Clarithromycin Disease Interactions
There are 5 disease interactions with clarithromycin.
Antibiotics (applies to clarithromycin) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
Clarithromycin (applies to clarithromycin) hepatotoxicity
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
Hepatic dysfunction, including increased liver enzymes, and hepatocellular and/or cholestatic hepatitis, with or without jaundice, has been reported in patients receiving clarithromycin. The hepatic dysfunction may be severe but in most cases is reversible. Fatal outcomes have also been reported and in general have been associated with serious underlying diseases and/or concomitant medications. Caution and monitoring is advised if using this drug in patients with hepatic impairment. Treatment must be discontinued immediately if signs and symptoms of hepatitis occur (e.g., anorexia, jaundice, dark urine, pruritus, or tender abdomen). The use of clarithromycin and combination medications containing this antibiotic are contraindicated in patients with a history of cholestatic jaundice or hepatic impairment associated with the prior use of clarithromycin.
Clarithromycin (applies to clarithromycin) renal dysfunction
Moderate Potential Hazard, Moderate plausibility.
Clarithromycin is primarily eliminated by the kidney and liver. A decreased dosage or prolonged dosing intervals are recommended in patients with severe renal impairment (CrCl < 30 mL/min). Dosage adjustments are usually not necessary in patients with mild to moderate renal impairment, although drug accumulation could occur in the presence of concomitant liver disease. Monitoring is advised.
Macrolide antibiotics (applies to clarithromycin) myasthenia gravis
Moderate Potential Hazard, Moderate plausibility.
The use of macrolide antibiotics has been reported to exacerbate symptoms of myasthenia gravis and trigger new onset of symptoms of myasthenic syndrome. Therapy with these agents should be administered cautiously in patients with a history of myasthenia gravis.
Macrolide antibiotics (applies to clarithromycin) QT prolongation
Moderate Potential Hazard, High plausibility. Applicable conditions: Hypokalemia, Magnesium Imbalance, Arrhythmias
Macrolides have been associated with prolongation of the QT interval and infrequent cases of arrhythmia. Clarithromycin and erythromycin should be avoided in: patients with known prolongation of the QT interval, ventricular cardiac arrhythmia, including torsades de pointes; patients with proarrhythmic conditions such as uncorrected hypokalemia or hypomagnesemia, clinically significant bradycardia, or receiving other drugs that prolong the QT interval.
Switch to professional interaction data
Clarithromycin drug interactions
There are 727 drug interactions with clarithromycin.
Clarithromycin alcohol/food interactions
There is 1 alcohol/food interaction with clarithromycin.
More about clarithromycin
- clarithromycin consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (854)
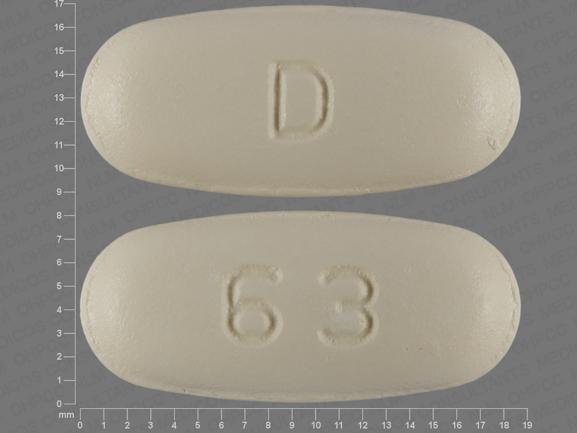
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: macrolides
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.