Heart Failure
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
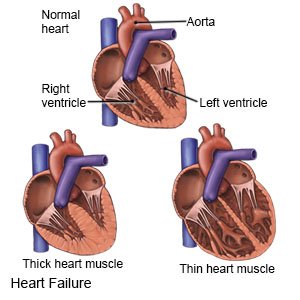
Heart failure
is a condition that does not allow your heart to fill or pump properly. Not enough oxygen in your blood gets to your organs and tissues. Fluid may not move through your body properly. Fluid may build up and cause swelling and trouble breathing. This is known as congestive heart failure. It is important to manage your health to improve your quality of life.
 |
Signs and symptoms
depend on the type of heart failure you have and how severe it is. You may have any of the following:
- Trouble breathing with activity that worsens to trouble breathing at rest
- Shortness of breath while lying flat
- Severe shortness of breath and coughing at night that usually wakes you
- Feeling lightheaded when you stand up
- Purple color around your mouth and nails
- Confusion or anxiety
- Chest pain at night
- Periods of no breathing, then breathing fast
- Lack of energy (often worsened by physical activity), or trouble sleeping
- Swelling in your ankles, legs, or abdomen
- Heartbeat that is fast or not regular
- Fingers and toes feel cool to the touch
Call your local emergency number (911 in the US) if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
Seek immediate care if:
- Your heartbeat is fast, slow, or uneven all the time.
Call your doctor if:
- You have symptoms of worsening heart failure:
- Shortness of breath at rest, at night, or that is getting worse in any way
- Weight gain of 3 or more pounds (1.4 kg) in a day, or more than your healthcare provider says is okay
- More swelling in your legs or ankles
- Abdominal pain or swelling
- More coughing
- Loss of appetite
- Feeling tired all the time
- You feel depressed, or you have lost interest in things you used to enjoy.
- You often feel worried or afraid.
- You have questions or concerns about your condition or care.
Related medications
Treatment:
Heart failure is often caused by damage or injury to your heart. The damage may be caused by other heart problems, diabetes, or high blood pressure. The damage may have also been caused by an infection. Your healthcare providers will help you manage any other health conditions that may be causing your heart failure. The goals of treatment are to manage, slow, or reverse heart damage. Treatment may include any of the following:
- Medicines may be needed to help regulate your heart rhythm. You may also need medicines to lower your blood pressure, and to decrease extra fluids.
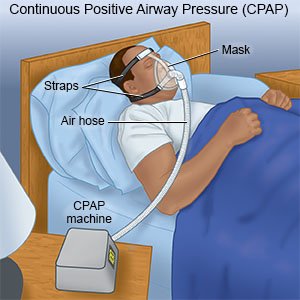
- Oxygen may help you breathe easier if your oxygen level is lower than normal. A CPAP machine may be used to keep your airway open while you sleep.
- Cardiac rehab is a program run by specialists who will help you safely strengthen your heart. In the program you will learn about exercise, relaxation, stress management, and heart-healthy nutrition. Cardiac rehab may be recommended if your heart failure is not severe.
- Surgery can be done to implant a pacemaker or another device in your chest to regulate your heart rhythm. Other types of surgery can open blocked heart vessels, replace a damaged heart valve, or remove scar tissue.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Manage swelling from extra fluid:
- Elevate (raise) your legs above the level of your heart. This will help with fluid that builds up in your legs or ankles. Elevate your legs as often as possible during the day. Prop your legs on pillows or blankets to keep them elevated comfortably. Try not to stand for long periods of time during the day. Move around to keep your blood circulating.

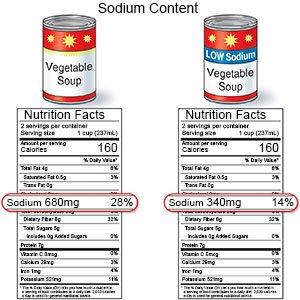
- Limit sodium (salt). Ask how much sodium you can have each day. Your healthcare provider may give you a limit, such as 2,300 milligrams (mg) a day. Your provider or a dietitian can teach you how to read food labels for the number of mg in a food. He or she can also help you find ways to have less salt. For example, if you add salt to food as you cook, do not add more at the table.
