Bupivacaine and Meloxicam (Local) (Monograph)
Drug class: Local Anesthetics
Warning
Risk of Serious Cardiovascular and GI Events
-
Nonsteroidal anti-inflammatory agents (NSAIAs) cause an increased risk of serious cardiovascular thrombotic events, including MI and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use.
-
Bupivacaine/meloxicam is contraindicated in the setting of coronary artery bypass graft (CABG) surgery.
-
NSAIAs cause an increased risk of serious adverse GI events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events.
Introduction
Fixed-combination, extended-release solution containing bupivacaine (amide local anesthetic) and meloxicam (nonsteroidal anti-inflammatory agent [NSAIA]).
Uses for Bupivacaine and Meloxicam (Local)
Postsurgical Analgesia
Used in adults for soft tissue or periarticular instillation to produce postsurgical analgesia for up to 72 hours after bunionectomy, open inguinal herniorrhaphy, or total knee arthroplasty.
Safety and efficacy not established in highly vascular surgeries, such as intrathoracic, large multilevel spinal, and head and neck procedures.
A multimodal approach to manage postoperative analgesia is recommended. The combination of bupivacaine/meloxicam may be considered for use in perioperative analgesia.
Bupivacaine and Meloxicam (Local) Dosage and Administration
General
Pretreatment Screening
-
Correct volume status in dehydrated or hypovolemic patients prior to initiating bupivacaine/meloxicam.
Patient Monitoring
-
If benefits outweigh risks and bupivacaine/meloxicam is used in patients with a recent MI, monitor for signs of cardiac ischemia.
-
Monitor for signs and symptoms of GI ulceration and bleeding.
-
Monitor for signs of bleeding in patients with coagulation disorders or patients taking concomitant drugs that increase the risk of bleeding.
-
If additional local anesthetic use cannot be avoided, monitor for neurologic and cardiovascular effects associated with local anesthetic systemic toxicity. Monitor cardiovascular and respiratory vital signs and level of consciousness.
-
Monitor BP, heart rate, and ECG changes closely in patients with impaired cardiovascular function.
-
If used in patients with severe heart failure, monitor for signs of worsening heart failure.
-
Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia.
-
Monitor for signs and symptoms of methemoglobinemia (initial signs include cyanotic skin discoloration and/or abnormal coloration of blood) in patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants <6 months of age, and concurrent exposure to oxidizing agents or their metabolites.
-
Monitor for exacerbation of asthma symptoms in patients with preexisting asthma (without known aspirin sensitivity).
-
Monitor for oligohydramnios via ultrasound in pregnant patients who receive treatment between 20 and 30 weeks gestation.
Other General Considerations
-
Administer in a setting where trained personnel and equipment are available to promptly treat patients who experience neurologic or cardiac toxicity.
-
Avoid additional use of local anesthetics within 96 hours following administration.
Administration
Soft tissue/Periarticular Instillation
Sterile solution for administration by soft tissue or periarticular instillation into surgical site.
Do not administer via epidural, intrathecal, intravascular, intra-articular routes.
Solution should be clear, pale-yellow to yellow, viscous, and free from particulates. Do not use if the solution is discolored or contains visible particles.
Apply without a needle into the surgical site following final irrigation and suctioning and prior to suturing of each layer when multiple tissue layers are involved. When the solution comes in contact with moisture in the tissues, it becomes more viscous, allowing it to stay in place.
Attach vented vial spike to vial. Fill syringe with air and attach to vial spike. Invert, inject air, then withdraw the required volume. Solution is very thick; may take a few minutes to withdraw. Instill to tissue layers below the skin incision; minimize administration near the incision line; consult prescribing information for additional details.
Allow the site to dry after application of a topical antiseptic such as povidone and iodine before administering bupivacaine/meloxicam.
Do not mix bupivacaine/meloxicam with water, saline, or other local anesthetics as the product will become more viscous and difficult to administer.
