Aspirin/omeprazole Disease Interactions
There are 12 disease interactions with aspirin / omeprazole.
- Coagulation
- Asthma
- C. diff
- GI toxicity
- Renal dysfunction
- Reye's syndrome
- Bone fractures
- Hypomagnesemia
- Anemia
- Dialysis
- G-6-PD deficiency
- Hepatotoxicity
Aspirin (applies to aspirin/omeprazole) coagulation
Major Potential Hazard, High plausibility. Applicable conditions: Coagulation Defect, Bleeding, Thrombocytopathy, Thrombocytopenia, Vitamin K Deficiency
The use of aspirin is contraindicated in patients with significant active bleeding or hemorrhagic disorders such as hemophilia, von Willebrand's disease, or telangiectasia. Aspirin interferes with coagulation by irreversibly inhibiting platelet aggregation and prolonging bleeding time. The non-aceylated salicylates (i.e. salicylate salts such as sodium or magnesium salicylate) do not demonstrate these effects and may be appropriate substitutions in these patients. However, all salicylates can interfere with the action of vitamin K and induce a dose-dependent alteration in hepatic synthesis of coagulation factors VII, IX and X. At usual recommended dosages, a slight increase in prothrombin time (PT) may occur. Therapy with salicylates, especially aspirin, should be administered with extreme caution in patients with hypoprothrombinemia, vitamin K deficiency, thrombocytopenia, thrombotic thrombocytopenic purpura, severe hepatic impairment, or anticoagulant use.
NSAIDs (applies to aspirin/omeprazole) asthma
Major Potential Hazard, Moderate plausibility.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are contraindicated in patients with history of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs; severe, sometimes fatal, anaphylactic reactions to NSAIDs have been reported in such patients. A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps, severe potentially fatal bronchospasm, and/or intolerance to aspirin and other NSAIDs. Since cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, therapy with any NSAID should be avoided in patients with this form of aspirin sensitivity. NSAIDs should be used with caution in patients with preexisting asthma (without known aspirin sensitivity), and these patients should be monitored for changes in the signs and symptoms of asthma.
PPIs (applies to aspirin/omeprazole) C. diff
Major Potential Hazard, Moderate plausibility. Applicable conditions: Pseudomembranous Colitis, Diarrhea
Published observational studies suggest that proton pump inhibitor (PPI) use may be associated with an increased risk of Clostridium difficile-associated diarrhea (CDAD), especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve. It is recommended that patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Close monitoring is recommended in patients with diarrhea and in those taking antibacterial agents as CDAD has been reported with the use of nearly all these agents. Treatment with antibacterial agents alters the normal flora of the colon, leading to overgrowth of C. difficile. C. difficile produces toxins A and B, which contribute to the development of CDAD. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Salicylates (applies to aspirin/omeprazole) GI toxicity
Major Potential Hazard, High plausibility. Applicable conditions: Peptic Ulcer, Duodenitis/Gastritis, Gastrointestinal Hemorrhage, Gastrointestinal Perforation, History - Peptic Ulcer, Alcoholism, Colitis/Enteritis (Noninfectious), Colonic Ulceration
Salicylates, particularly aspirin, can cause dose-related gastrointestinal bleeding and mucosal damage, which may occur independently of each other. Occult, often asymptomatic GI blood loss is quite common with usual dosages of aspirin and stems from the drug's local effect on the GI mucosa. During chronic therapy, this type of bleeding may occasionally produce iron deficiency anemia. In contrast, major upper GI bleeding rarely occurs except in patients with active peptic ulcers or recent GI bleeding. However, these patients generally do not experience greater occult blood loss than healthy patients following small doses of aspirin. Mucosal damage associated with the use of salicylates may lead to development of peptic ulcers with or without bleeding, reactivation of latent ulcers, and ulcer perforation. Therapy with salicylates and related agents such as salicylamide should be considered and administered cautiously in patients with a history of GI disease or alcoholism, particularly if they are elderly and/or debilitated, since such patients may be more susceptible to the GI toxicity of these drugs and seem to tolerate ulceration and bleeding less well than other individuals. Extreme caution and thorough assessment of risks and benefits are warranted in patients with active or recent GI bleeding or lesions. Whenever possible, especially if prolonged use is anticipated, treatment with non-ulcerogenic agents should be attempted first. If salicylates are used, close monitoring for toxicity is recommended. Some adverse GI effects may be minimized by administration with high dosages of antacids, use of enteric-coated or extended-release formulations, and/or concurrent use of a histamine H2-receptor antagonist or a cytoprotective agent such as misoprostol. Patients with active peptic ulceration or GI bleeding treated with salicylates should generally be administered a concomitant anti-ulcer regimen.
Salicylates (applies to aspirin/omeprazole) renal dysfunction
Major Potential Hazard, High plausibility.
Salicylate and its metabolites are eliminated almost entirely by the kidney. Therapy with salicylate drugs should be administered cautiously in patients with renal impairment, especially if it is severe. Reduced dosages may be necessary to avoid drug accumulation. Clinical monitoring of renal function is recommended during prolonged therapy, since the use of salicylate drugs has rarely been associated with renal toxicities, including elevations in serum creatinine, renal papillary necrosis, and acute tubular necrosis with renal failure. Most of the data have been derived from experience with aspirin but may apply to other salicylates as well. In patients with impaired renal function, aspirin has caused reversible and sometimes marked decreases in renal blood flow and glomerular filtration rate. Adverse renal effects have usually reversed rapidly following withdrawal of aspirin therapy.