- Drink liquids as directed. You may need to limit the amount of liquid you drink within 24 hours. Your healthcare provider will tell you how much liquid to have and which liquids are best for you. He or she may tell you to limit liquid to 1.5 to 2 liters in a day. He or she will also tell you how often to drink liquid throughout the day.
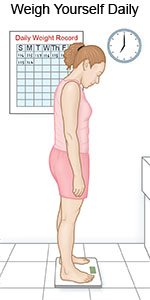
- Weigh yourself every morning. Use the same scale, in the same spot. Do this after you use the bathroom, but before you eat or drink. Wear the same type of clothing each time. Write down your weight and call your healthcare provider if you have a sudden weight gain. Swelling and weight gain are signs of fluid buildup.
Manage heart failure:
Your quality of life may improve with treatment and the following:
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung and heart damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Do not drink alcohol or use illegal drugs. Alcohol and drugs can increase your risk for high blood pressure, diabetes, and coronary artery disease.
- Eat heart-healthy foods. Heart-healthy foods include fruits, vegetables, lean meat (such as beef, chicken, or pork), and low-fat dairy products. Fatty fish such as salmon and tuna are also heart healthy. Other heart-healthy foods include walnuts, whole-grain breads, and legumes such as pinto beans. Replace butter and margarine with heart-healthy oils such as olive oil or canola oil. Your provider or a dietitian can help you create heart-healthy meal plans.

- Manage any chronic health conditions you have. These include high blood pressure, diabetes, obesity, high cholesterol, metabolic syndrome, and COPD. You will have fewer symptoms if you manage these health conditions. Follow your healthcare provider's recommendations and follow up with him or her regularly.
- Maintain a healthy weight. Being overweight can increase your risk for high blood pressure, diabetes, and coronary artery disease. These conditions can make your symptoms worse. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a weight loss plan, if needed.
- Stay active. Activity can help keep your symptoms from getting worse. Walking is a type of physical activity that helps maintain your strength and improve your mood. Physical activity also helps you manage your weight. Work with your healthcare provider to create an exercise plan that is right for you.
- Get vaccines as directed. The flu, COVID-19, and pneumonia can be severe for a person who has heart failure. Vaccines protect you from these infections. Your provider can tell you if you should also get vaccines not listed below:
- Ask your healthcare provider about the flu and pneumonia vaccines. All adults should get the flu (influenza) vaccine as soon as recommended each year, usually in September or October. The pneumonia vaccine is recommended for all adults aged 50 or older to prevent pneumococcal disease, such as pneumonia. Adults aged 19 to 49 years who are at high risk for pneumococcal disease should also receive the vaccine. You may need 1 dose or 2. The number depends on the vaccine used and your risk factors.
- COVID-19 vaccines are given to adults as a shot. At least 1 dose of an updated vaccine is recommended for all adults. COVID-19 vaccines are updated throughout the year. Adults 65 or older need a second dose of updated vaccine at least 4 months after the first dose. Your healthcare provider can help you schedule all needed doses as updated vaccines become available.
 |
Follow up with your doctor or cardiologist within 7 days or as directed:
You may need to return for other tests. You may need home health care. A healthcare provider will monitor your vital signs, weight, and make sure your medicines are working. Write down your questions so you remember to ask them during your visits.
For support or more information:
Heart failure can be difficult to manage. It may be helpful to talk with others who have heart failure. You may learn how to better manage your condition or get emotional support. For more information:
- American Heart Association
7272 Greenville Avenue
Dallas , TX 75231-4596
Phone: 1- 800 - 242-8721
Web Address: http://www.heart.org
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Heart Failure
Treatment options
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