Dosage
Adults
Foot and Ankle Procedures (e.g., Bunionectomy)
Soft tissue Instillation
Up to 2.3 mL to deliver 60 mg bupivacaine and 1.8 mg meloxicam.
Small to Medium Open Abdominal Procedures (e.g., Open Inguinal Herniorrhaphy)
Soft tissue Instillation
Up to 10.5 mL to deliver 300 mg bupivacaine and 9 mg meloxicam.
Lower Extremity Total Joint Arthroplasty (e.g., Total Knee Arthroplasty)
Periarticular Instillation
Up to 14 mL to deliver 400 mg bupivacaine and 12 mg meloxicam.
Special Populations
Hepatic Impairment
No adjustment for mild to moderate impairment. Use in patients with severe hepatic impairment if benefits outweigh risks; close monitoring is advised.
Renal Impairment
Consider dosage reduction for mild to moderate impairment. Use not recommended in severe renal impairment.
Geriatric Use
Consider lower doses and monitor renal function
Poor Metabolizers of CYP2C9 Substrates
Consider lower doses for CYP2C9 poor metabolizers; use lowest effective dosage and monitor for adverse effects.
Cautions for Bupivacaine and Meloxicam (Local)
Contraindications
-
Patients with a known hypersensitivity (e.g., anaphylactic reactions, serious skin reactions) to any local anesthetic agent of the amide-type, NSAIAs, or to any of the other components of bupivacaine/meloxicam.
-
Patients with a history of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIAs.
-
Patients undergoing obstetrical paracervical block anesthesia.
-
Patients undergoing CABG surgery.
Warnings/Precautions
Warnings
Cardiovascular Thrombotic Events with NSAIA Use
Increased risk of cardiovascular events (e.g., MI, stroke), which can be fatal, including in patients with recent CABG surgery and recent MI (see Boxed Warning). Higher risk possibly related to higher doses. Uncertain risk with single-dose local application of bupivacaine/meloxicam. Do not exceed recommended dose.
Do not use in patients with recent CABG surgery or in patients with recent MI. Inform patients to seek immediate care if cardiovascular signs and symptoms occur.
GI Ulceration and Perforation with NSAIA Use
Serious adverse GI events, including inflammation, bleeding, ulceration, and perforation of the esophagus, stomach, small intestine, or large intestine, which can be fatal, can occur with NSAIAs, including meloxicam. (See Boxed Warning.)
Use the recommended dose. Avoid using multiple NSAIAs. Avoid in high risk patients. Monitor for signs and symptoms of GI bleeding; evaluate and treat promptly if a serious GI event is suspected. Monitor patients more closely if they are treated with concomitant low-dose aspirin for cardiac prophylaxis.
Other Warnings and Precautions
Dose-related Toxicity
Toxic effects of local anesthetics are additive. Avoid additional local anesthetic administration within 96 hours following bupivacaine/meloxicam instillation. Monitor neurologic, cardiovascular, and respiratory status.
Risk of Use in Patients with Impaired Cardiovascular Function
Patients with impaired cardiovascular function may not compensate for functional changes related to prolongation of AV conduction. Monitor BP, heart rate, and ECG changes.
Hepatoxicity
Amide-type local anesthetics (e.g., bupivacaine) metabolized by the liver. Use with caution in hepatic disease because of risk of toxic plasma concentrations.
Elevations of ALT or AST (≥3 times ULN) reported in approximately 1% of NSAIA-treated patients in clinical trials. Elevations of ALT or AST (<3 times ULN) may occur in up to 15% of patients treated with NSAIAs. Uncertain risk following single-dose local application of bupivacaine/meloxicam.
Monitor for signs and symptoms of hepatotoxicity.
Hypertension
NSAIAs, including meloxicam, can lead to new onset of hypertension or worsening of preexisting hypertension. Efficacy of angiotensin converting enzyme (ACE) inhibitors, thiazide diuretics, or loop diuretics may be reduced by NSAIAs.
