Coronary Intravascular Stent Placement
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about coronary intravascular stent placement:
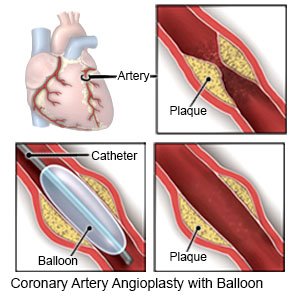
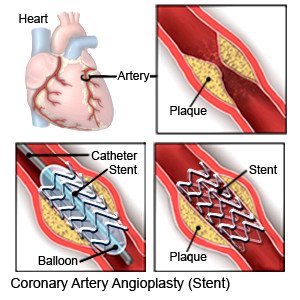
Coronary intravascular stent placement is a procedure to place a stent in an artery of your heart that has plaque buildup. Plaque is a mixture of fat and cholesterol. A stent is a small mesh tube made of metal that helps keep your artery open. The stent remains in your artery for life. You may need more than one stent.
How to prepare for your procedure:
- Your healthcare provider will tell you how to prepare for your procedure. Your provider may tell you not to eat or drink anything after midnight on the day of your procedure. Arrange to have someone drive you home when you leave the hospital.
- Tell your provider about all your current medicines. Your provider will tell you if you need to stop any medicine for the procedure and when to stop. Your provider will tell you which medicines to take or not take on the day of your procedure.
- You may be given an antibiotic to help prevent a bacterial infection. Contrast liquid may be used during your procedure. Tell a healthcare provider if you have ever had an allergic reaction to antibiotics or contrast liquid.
- You may need blood tests and a stress test before your procedure. Talk to your provider about these or other tests you may need.
What will happen during the procedure:
- You may be given an antibiotic through your IV to help prevent a bacterial infection. You will be given medicine in your IV to help you relax or make you drowsy. You will also get local anesthesia that will numb the area where the catheter will be placed (catheter site). You will be awake during the procedure so healthcare providers can give you instructions. You may be asked to cough, hold your breath, or to tell them how you feel during the procedure.
- A catheter (long, thin tube) will be put into an artery in your wrist, groin, or neck. The catheter will be gently guided through this artery to your heart and into the narrowed or blocked artery. Healthcare providers will use x-rays and contrast liquid to find the area where the stent needs to be placed. You may feel warm as the contrast liquid is put into the catheter. This feeling should go away quickly.
- A guidewire will then be placed into the catheter. The balloon catheter will be guided into the narrowed or blocked artery with the guidewire. Healthcare providers will inflate the balloon several times for short periods. The inflated balloon pushes the plaque against the artery walls. This opens them and allows more blood flow to your heart. Another balloon catheter with a stent is then inserted into the artery. The balloon is inflated. This expands the stent and pushes it into place against the artery wall.
- Your healthcare provider may place a bare metal stent or a drug-eluting stent (DES) in your artery. A DES is coated with medicine that is slowly released. The medicine helps prevent more plaque buildup. The stent will be left in your artery to help keep it open.
- The catheter and guidewire will be taken out of the artery and a pressure bandage will be put on the catheter site. Your provider may apply a collagen plug or other closure device to stop the bleeding. Healthcare providers will put pressure on the bandaged area to help stop the bleeding.
What to expect after the procedure:
- You will be taken to a room to rest. Healthcare providers will monitor you closely for any problems. You will then be taken to your hospital room.
- You may need to lie still for 3 to 6 hours after the procedure to prevent bleeding. Do not get out of bed until your healthcare provider says it is okay. If you need to cough, use your hand to apply pressure to the catheter site.
Risks of the procedure:
- You may develop a hematoma (swelling caused by collection of blood). You may bleed more than expected from your catheter site. The contrast liquid used during this procedure may cause an allergic reaction or kidney problems. You may develop an infection.
- Your artery may be injured when the catheter is inserted. During or after your procedure, blood clots may form, or plaque may break off. The blood clot or plaque may block your artery and cause a heart attack or stroke. The stent could collapse, or a clot could form on the stent. This could cause the artery to become blocked again. You may need another procedure to open your artery.
Call your local emergency number (911 in the US) for any of the following:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- Your leg or arm becomes numb, or your fingers or toes turn white or blue.
- The catheter site is swollen, red, or has pus or foul-smelling fluid coming from it.
- You start to bleed from your catheter site again.
Call your cardiologist or doctor if:
- You have a fever or chills.
- You have questions or concerns about your condition or care.
Related medications
Medicines:
You may need any of the following:
- Antiplatelets prevent blood clots from forming. You will need to take aspirin and another type of antiplatelet medicine. Take this medicine daily as directed. Do not stop taking aspirin or other type of antiplatelet medicine without asking your healthcare provider.
- Cholesterol medicine helps decrease the amount of cholesterol in your blood. Too much cholesterol in your blood may cause plaque buildup.
- Blood pressure medicine lowers your blood pressure.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Apply firm, steady pressure if bleeding continues:
A small amount of bleeding from the catheter site is possible. Apply pressure with a clean gauze or towel for 5 to 10 minutes. Call your local emergency number (911 in the US) if bleeding becomes heavy or does not stop.
Care for the catheter site:
Most bandages can be removed the day after your procedure. Gently clean the catheter site with soap and water. Do not rub the site. Do not take a bath, swim, or get in a hot tub until your healthcare provider says these are okay. If you need to cough, support the catheter site with your hand.
Activity:
Rest for 1 or 2 days after your procedure. Slowly start to do more each day. Take walks around your house. Make a plan for rest during the day. Your provider will tell you when you can drive, go back to work, or do other activities. Activity limits help reduce pressure on your catheter site and prevent bleeding. The following limits depend on the catheter site:
- Wrist: Follow these guidelines for 1 week , or as directed.
- Do not lift anything heavier than 2 pounds.
- Do not push or pull with the arm used for the procedure.
- Avoid activities that use your arm or wrist, such as tennis, bowling, and golf.
- Groin: Follow these guidelines for as long as shown below, or as directed.
- Do not have sex for 2 days.
- Do not lift anything heavier than 5 pounds for 1 week.
- Limit stair climbing for 1 week.
- Avoid intense exercise for 2 to 4 weeks.
Drink liquids as directed:
Drink extra liquids if contrast liquid was used during your procedure. Liquid will help flush the contrast out of your body. Ask your healthcare provider how much liquid to drink each day and which liquids are best for you. Do not drink alcohol for at least 24 hours after your procedure.
Do not smoke:
Nicotine and other chemicals in cigarettes and cigars can cause heart damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Go to cardiac rehabilitation (rehab), if directed:
Your cardiologist may recommend that you attend cardiac rehab. This is a program run by specialists who will help you safely strengthen your heart and reduce the risk for more heart disease. The plan includes exercise, relaxation, stress management, and heart-healthy nutrition. Healthcare providers will also check to make sure any medicines you are taking are working.
Stent safety:
- Carry your stent card with you at all times.
- Let all healthcare providers know that you have a stent.
- If you need an MRI, wait at least 6 to 8 weeks after stent placement, or as directed.
Follow up with your cardiologist or doctor as directed:
You may need more tests. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Coronary Intravascular Stent Placement
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
