Total Hip Replacement
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about total hip replacement (THR):
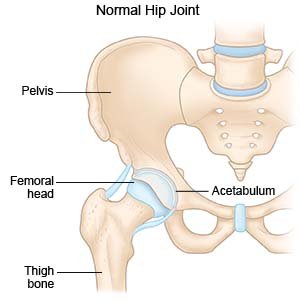
THR, or total hip arthroplasty, is surgery to replace all or part of your hip joint. The hip joint is where the top of your femur (thigh bone) sits in the socket of your pelvic bone. The joint is held together by ligaments and muscles. The top of your femur is shaped like a ball and covered with cartilage. Cartilage is a tissue that helps joints move.
 |
How to prepare for THR:
- Your surgeon will tell you how to prepare. Your surgeon may tell you not to eat or drink anything after midnight on the day of your surgery. Arrange to have someone drive you home when you are discharged.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for the surgery, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about any allergies you have, including anesthesia or medicines. You may be given an antibiotic to help prevent a bacterial infection.
- Your surgeon will tell you if you need any tests before your surgery, and when to have them.
- You may need blood and urine tests before your surgery. These tests show how well your kidneys are functioning and your blood is clotting. You may also need x-rays or an ultrasound.
What will happen during THR:
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given spinal, or regional, anesthesia. This type will numb you from the waist down. You may still feel pressure or pushing, but you should not feel any pain.
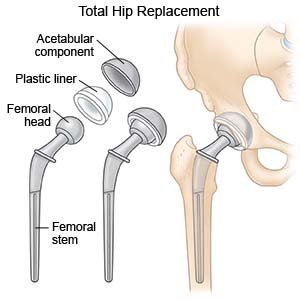
- Your surgeon will make an incision over your hip. The top, or head, of the femur will be removed and a metal stem will be placed into the middle of your leg bone. A metal or ceramic ball will be placed on the upper part of the stem. This ball replaces the damaged bone that was removed.
- The damaged cartilage of your hip socket will be removed and replaced with a metal socket or porous surface. The porous surface allows your bone to grow and fill the pores of the implant. Medical cement or screws may be placed to secure the implant parts. A metal, ceramic, or plastic spacer will be placed between the ball and socket. This creates a smooth surface for the parts to move smoothly against each other.
- The incision will be closed with stitches or staples. You may have a bandage covering the area.
 |
What to expect after THR:
You may have increased pain or stiffness after surgery. This will get better with movement and exercise. Providers will teach you how to sit up and move without damaging your hip. A physical therapist will help you get up and walk after surgery. You may need a walker.
Risks of THR:
You may bleed more than expected or develop an infection. One leg may feel longer or shorter than the other. Your nerves, blood vessels, ligaments, or muscles may be damaged during surgery. Your implant may become loose or move out of place. If this happens, you may need another surgery to replace the implant. You may get a blood clot in your limb. This may become life-threatening.
Call your local emergency number (911 in the US) or have someone call if:
- You have chest pain when you take a deep breath or cough. You may cough up blood.
- You suddenly feel lightheaded and short of breath.
- You have a seizure or feel confused.
Related medications
Seek care immediately if:
- Your leg feels warm, tender, and painful. It may look swollen and red.
- Your incision comes apart.
- You urinate less than usual or not at all.
Call your doctor or surgeon if:
- You have a fever or chills.
- Your wound is red, swollen, or draining pus.
- Blood soaks through your bandage.
- You have nausea or are vomiting.
- You have more pain and swelling in your hip joint, even after you take pain medicine.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for the area as directed:
You may have stitches or staples. These may be removed in about 2 weeks. Do not get the area wet until it is completely healed. Ask your healthcare provider when it is okay to get the area wet. Change your bandage as directed and if it gets wet or dirty.
Self-care:
- Apply ice on your hip for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel. Ice helps prevent tissue damage and decreases swelling and pain.
- Use assistive devices as directed. Examples include a raised toilet seat, a shower bench, and a reacher. You may also need a cane, crutches, or a walker. These devices will help with your daily activities until your strength and balance improves.
- Go to physical therapy. A physical therapist teaches you exercises to help improve movement and strength, and to decrease pain.
Prevent dislocation of your hip implant:
Do the following for up to 8 weeks after your hip replacement:
- Sit in a straight-backed chair. Use armrests to help you rise from a seated position. Do not sit on low chairs, sofas, rocking chairs, or stools.
- Do not lean forward to put on pants, socks, or shoes. Do not lean forward or twist to pick items up. Use assistive devices to put on socks and shoes.
- Keep your knees apart. Do not cross your legs. You may need to put a pillow between your knees to remind you.
Follow up with your doctor or surgeon as directed:
You may need to have your stitches or staples removed. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Total Hip Replacement
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