Monitor BP after administration.
Heart Failure and Edema
Increased hospitalizations for heart failure, risk of MI, fluid retention, edema, and death observed with use of NSAIAs. Meloxicam may blunt cardiovascular effects of several therapeutic agents used to treat these medical conditions, including diuretics, ACE inhibitors, or angiotensin receptor blockers (ARBs). Uncertain risk of these events following single-dose local application of bupivacaine/meloxicam.
Avoid use in severe heart failure unless benefits are expected to outweigh risks of worsening heart failure. Monitor for worsening heart failure if used.
Renal Toxicity and Hyperkalemia
Higher risk of renal toxicity when NSAIAs used in patients with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors or ARBs, and in the elderly. Discontinuation of NSAIA therapy typically leads to recovery to the pretreatment state.
Monitor patients with preexisting renal disease, hepatic impairment, heart failure, dehydration, and hypovolemia for signs of worsening renal function. Correct volume status in dehydrated or hypovolemic patients prior to initiating bupivacaine/meloxicam.
Avoid use in patients with advanced renal disease unless the benefits are expected to outweigh risk of worsening renal function.
Increases in serum potassium concentration, including hyperkalemia, reported with use of NSAIAs.
Anaphylactic Reactions
Anaphylactic reactions reported in patients with and without known hypersensitivity to meloxicam and in patients with aspirin-sensitive asthma.
Seek emergency help if an anaphylactic reaction occurs.
Chondrolysis
Limit exposure to articular cartilage due to the potential risk of chondrolysis.
Methemoglobinemia
Cases of methemoglobinemia reported in association with local anesthetic use.
Higher susceptibility in patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, or cardiac or pulmonary compromise, those with concurrent exposure to oxidizing agents or their metabolites, and infants <6 months of age. If used in these patients, closely monitor and immediately treat for symptoms and signs (cyanotic skin discoloration and/or abnormal coloration of the blood) of methemoglobinemia.
Exacerbation of Asthma Related to Aspirin Sensitivity
NSAIAs are contraindicated in patients with aspirin-sensitive asthma. If used in patients with preexisting asthma (without known aspirin sensitivity), monitor for exacerbation of asthma symptoms.
Serious Skin Reactions
Exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal, can occur with NSAIAs, including meloxicam. Inform patients about the signs and symptoms of serious skin reactions.
Bupivacaine/meloxicam is contraindicated in patients with previous serious skin reactions to NSAIAs.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
Drug reaction with eosinophilia and systemic symptoms (DRESS), including fatal or life-threatening cases, reported in patients taking NSAIAs such as bupivacaine/meloxicam. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling. Other clinical manifestations may include hepatitis, nephritis, hematologic abnormalities, myocarditis, or myositis.
If such signs or symptoms are present, evaluate patient immediately and treat as clinically indicated.
Fetal Toxicity
Avoid use of NSAIAs, including bupivacaine/meloxicam, in pregnant women at about 30 weeks gestation and later. NSAIAs, including bupivacaine/meloxicam, increase the risk of premature closure of the fetal ductus arteriosus at approximately this gestational age.
Use of NSAIAs, including bupivacaine/meloxicam, at about 20 weeks gestation or later in pregnancy may cause fetal renal dysfunction leading to oligohydramnios and, in some cases, neonatal renal impairment after days to weeks of treatment. May or may not be reversible with treatment discontinuation.
If NSAIA treatment is necessary between about 20 and 30 weeks gestation, limit bupivacaine/meloxicam use to the lowest effective dose. Consider ultrasound monitoring for oligohydramnios. If oligohydramnios occurs, follow up according to clinical practice.
Hematologic Toxicity
Anemia has occurred in NSAIA-treated patients. If signs or symptoms of anemia occur, monitor hemoglobin or hematocrit.
