
Severe Liver Dysfunction (Child-Pugh class 3): Use is not recommended; use only if benefits outweigh risks.
- Amide-type local anesthetics like bupivacaine are primarily hepatically metabolized.
- Patients with severe liver disease are at greater risk of toxicities and developing toxic plasma concentrations due to their inability to metabolize local anesthetics normally.
- Monitor patients with hepatic impairment for worsening hepatic impairment.
- Consider monitoring patients with moderate to severe liver dysfunction for local anesthetic systemic toxicity.
- This product has not been adequately studied in severe liver impairment.
Dose Adjustments
Poor Metabolizers of CYP450 2C9 Substrates:
- Poor CYP450 2C9 metabolizers may have abnormally high meloxicam plasma levels due to reduced metabolic clearance.
- Consider a dose reduction for known or suspected poor CYP450 2C9 metabolizers (based on genotype or experience with other CYP450 2C9 substrates like warfarin or phenytoin).
- Monitor for adverse effects.
Precautions
US BOXED WARNING(S):
Risk of Serious Cardiovascular and Gastrointestinal Events:
- NSAIDs increase the risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk occurs early in treatment and may increase with duration of use.
- This drug is contraindicated in the setting of coronary artery bypass graft (CABG) surgery.
- NSAIDs increase the risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, or perforation of the stomach or intestines, which may be fatal. These events may occur any time during treatment without warning symptoms.
- Elderly patients and patients with a history of peptic ulcer disease and/or GI bleeding are at increased risk of serious GI events.
CONTRAINDICATIONS:
- Serious hypersensitivity (e.g. anaphylactic reaction, serious skin reaction) to any amide-type local anesthetic agent, NSAIDs, or any other ingredient in the formulation
- History of asthma, urticaria, or other allergic-type reaction after aspirin or other NSAIDs. Severe, sometimes fatal, anaphylactic reactions to NSAIDs have been reported in such patients.
- Use for obstetrical paracervical block anesthesia: use of bupivacaine in this technique has led to fetal bradycardia and death.
- Use for coronary artery bypass graft (CABG) surgery
Safety and efficacy have not been established in patients younger than 18 years.
This drug is not recommended for use in children.
Consult WARNINGS section for additional precautions.
Dialysis
Use is not recommended in severe renal impairment.
- Meloxicam is not dialyzable.
Hemodialysis: Do not exceed maximum recommended dose or use with other meloxicam-containing products.
Peritoneal dialysis: Data not available
Other Comments
Administration advice:
- Avoid intravascular administration: convulsions and cardiac arrest have occurred after accidental intravascular injection of bupivacaine and other amide-containing products.
- Do not give via the following routes: epidural, intrathecal, intravascular, intra-articular, regional nerve blocks, pre-incisional or pre-procedural locoregional anesthetic techniques
- Bunionectomy: apply to proximal distal ends (beyond the bony repair) of the wound.
- Open inguinal herniorrhaphy: apply above and below fascial repair.
- Total knee arthroplasty: apply directly to posterior capsule, anteromedial tissues and periosteum, and anterolateral tissues and periosteum after cementation of components.
- Restrict exposure to articular cartilage as it carries the potential risk of chondrolysis.
- Only apply to tissue layers below the skin incision and not directly onto the subdermal layer or the skin.
- Use only enough to coat tissues so it does not leak from the closed surgical wound.
- Apply without a needle into the surgical site after final irrigation and suction, and prior to suturing of each layer when multiple tissue layers are involved.
- If a topical antiseptic (e.g. povidone) is applied, allow site to dry before applying this product.
Storage requirements:
- Kits can be stored at 20C to 25C (68F to 77F); excursions permitted between 15C to 30C (59F to 86F).
- If vials are removed from kits, store at controlled room temperature.
- Protect from moisture and light.
Reconstitution/preparation techniques:
- Do not dilute.
- Do not mix with water, saline, or other local anesthetics: product may become more viscous and difficult to administer.
Compatibility:
- Surgical mesh materials, including polypropylene, Gore-tex, and polyester
- Silicone membranes
- Bone cement
- Metal alloys used in surgical implants
Patient advice:
- Patients should remain vigilant for symptoms of cardiovascular thrombotic events such as chest pain, shortness of breath, weakness, or slurred speech. They should promptly notify their healthcare provider if they experience any of these symptoms.
- Patients should inform their healthcare provider about symptoms of ulcerations and bleeding, such as epigastric pain, dyspepsia, melena, and hematemesis. When using low-dose aspirin for cardiac prophylaxis, patients should be aware of the increased risk of gastrointestinal bleeding and its associated signs and symptoms.
- Educate patients about the signs of an anaphylactic reaction, such as breathing difficulties and facial or throat swelling. Instruct them to seek immediate emergency assistance if they experience these symptoms.
- Instruct patients to promptly notify their healthcare provider if they experience a rash or fever.
- Notify patients about the potential risk of methemoglobinemia, a serious condition that can be caused by the use of local anesthetics. Emphasize the importance of seeking prompt medical attention if they encounter the following signs or symptoms: pale, gray, or blue skin color (cyanosis), headache, rapid heart rate, shortness of breath, lightheadedness, or fatigue.
- Notify pregnant women about the potential risk of premature closure of the fetal ductus arteriosus when using this drug or other NSAIDs starting at 30 weeks gestation. If treatment with this drug is required between approximately 20 to 30 weeks gestation, advise monitoring for oligohydramnios as meloxicam can be detected in plasma beyond 48 hours after administration.
- Advise patients beforehand that this drug may temporarily cause numbness near the surgical area.
- Notify patients about the increased risk of gastrointestinal toxicity when using an NSAID or salicylate (e.g., diflunisal, salsalate) in the postoperative period after receiving this drug.
More about bupivacaine / meloxicam
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- During pregnancy
- Drug class: analgesic combinations
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.