Uterine Tissue Removal
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
Uterine tissue removal
is a procedure used to remove fibroids and polyps from inside your uterus. This may help reduce heavy bleeding during your monthly periods. You may still have normal periods and become pregnant after this procedure.
 |
How to prepare for your procedure:
- The procedure will be done at a hospital, your healthcare provider's office, or an outpatient facility. Your provider will talk to you about how to prepare. You may be told not to eat or drink anything after midnight on the day of your procedure. Arrange for someone to drive you home after your procedure.
- You may need to stop taking blood thinners or aspirin several days before your procedure. This will help decrease your risk for bleeding. Your provider will tell you what medicines to take or not take on the day of your procedure. You may be given an antibiotic to prevent infection. Tell healthcare providers if you have ever had an allergic reaction to an antibiotic.
What will happen during your procedure:
- General or local anesthesia may be used for this procedure. General anesthesia means you will be asleep during the procedure. Local anesthesia means you will be awake and may feel pressure or pushing, but you should not feel pain.
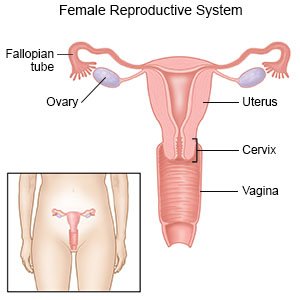
- Your healthcare provider will gently insert a device into your vagina. The device opens the walls of your vagina so your provider can see your cervix. Tools or liquid will be used to open your cervix. Your provider will guide a camera through your cervix and into your uterus. The camera will allow your provider to see inside your uterus to find the fibroid or polyp.
- Your provider will guide a thin wand through your vagina and into your uterus. One side of the wand is made to cut the fibroid or polyp into pieces. Suction is used to pull the small pieces into the wand to remove them from your uterus. When all the pieces have been removed, the wand will be removed.
What to expect after your procedure:
You may have mild lower abdominal cramping after the procedure. This should last 1 to 2 days. Your healthcare provider may tell you to take acetaminophen or an NSAID pain medicine, such as ibuprofen. You may be able to go home the same day. Plan to rest when you get home. You can return to your regular activities within 2 days or as directed.
Risks of this procedure:
You may bleed more than expected or get an infection. Your uterus may be torn, or your cervix may be damaged. You may get fibroids or polyps again, even if your treatment is successful. Scar tissue may form in your uterus. You may have fluid overload. This means your body absorbs too much fluid produced during the procedure. Your provider will have to stop the procedure if this happens.
Related medications
Seek care immediately if:
- You have shortness of breath or feel dizzy.
- You have heavy bleeding from your vagina that soaks more than 1 sanitary pad every hour.
- You have abdominal cramps for more than 2 days.
- You have severe pain that does not get better even after you take pain medicine.
- You have trouble urinating or having a bowel movement.
Call your doctor if:
- You have nausea or are vomiting.
- You have a fever higher than 100.4°F (38°C).
- You have a green or foul-smelling vaginal discharge.
- You do not get your monthly period.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Return to your regular activities as directed:
Your healthcare provider will tell you when it is safe to soak in a bath or hot tub. Your provider will also tell you when it is safe to use tampons or have sex. It is important to follow all instructions to prevent an infection.
Self-care:
- Rest as needed. You may have mild lower abdominal cramps or feel tired.
- Apply heat on your abdomen for 20 to 30 minutes every 2 hours, or as directed. Heat helps relieve cramps.
- Keep a record of your monthly periods. Record the day your period starts and stops each month. Also record if you have a lighter flow than before the procedure. The first few months may vary. It may take 3 months for your period to return to normal. Bring your record with you to follow-up visits with your healthcare provider.
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