NSAIAs, including meloxicam, may increase the risk of bleeding events. Co-morbid conditions such as coagulation disorders or concomitant use of warfarin, other anticoagulants, antiplatelet agents (e.g., aspirin), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs) may increase this risk. Monitor patients for signs of bleeding.
Masking of Inflammation and Fever
Utility of diagnostic signs of inflammation and fever in detecting infections may be diminished.
Specific Populations
Pregnancy
Risk of combined use of bupivacaine and meloxicam during human pregnancy unknown.
Data with bupivacaine alone in pregnant women inconclusive. Embryofetal lethality reported in some animal studies at exposures equivalent to the maximum recommended human dose.
Use of NSAIAs, including meloxicam, can cause premature closure of fetal ductus arteriosus and fetal renal dysfunction leading to oligohydramnios and, in some cases, neonatal renal impairment. Limit dose and duration of bupivacaine/meloxicam use between about 20 and 30 weeks of gestation. Avoid bupivacaine/meloxicam use at about 30 weeks of gestation and later in pregnancy.
Embryofetal death, septal heart defects, dystocia, delayed parturition, and decreased offspring survival reported in animal studies with oral meloxicam; no malformations reported.
Lactation
Bupivacaine is present in human milk. Not known if meloxicam is present in human milk. Consider benefits of breastfeeding to infant and benefit of treatment to mother.
Females and Males of Reproductive Potential
Meloxicam may delay or prevent rupture of ovarian follicles. Consider withdrawal of NSAIAs and avoidance of bupivacaine/meloxicam in women who have difficulties conceiving or who are undergoing investigation of infertility.
Decreased sperm count, motility, and testicular degeneration reported in male animal studies with oral meloxicam. Clinical relevance unknown.
Pediatric Use
Safety and effectiveness in pediatric patients not established.
Geriatric Use
Elderly patients, compared to younger patients, at greater risk for NSAIA-associated serious cardiovascular, GI, and/or renal adverse reactions, although applicability of this to a single administration of low-dose meloxicam in bupivacaine/meloxicam is uncertain
Consider dose reduction in elderly patients. Monitor renal function.
Hepatic Impairment
Hepatic disease may alter the pharmacokinetics of local anesthetics. Severe hepatic disease can increase susceptibility to toxicity.
Mild to moderate hepatic impairment had no substantial impact on meloxicam pharmacokinetics. Impact of severe hepatic impairment on meloxicam pharmacokinetics not studied.
Renal Impairment
Renal disease may alter pharmacokinetics of local anesthetics.
Total plasma meloxicam concentration decreased and drug clearance increased with renal impairment, possibly due to increased fraction of unbound meloxicam which is available for hepatic metabolism.
Consider reducing dosage of bupivacaine/meloxicam in patients with mild to moderate renal impairment. Use in severe renal impairment not recommended.
Pharmacogenomic Considerations: Poor CYP2C9 Metabolizers
In patients who are known or suspected to be poor CYP2C9 metabolizers based on genotype or previous history/experience with other CYP2C9 substrates (such as warfarin or phenytoin), consider dosage reduction. Monitor for adverse effects.
Common Adverse Effects
Most common adverse reactions (incidence ≥10%): constipation, vomiting, headache.
Drug Interactions
Meloxicam is metabolized via CYP2C9 with a minor contribution of CYP3A4; bupivacaine is metabolized primarily in the liver via conjugation with glucuronic acid.