Salicylates (applies to aspirin/omeprazole) Reye's syndrome
Major Potential Hazard, High plausibility. Applicable conditions: Influenza, Varicella-Zoster
The use of salicylates, primarily aspirin, in children with varicella infections or influenza-like illnesses has been associated with an increased risk of Reye's syndrome. Although a causal relationship has not been established, the majority of evidence to date seems to support the association. Most authorities, including the American Academy of Pediatrics Committee on Infectious Diseases, recommend avoiding the use of salicylates in children and teenagers with known or suspected varicella or influenza and during presumed outbreaks of influenza. If antipyretic or analgesic therapy is indicated under these circumstances, acetaminophen may be an appropriate alternative. The same precautions should also be observed with related agents such as salicylamide or diflunisal because of their structural and pharmacological similarities to salicylate.
Proton pump inhibitors (applies to aspirin/omeprazole) bone fractures
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Osteoporosis
Various published observational studies have reported that PPI therapy may be associated with an increased risk for osteoporosis related fractures of the hip, wrist or spine. The risk was increased in patients who received high doses (multiple daily doses), and long term treatment (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Caution should be used in patients at risk for osteoporosis related fractures and should be managed according to established treatment guidelines.
Proton pump inhibitors (applies to aspirin/omeprazole) hypomagnesemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Magnesium Imbalance
Symptomatic and asymptomatic hypomagnesemia has been reported rarely in patients treated with PPIs for at least 3 months, in most cases after a year of therapy. Serious adverse events can include tetany, seizures, and arrhythmias. Caution should be used in patients prone to magnesium imbalances such as patients taking other medications that can cause hypomagnesemia (e.g., diuretics). Regular monitoring is recommended.
Salicylates (applies to aspirin/omeprazole) anemia
Moderate Potential Hazard, Moderate plausibility.
Occult, often asymptomatic GI blood loss occurs quite frequently with the use of normal dosages of aspirin and stems from the drug's local effect on the GI mucosa. During chronic therapy, this type of bleeding may occasionally produce iron deficiency anemia. Other salicylates reportedly cause little or no GI blood loss at usual dosages, but may do so at high dosages. Prolonged therapy with salicylates, particularly aspirin, should be administered cautiously in patients with or predisposed to anemia. Periodic monitoring of hematocrit is recommended. The same precautions should also be observed with the use of related agents such as salicylamide because of their structural and pharmacological similarities to salicylate.
Salicylates (applies to aspirin/omeprazole) dialysis
Moderate Potential Hazard, High plausibility. Applicable conditions: hemodialysis
Salicylate and its metabolites are readily removed by hemodialysis and, to a lesser extent, by peritoneal dialysis. Doses should either be scheduled for administration after dialysis or supplemental doses be given after dialysis.
Salicylates (applies to aspirin/omeprazole) G-6-PD deficiency
Moderate Potential Hazard, Moderate plausibility.
Salicylates, particularly aspirin, may cause or aggravate hemolysis in patients with pyruvate kinase or glucose-6-phosphate dehydrogenase (G-6-PD) deficiency. However, this effect has not been clearly established. Until more data are available, therapy with salicylates should be administered cautiously in patients with G-6-PD deficiency. The same precaution should also be observed with the use of related agents such as salicylamide because of their structural and pharmacological similarities to salicylate.
Salicylates (applies to aspirin/omeprazole) hepatotoxicity
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
The use of salicylates has occasionally been associated with acute, reversible hepatotoxicity, primarily manifested as elevations of serum transaminases, alkaline phosphatase and/or, rarely, bilirubin. Hepatic injury consistent with chronic active hepatitis has also been reported in a few patients, which resulted rarely in encephalopathy or death. Salicylate-induced hepatotoxicity appears to be dependent on serum salicylate concentration (> 25 mg/dL) and has occurred most frequently in patients with juvenile arthritis, active systemic lupus erythematosus, rheumatic fever, or preexisting hepatic impairment. Therapy with salicylates, particularly when given in high dosages, should be administered cautiously in these patients, and periodic monitoring of liver function is recommended. The same precautions should also be observed with the use of related agents such as salicylamide because of their structural and pharmacological similarities to salicylate. A dosage reduction may be necessary if liver function abnormalities develop and serum salicylate concentration exceeds 25 mg/dL, although serum transaminase elevations may sometimes be transient and return to pretreatment values despite continued therapy without dosage adjustment.
Switch to professional interaction data
Aspirin/omeprazole drug interactions
There are 547 drug interactions with aspirin / omeprazole.
Aspirin/omeprazole alcohol/food interactions
There are 2 alcohol/food interactions with aspirin / omeprazole.
More about aspirin / omeprazole
- aspirin/omeprazole consumer information
- Check interactions
- Compare alternatives
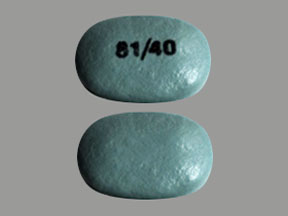
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: platelet aggregation inhibitors
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.