Drugs Associated with Methemoglobinemia
Local anesthetics can increase the risk of developing methemoglobinemia in patients concurrently exposed to other drugs associated with the condition, including nitrate/nitrites, other local anesthetics, certain antineoplastic agents, antibiotics, antimalarials, anticonvulsants, as well as acetaminophen, metoclopramide, quinine, and sulfasalazine.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Local anesthetics (articaine, benzocaine, bupivacaine, lidocaine, mepivacaine, prilocaine, procaine, ropivacaine, tetracaine) |
Additive toxic local anesthetic systemic effects. Higher risk of methemoglobinemia. |
Avoid additional use of local anesthetics within 96 hours from initial administration of bupivacaine and meloxicam. Monitor closely if administered sooner or at all. |
|
Drug |
Interactions |
Comments |
|---|---|---|
|
ACE inhibitors |
NSAIAs, including meloxicam, may diminish antihypertensive effect. Coadministration in elderly or in patients who are volume-depleted or have renal impairment can lead to renal function decline including acute renal failure. |
Monitor BP. Monitor for signs of worsening renal function in high-risk patients. |
|
Anticoagulants (e.g., warfarin) |
Increased risk of serious bleeding. |
Monitor for signs of bleeding. |
|
Angiotensin receptor blockers (ARBs) |
NSAIAs, including meloxicam, may diminish antihypertensive effect. Coadministration in elderly or in patients who are volume-depleted or have renal impairment can lead to renal function decline including acute renal failure. |
Monitor BP. Monitor for signs of worsening renal function in high-risk patients |
|
Aspirin |
Increased risk of adverse GI reactions. |
Monitor for signs of bleeding. |
|
Beta-blockers |
NSAIAs, including meloxicam, may diminish antihypertensive effect. Coadministration in elderly or in patients who are volume-depleted or have renal impairment can lead to renal function decline including acute renal failure. |
Monitor BP. Monitor for signs of worsening renal function in high-risk patients. |
|
Cyclosporine |
NSAIAs may increase cyclosporine nephrotoxicity. |
Monitor for signs of worsening renal function |
|
Diuretics (furosemide, thiazide diuretics) |
Meloxicam did not impact pharmacokinetics of furosemide NSAIAs may reduce natriuretic effect. |
Monitor renal function and diuretic efficacy. |
|
Digoxin |
NSAIAs may increase concentration and prolong half-life of digoxin. |
Monitor serum digoxin levels. |
|
Lithium |
NSAIAs may increase plasma lithium levels and reduce lithium clearance. |
Monitor for signs of lithium toxicity. |
|
Methotrexate |
NSAIAs may increase methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction) |
Monitor for methotrexate toxicity. |
|
NSAIAs/Salicylates |
Increased risk of GI toxicity. |
Monitor for signs of GI toxicity if additional NSAIA treatment is indicated in the post-operative period. |
|
Pemetrexed |
NSAIAs may increase pemetrexed-associated myelosuppression and renal and GI toxicity. |
Interrupt meloxicam for 5 days before, the day of, and 2 days after pemetrexed administration. Monitor for myelosuppression, renal, and GI toxicity in patients with Clcr 45–79 mL/minute. Avoid concomitant administration in patients with Clcr <45 mL/minute. |
|
SSRIs/SNRIs |
Increased risk of serious bleeding |
Monitor for signs of bleeding |
Bupivacaine and Meloxicam (Local) Pharmacokinetics
Absorption
Absorption
Systemic absorption from extended-release, sterile solution dependent on total dose and vascularity of administration site.
Onset
Time to maximum bupivacaine concentration: 3 hours (bunionectomy), 18 hours (herniorrhaphy), 21 hours (total knee arthroplasty).
Time to maximum meloxicam concentration: 18 hours (bunionectomy), 54 hours (herniorrhaphy), 36 hours (total knee arthroplasty).
Systemic plasma levels of bupivacaine or meloxicam following application of bupivacaine/meloxicam do not correlate with local efficacy.
Distribution
Extent
Bupivacaine
Distribution after local instillation and absorption of bupivacaine/meloxicam is expected to be the same as for other bupivacaine solution formulations.
Extensive; high concentration in highly perfused organs (liver, heart, lungs, and brain).
95% protein bound.
Crosses placenta; fetal/maternal ratio 0.2–0.4.
Present in human milk.
Meloxicam
Distribution after local instillation and absorption of bupivacaine/meloxicam is expected to be the same as for oral meloxicam.
~99.4% protein bound (primarily albumin).
Free fraction in synovial fluid 2.5 times higher than in plasma.
Unknown if present in human milk.
Elimination
Half-Life
Bupivacaine: 14–15 hours.
Meloxicam 22–25 hours.
Special Populations
Poor Metabolizers of CYP2C9 Substrates
Meloxicam concentrations substantially higher in CYP2C9 poor metabolizers compared to normal metabolizers.
Stability
Storage
Parenteral
Solution for Soft Tissue or Periarticular Instillation.
Store vials at 20–25°C (excursions permitted between 15–30°C). Protect from moisture and light. If vials are removed from the kit, store at controlled room temperature protected from light.
Actions
Bupivacaine
-
Blocks generation and conduction of nerve impulses presumably by increasing threshold for electrical excitation in the nerve, by slowing propagation of nerve impulse, and by reducing rate of rise of the action potential.
Meloxicam
-
Potent inhibitor of prostaglandin synthesis in vitro. Prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain in animal models.
-
Prostaglandins are mediators of inflammation; mode of action of meloxicam may be due to a decrease of prostaglandins in peripheral tissues.
Advice to Patients
-
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately.
-
Advise patients to report symptoms of ulcerations and bleeding, including epigastric pain, dyspepsia, melena, and hematemesis to their health care provider. In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, inform patients of the increased risk for and the signs and symptoms of GI bleeding.
-
Inform patients of the signs of an anaphylactic reaction (e.g., difficulty breathing, swelling of the face or throat).
-
Advise patients to contact their healthcare provider as soon as possible if they develop any type of rash or fever.
-
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue.
-
Inform pregnant women of the risk of the premature closing of the fetal ductus arteriosus if bupivacaine/meloxicam or other NSAIAs are used starting at 30 weeks gestation. If treatment with bupivacaine/meloxicam is needed for a pregnant woman between about 20 to 30 weeks gestation, advise monitoring may be needed for oligohydramnios because meloxicam can be detected in plasma beyond 48 hours after administration.
-
Inform patients in advance that bupivacaine/meloxicam can cause temporary loss of sensation near the surgical site.
-
Inform patients of the increased risk of GI toxicity if an NSAIA or salicylate (e.g., diflunisal, salsalate) is used in the postoperative period following administration of bupivacaine/meloxicam.
-
Advise women to inform their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
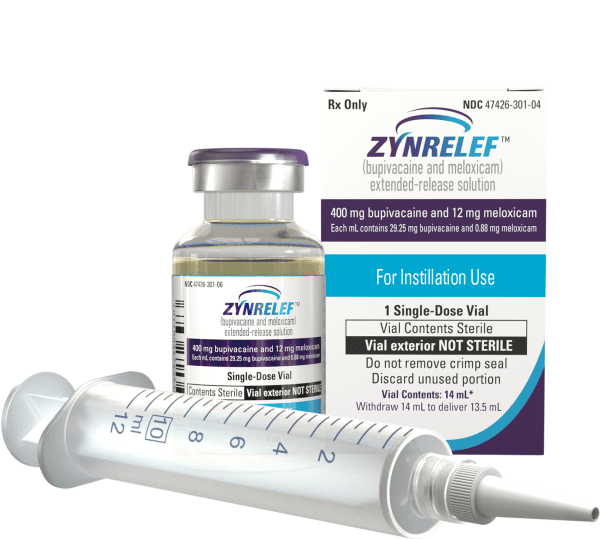
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Solution, extended-release, for soft tissue or periarticular instillation |
Bupivacaine 29.25 mg and meloxicam 0.88 mg per mL |
Zynrelef (available in 4 presentations for single-dose application [400 mg bupivacaine/12 mg meloxicam, 300 mg bupivacaine/9 mg meloxicam, 200 mg bupivacaine/6 mg meloxicam, and 60 mg bupivacaine/1.8 mg meloxicam]) |
Heron Therapeutics |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about bupivacaine / meloxicam
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: analgesic combinations
- En español